Chapter 5 Immunity
Immunity
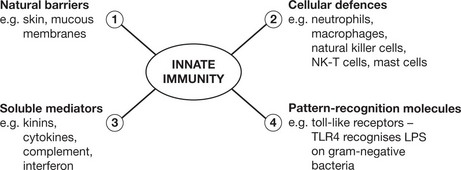
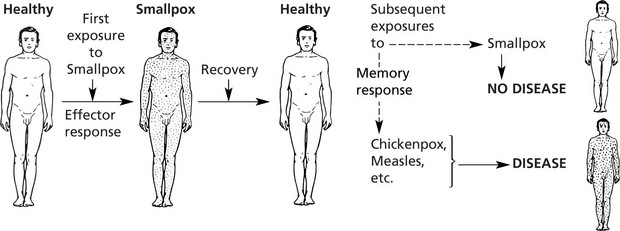
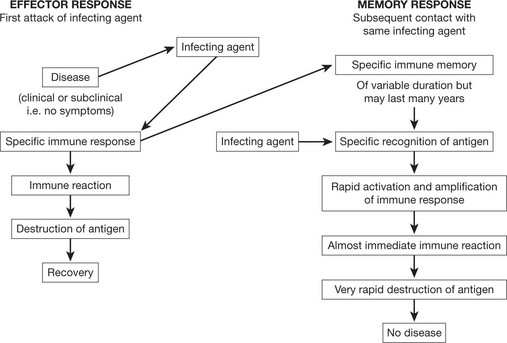
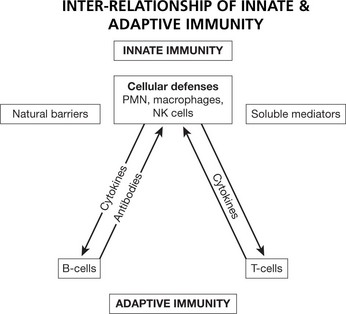
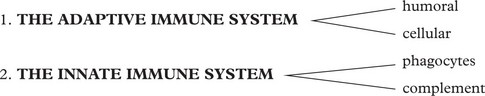
The immune system protects us from invading pathogenic microorganisms and cancer. Immunity – the state of protection from infectious disease – has both a less specific or INNATE and a more specific or ADAPTIVE component.
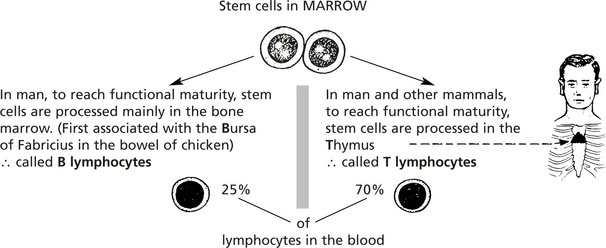
Cellular Basis of the Adaptive Immune Response
The main cells of the adaptive immune response are the lymphocytes. They are indistinguishable by light microscopy using conventional stains but can be separated by the presence of different surface proteins on T and B cells.
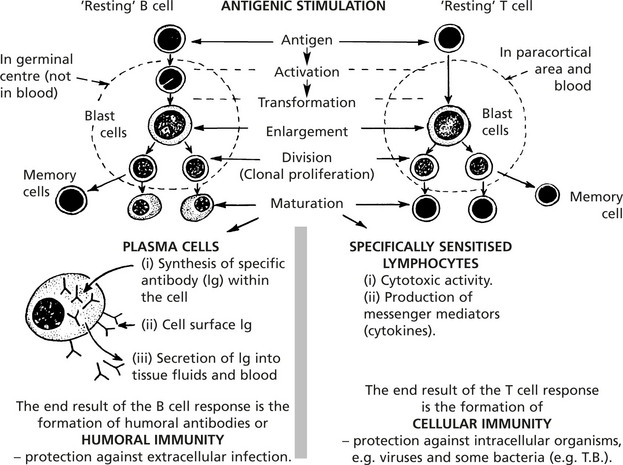
Genetic Influences on the Immune Response
The major histocompatibility complex, also known as the human leucocyte antigen (HLA), has an important role in the immune response and disease.
The important roles of HLA are:
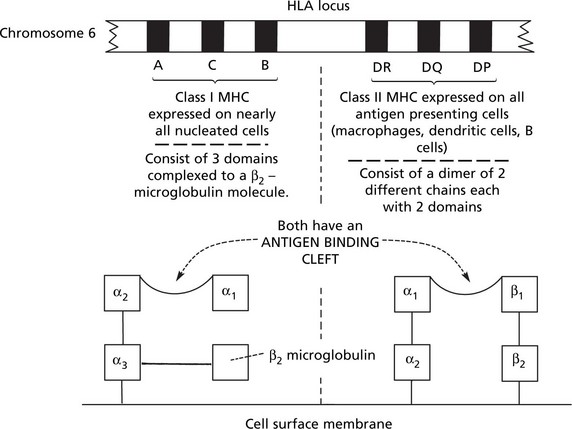
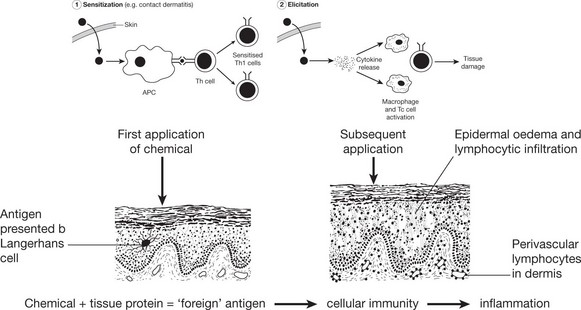
Cellular Immunity
Activation of T cells requires the involvement of antigen presenting cells. Within these cells, foreign antigen is proteolytically digested to short peptides and then presented with HLA molecules to the T cell which possesses a specific receptor for that antigen.
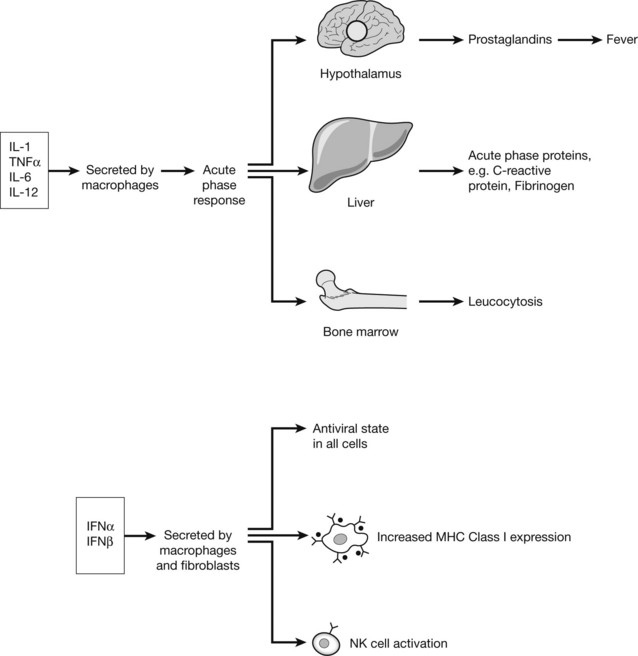
Cytokines
The chemical messengers of immune system are known as CYTOKINES. These small proteins are produced by virtually all cells of the innate and adaptive immune system, particularly CD4+ lymphocytes. The quantity and type of cytokine can positively and negatively regulate cells and cytokine effect is in turn controlled by expression or down-regulation of cytokine receptors on the cell surface.
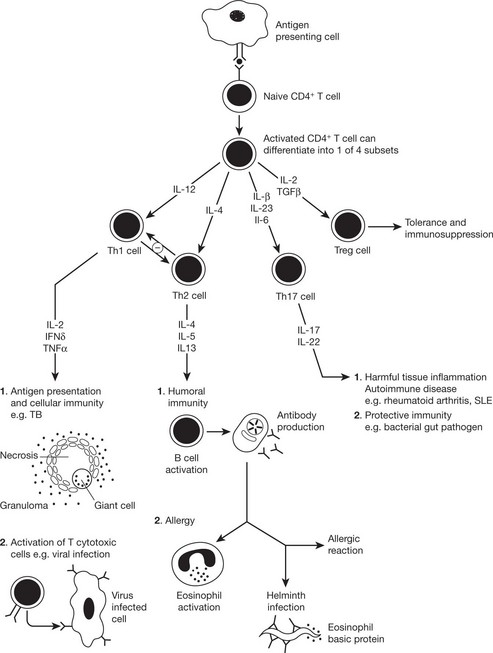
Cytokines Involved in Adaptive Immunity
The immune response to a particular pathogen must induce an appropriate set of effector functions that can eliminate the pathogen from the host. Differences in cytokine secretion patterns among T helper cells are determinants of the type of immune response made to a particular antigenic challenge. Accordingly the cytokines secreting T helper cells are currently divided into 4 subsets:
Humoral Immunity
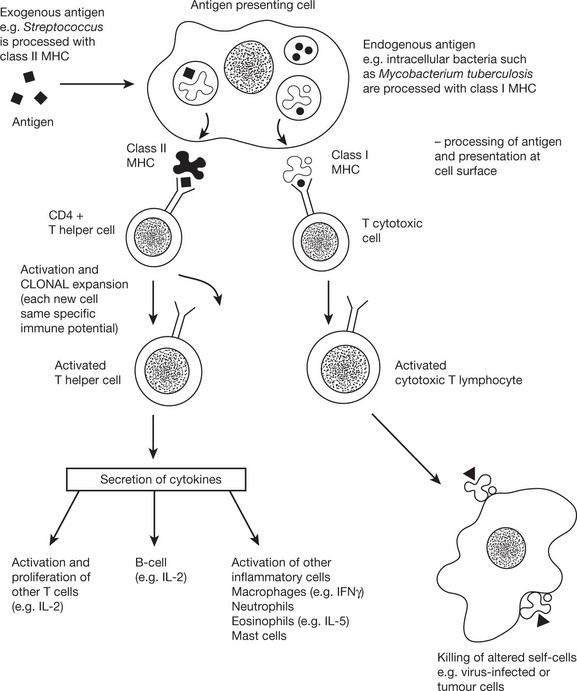
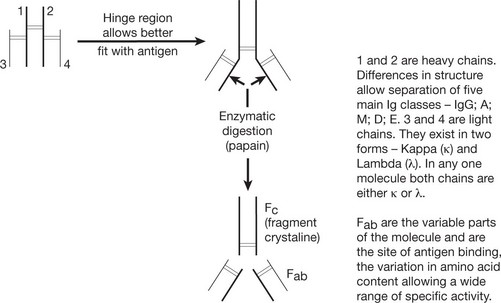
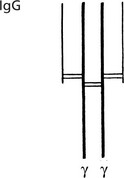
Basic Structure of Immunoglobulin
The basic immunoglobulin is a protein molecule consisting of 2 identical LIGHT chains and two identical HEAVY chains. Each light chain is bound to a heavy chain by a disulphide bond. Similarly disulphide bridges link the two heavy and light chain combinations to form the basic four chain structure.
Immunoglobulins
Antibody Classes and Activities
These groups are named according to the composition of the heavy chains.
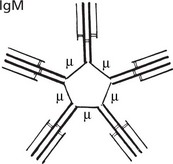
Note: The numerous (10) antigenbinding sites increase its efficiency.
The natural blood group antibodies, anti-A and anti-B are M globulins.
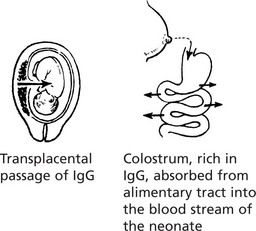
IgG (heavy chain = γ) is a single molecule with two antigen binding sites.
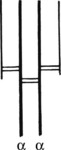
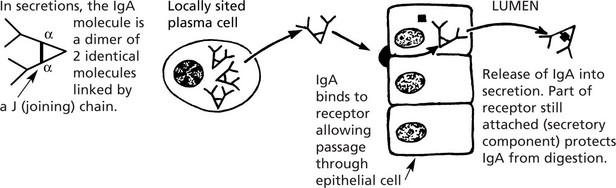
IgA (heavy chain = α) occurs in the blood (1.5–4 mg/ml) where its function is unknown.
The diagram illustrates the local production of IgA in the gut.
| IgD | (heavy chain Δ) of uncertain function: concentration in blood very low probably because it is not secreted by plasma cells. Like IgM it is present on the surface of B lymphocytes prior to transformation. |
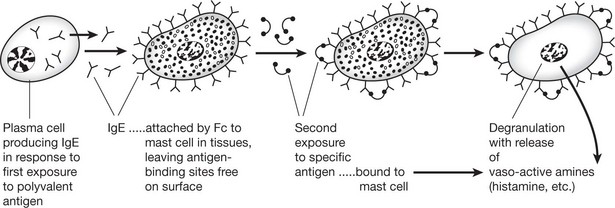
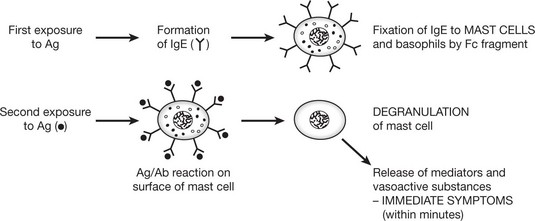
| IgE | (heavy chain ε) – a single molecule similar to IgG and IgA. It is sometimes called REAGIN: concentration in blood is low (20–500 ng/ml). The serum level is raised in worm infestation and is probably protective. Its main activity is mediated by MAST CELLS (or BASOPHILS); it is the principal mediator of atopic and anaphylactic disease. |
Immune Reactions
Antigen-Antibody Interactions
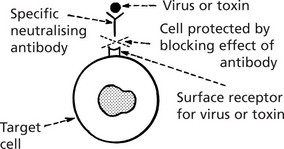
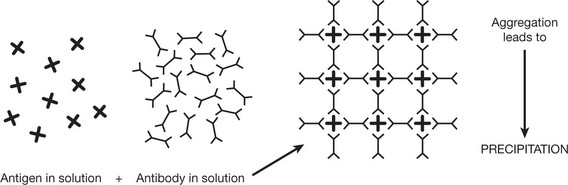
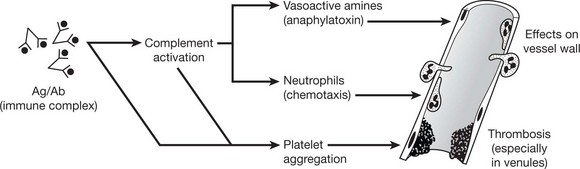
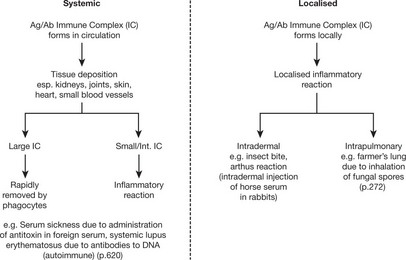
When an antigen (Ag) binds with an antibody (Ab) an Ag/Ab complex is formed. This reaction is reversible in varying degrees and depends on the affinity of the antibody for an individual antigen and the avidity (strength when multiple epitopes on an antigen interact with multiple binding sites).
The consequences of Ag/Ab interaction include:
A soluble antigen is rendered insoluble by aggregation of the Ag/Ab complexes into a lattice.
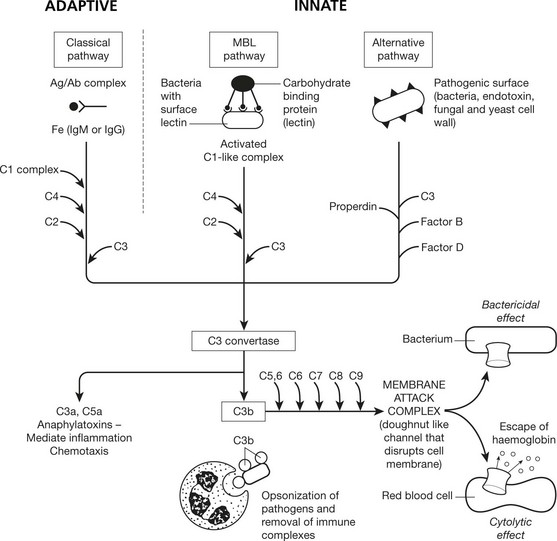
Complement System
Complement consists of nine main protein components present in inactive form in the blood. There are 3 pathways of complement activation. Activation results in the formation of multi-molecular enzymes that activate further components in a cascade ultimately generating a membrane attack complex that is capable of causing cell lysis.
E.g. Test serum + antigen + C.
If serum contains antibody, C is fixed, otherwise it remains free.
Add sensitised RBC (coated with Ab).
Lysis of RBC = complement still free ∴ no Ab in original serum.
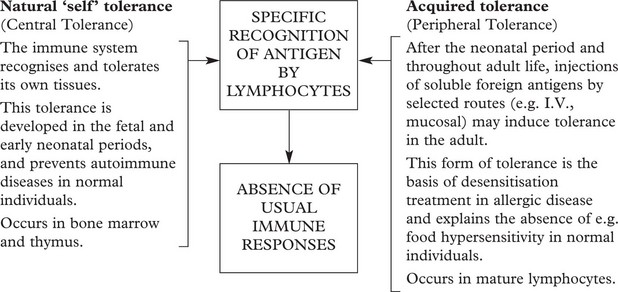
Tolerance
Humoral and cell-mediated immunity are specific active immune responses with a protective function.
Immunopathology
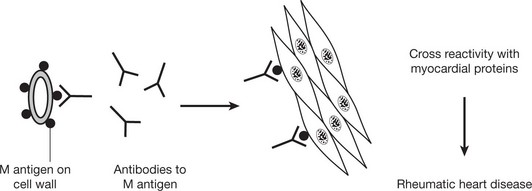
The complicated and delicately balanced immune mechanisms clearly have been developed to protect against antigens, particularly infections. When these immune reactions are upset, the protective mechanism can itself be a source of disease states.
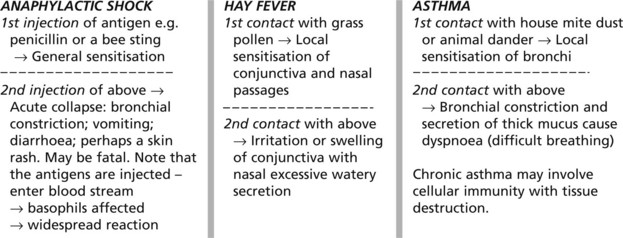
Hypersensitivity States
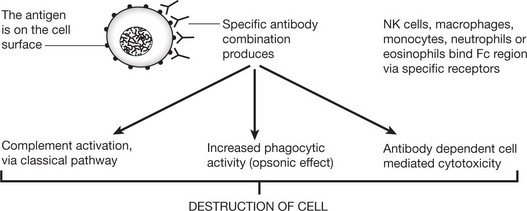
Type II – Cytotoxic Type
This cytotoxic reaction causes some forms of haemolytic anaemia (e.g. autoimmune HA (p.392): Rhesus incompatibility (p.393)) and some blood transfusion reactions. Certain drugs (e.g. penicillins) can also cause autoimmune HA by acting as a hapten. This is a small molecule that only becomes immunogenic when combined with a host protein carrier.
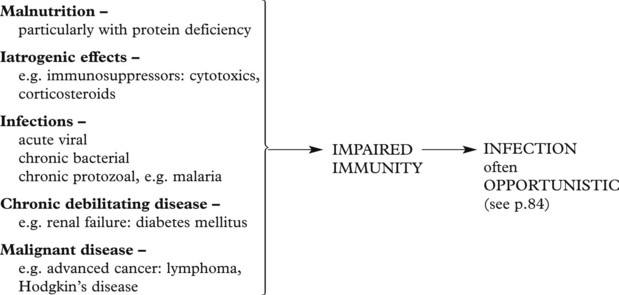
Immune Deficiency States
Deficiencies of the innate immune system are rare. The disorders of neutrophil function are described on page 408.
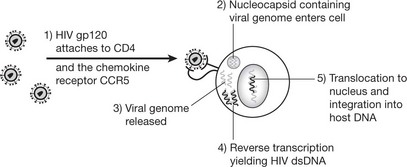
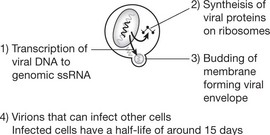
Immune Deficiency States – Aids
The acquired immune deficiency syndrome (AIDS) is a world-wide epidemic with large numbers of cases in sub-Saharan Africa and South East Asia. Globally, an estimated 40 million people are infected with the virus.
| Infection | Latent period | AIDS |
|---|---|---|
| CD4 > 500 × 106 | CD4 – 200–500 × 106 | CD4 < 200 × 106 |
| Asymptomatic or a short febrile illness. Although the patient’s cells contain HIV, tests for antibodies may be negative for up to several months. | Virus present in lymphocytes: may be persistent lymph node enlargement and fever. | Infections and tumours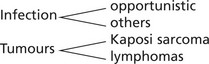 |
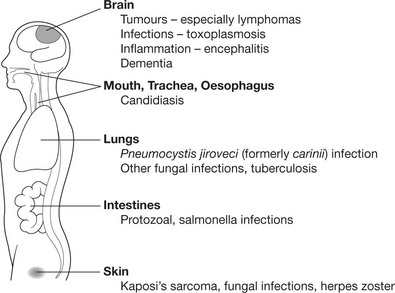
The whole range of opportunistic infection (see p.84), including disseminated virus infection (e.g. herpes simplex and cytomegalovirus), occurs.
The diagram shows the more common AIDS-associated diseases and sites:
Epidemiology and Transmission
Although the virus may be present in many body fluids and secretions, transmission is by the parenteral route, usually by 1. sexual contact, 2. infected blood or 3. from mother to infant.
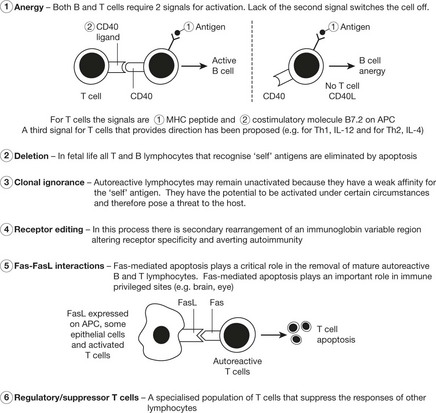
Autoimmune Diseases
Autoimmune diseases result from, or are associated with, an immune response against the individual’s own cells, or in some cases cell products. Although both humoral and cellular immunity are involved, it is thought that changes in the latter are of primary importance. In autoimmunity, something occurs to destroy integrity of self tolerance. The aetiology of autoimmunity is not fully established. Potential causes include:
Autoimmune diseases were traditionally classified as organ specific and non-organ specific. However, since there is some crossover between these two groups, they can be classified by the predominant effector mechanism leading to organ damage.
| Autoantigen | Target Organ | Disease |
|---|---|---|
| Red blood cells | Red blood cells | Haemolytic anaemia |
| Acetylcholine receptor | Voluntary muscle | Myasthenia gravis |
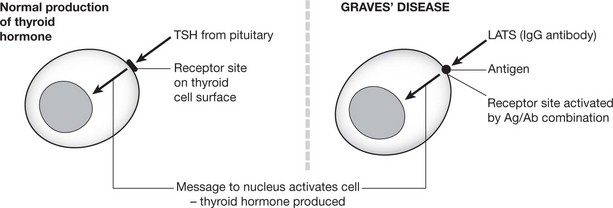
| TSH receptor | Thyroid | Graves’ disease |
| Nuclear constituents e.g. DNA, | Many – Kidney, skin, blood vessels, joint, heart | Systemic lupus erythematosus |
PREDOMINANTLY T CELL MEDIATED AUTOIMMUNE DISEASE
| Autoantigen | Target Organ | Disease |
|---|---|---|
| Myelin basic protein | Central nervous system | Multiple sclerosis |
| β-islet cells | Pancreas | Type 1 insulin dependent diabetes mellitus |
| Thyroglobulin Microsomal antigens Thyroid peroxidase |
Thyroid | Hashimoto’s thyroiditis |
| IgG | Synovium/joints | Rheumatoid arthritis |
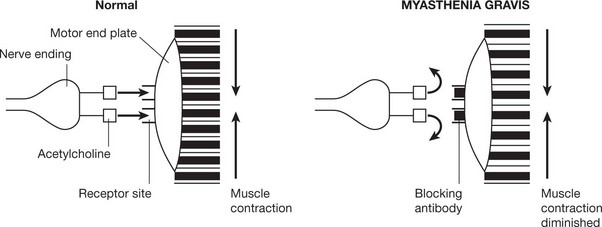
Primary thyrotoxicosis (Graves’ disease) and myasthenia gravis are of particular interest. In these diseases specific autoimmune antibodies combine with antigen on the cell surface and either stimulate or block the action of the physiological agent which would normally turn on the activity of the cell.
Applied Immunology
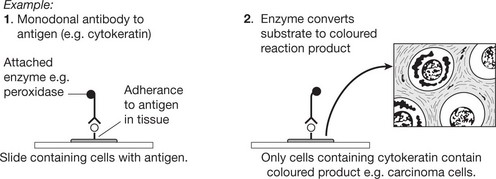
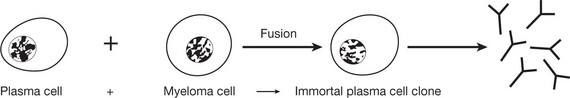
Immunohistochemical Identification
Immunohistochemistry is now well established and allows identification of specific substances in histological sections.
Prophylaxis and Treatment of Infections
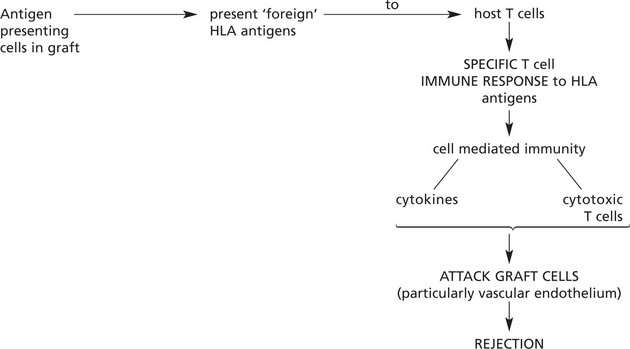
Applied Immunology – Tissue Transplantation
In the past, allografting (transplanting of tissues or organs from one individual to another of the same species) inevitably led to rejection of the graft by the host. Understanding of the mechanisms has allowed intervention so that nowadays successful survival of grafts is usual (e.g. 90% survival of renal transplants after 1 year).
Usually rejection takes weeks while the cell mediated immune response is building up.
The remarkable improvement in transplant prognosis is due to: