53 Ilioinguinal Nerve Block
The lower abdominal wall is primarily supplied by the subcostal, iliohypogastric, ilioinguinal, and genitofemoral nerves. The last three nerves arise from the lumbar plexus. Blocks of the ilioinguinal nerve are often performed to provide postoperative pain relief from inguinal hernia repair or for selective diagnostic purposes. Because transversus abdominis plane (TAP) blocks often fail to provide analgesia in the L1 distribution, ilioinguinal blocks may be of greater benefit for inguinal surgical procedures.1
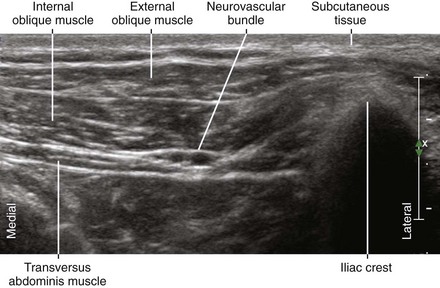
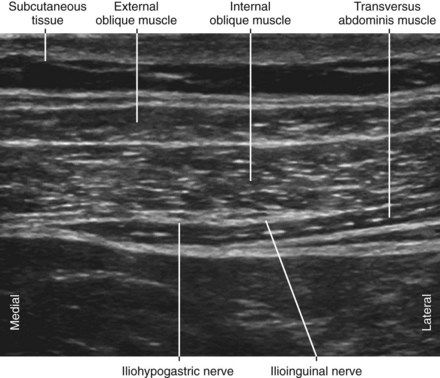
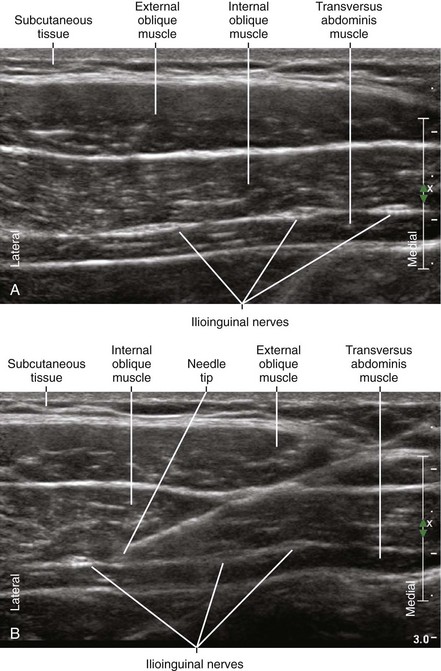
The ilioinguinal nerve emerges between the muscles of the abdominal wall. The longest running course of the nerve is between the internal oblique and transversus muscles. The iliohypogastric nerve has a parallel course to the ilioinguinal nerve, running cephalad (superior) and medial. Of the three abdominal wall muscles (external oblique, internal oblique, and transversus), the internal oblique is usually the thickest.2
Suggested Technique
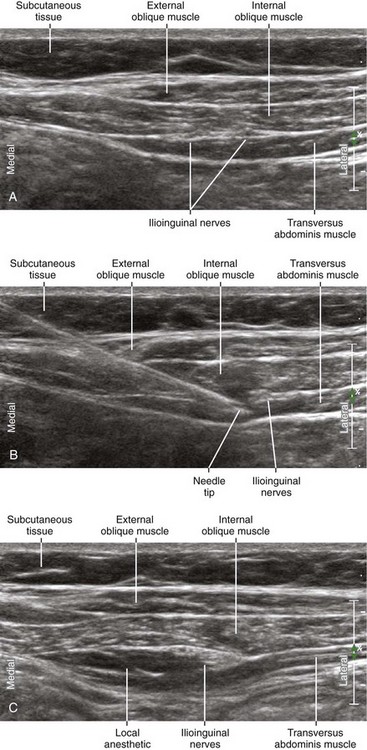
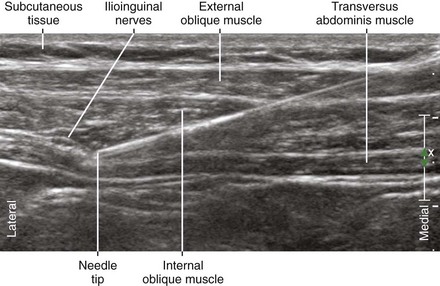
Nerve and muscle visibility are best cephalad to the pelvic brim.3 In the classic location for ilioinguinal block (2 cm medial and 2 cm superior to the anterior-superior iliac spine), the external oblique muscle is often aponeurotic, and therefore it is difficult to visualize this layer over the nerves. The first step is to obtain a view of the three abdominal wall muscles (external oblique, internal oblique, and transversus) to identify the ilioinguinal nerves between the internal oblique and transversus. Alternatively, the deep circumflex artery can be followed up from the external iliac artery until it meets the ilioinguinal nerves.
Key Points
| Ilioinguinal Nerve Block | The Essentials |
|---|---|
| Anatomy | The ILIH nerves lie between the IO and TA near the base of the IC. |
| The ILN lies 6 mm medial to the IC. | |
| The IHN lies 10 mm medial to the ILN. | |
| The IC has an inverted U appearance. | |
| The iliacus muscle lies under the TA at the IC. | |
| The DCIA is a recurrent branch of the external iliac artery. | |
| The ILN is often accompanied by the DCIA. | |
| The course of the ILN parallels the inside of the pelvic brim. | |
| ILN and IHN are about 3 × 1.5 mm in diameter. | |
| Image orientation | The ILIH nerves lie medial to the iliac crest. |
| Positioning | Supine |
| Operator | Standing at the side of the patient (either side) |
| Display | Across the table |
| Transducer | High-frequency linear, 38- to 50-mm footprint |
| Initial depth setting | 25 to 30 mm |
| Needle | 20 to 21 gauge, 70 mm in length |
| Anatomic location | Begin by placing the transducer above the iliac crest. |
| Look caudally with the transducer to image the IC. | |
| Rotate the transducer to obtain a SAX view of the ILIH nerves. | |
| Alternatively, begin scanning below the ASIS with ILN in SAX view. | |
| Identify the ILN lying on the start of the upslope of the TA. | |
| Slide the transducer to follow the ILN as proximally as possible. | |
| Approach | SAX view of ILIH, in-plane from medial to lateral. |
| Place the needle tip between ILN and IHN near the base of the IC. | |
| Sonographic assessment | The injection should layer between the IO and TA. |
| Anatomic variation | The ILN may not lie between IO and TA (10%). |
| The ILN and IHN can be fused together (12%). |
Clinical Pearls
• Ilioinguinal blocks are useful for pain relief after lower abdominal incisions (e.g., cesarean delivery, abdominal hysterectomy) and inguinal hernia repair.
• The course of the ilioinguinal nerve and deep circumflex iliac artery parallels the inside aspect of the pelvic brim.4
• The needle should be aimed at the corner of the neurovascular bundle, where the ilioinguinal nerves lie adjacent to the deep circumflex iliac artery. Power Doppler helps identify this small artery. In contrast to the artery, the nerves will not have color encoding with appropriate adjustment of the Doppler gain. The injection can be performed where the artery lies between the internal oblique and transversus muscle layers or as proximal as possible.
• The transversus muscle is thin, and therefore intraperitoneal placement of the needle tip can occur.
• The diameters of the ilioinguinal and iliohypogastric nerves are about 3 × 1.5 mm each. The two nerves usually lie about 10 mm apart from each other. The ilioinguinal nerve lies about 6 mm from the iliac bone. One common anatomic variation in this region is fusion of the ilioinguinal and iliohypogastric nerves into a common trunk, occurring in about 12% of normal subjects.2
• The best imaging of these nerves is about 5 cm cranial and slightly posterior to the anterior-superior iliac spine. In this location the two nerves consistently lie between the internal oblique and transversus muscles.2
• The transducer should be slightly rotated to image perpendicular to the course of the nerves and close enough to the bone that the iliac crest should be within the field of view. If the needle tip is sufficiently lateral, the iliacus or quadratus lumborum muscle, rather than peritoneum, will lie under the transversus.
• Because the cutaneous innervation of the ilioinguinal nerves is variable, there are no accurate clinical tests of block assessment.
1 Fredrickson MJ, Paine C, Hamill J. Improved analgesia with the ilioinguinal block compared to the transversus abdominis plane block after pediatric inguinal surgery: a prospective randomized trial. Paediatr Anaesth. 2010;20:1022–1027.
2 Rankin G, Stokes M, Newham DJ. Abdominal muscle size and symmetry in normal subjects. Muscle Nerve. 2006;34:320–326.
3 Eichenberger U, Greher M, Kirchmair L, et al. Ultrasound-guided blocks of the ilioinguinal and iliohypogastric nerve: accuracy of a selective new technique confirmed by anatomical dissection. Br J Anaesth. 2006;97:238–243.
4 Schlenz I, Burggasser G, Kuzbari R, et al. External oblique abdominal muscle: a new look on its blood supply and innervation. Anat Rec. 1999;255:388–395.