CHAPTER 28 Iliacus block
Clinical anatomy
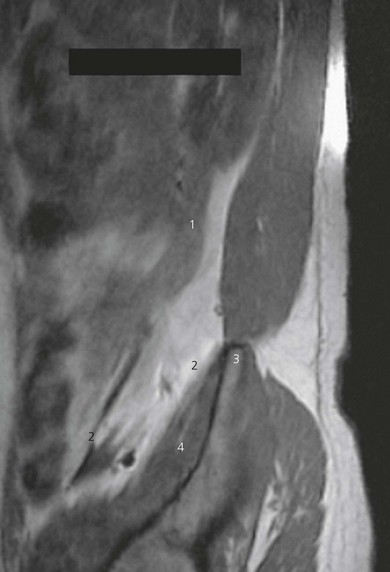
The iliacus fascia covers the iliacus and psoas muscles in the pelvis and descends into the thigh with these muscles (Fig. 28.1). The femoral nerve lies anterior to the psoas muscle initially, with the lateral cutaneous nerve of the thigh lateral to the psoas muscle and obturator nerve medial. At the inguinal ligament, the femoral nerve lies in a gutter between the psoas and iliacus muscles. These nerves thus lie beneath the iliacus fascia (Fig. 28.1). Spread of local anesthetic (Figs 28.2 and 28.3) beneath the iliacus fascia produces a higher success rate of anesthesia of the femoral nerve, lateral cutaneous nerve of the thigh, and obturator nerves than the femoral nerve block technique.
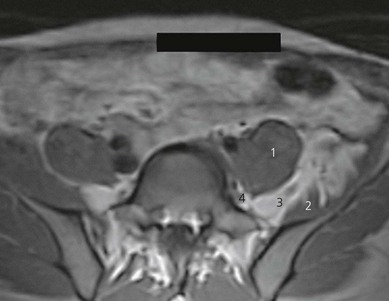
Figure 28.2 Axial T1-weighted MR image after injection of 40 mL of contrast, showing spread of injectate. Compare with Figure 21.5. Note contrast surrounding femoral and obturator nerves. Spread is via the plane between the iliacus and psoas muscles. 1: psoas muscle; 2: iliacus muscle; 3: femoral nerve; 4: obturator nerve.
Surface anatomy
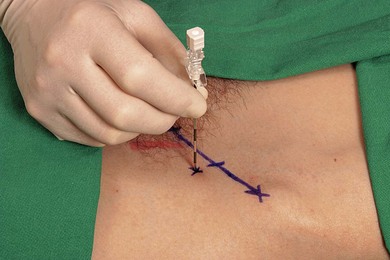
The inguinal ligament is outlined by a line connecting the anterior superior iliac spine and the pubic tubercle. The inguinal ligament is divided into equal thirds. At the junction between the outer one-third and inner two-thirds, a perpendicular line is drawn; 1 cm along this line is the needle insertion point (Fig. 28.4). The femoral artery can be palpated 2–3 cm more medially in the groin.
It is important to remember that with a fractured neck of femur these relations may change.
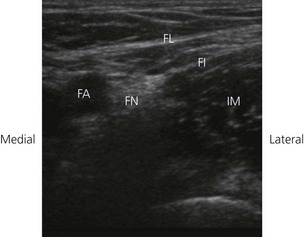
Sonoanatomy
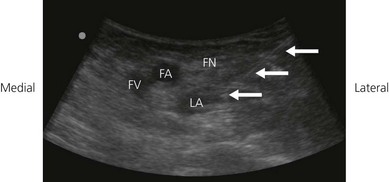
The iliacus muscle is found lateral to the femoral artery in the groin, lying outside the femoral sheath and beneath the fascia lata and iliaca. A transverse ultrasound transducer orientation is used (Fig. 28.5). The fascia lata and iliaca are seen as hyperechoic lines. The appearance of the iliacus muscle on ultrasound is hypoechoic with hyperechoic fascial boundaries (Fig. 28.6).
A scanning routine is used. To identify the iliacus muscle, the transducer is placed over the femoral vessels on the anterior thigh at 90° to the expected orientation of the nerve and vessels (Fig. 28.5). Identify the fascia lata. Move the tranducer laterally. Identify the fascia iliaca as a hyperechoic line deep to the fascia lata. The iliacus muscle lies beneath.
Technique
Landmark-based approach
The patient is placed in the supine position, with the operator standing on the side to be blocked, at the level of the patient’s thigh. Having outlined landmarks, the needle insertion point is infiltrated with local anesthetic using a 25-G needle. An 18-G Tuohy needle is inserted perpendicular to the skin (Fig. 28.7). An initial loss of resistance is identified on penetrating the fascia lata. A second loss of resistance indicates penetration of the fascia iliaca. No muscle response is sought. Incremental injection of local anesthetic (30–40 mL) is made with repeated aspiration. No resistance to injection should be present.
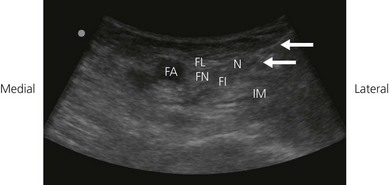
Ultrasound-guided approach
The operator stands on the side to be blocked, and with the patient in a supine position (Fig. 28.5). The skin is disinfected with antiseptic solution and draped. A sterile sheath (CIVCO Medical Instruments, Kalona, IA, USA) is applied over the ultrasound transducer with sterile ultrasound gel (Aquasonic, Parker Laboratories, Fairfield, NJ, USA). Another layer of sterile gel is placed between the sterile sheath and the skin. The infrainguinal region is scanned with a 6–13 MHz linear transducer. The ultrasound screen should be made to look like the scanning field. That is, the right side of the screen represents the right side of the field. Adjustable ultrasound variables such as scanning mode, depth of field, and gain are optimized.
A transverse image of the iliacus muscle is obtained (Fig. 28.6). The iliacus muscle is kept in the center of the field of view. The needle entry site is at the lateral-most end of the linear transducer. A 23-gauge needle is advanced under real-time ultrasound guidance and local anesthetic is deposited along the needle entry path. A free hand technique rather than the use of a needle guide is preferred. An 18-GA 21-Tuohy needle is inserted parallel to the axis of the beam of the ultrasound transducer, with the bevel facing the transducer (Fig. 28.8). The needle is attached to sterile extension tubing, which is connected to a 20-mL syringe and flushed with local anesthetic solution to remove all air from the system. It is then introduced at the lateral-most end of the transducer and visualized along its entire path to the iliacus muscle (Fig. 28.9). It is important not to advance the needle without good visualization. This may require needle or ultrasound transducer adjustment.
Once the needle has advanced deeper than the iliacus fascia, 1–2 mL of local anesthetic may be injected to confirm correct needle placement. Local anesthetic appears as a hypoechoic image. Correct needle placement is confirmed by observing solution surrounding beneath the iliacus fascia (Fig. 28.10). Should this not occur, the needle may need to be repositioned, and the procedure repeated. Following confirmation of correct needle placement, 30–40 mL of local anesthetic solution can be injected to achieve blockade.
Adverse effects
Capdevila X, Biboulet P, Bouregba M, et al. Comparison of the three-in-one and fascia iliaca compartment blocks in adults: clinical and radiographic analysis. Anesth Analg. 1998;86:1039-1044.
Dolan J, Williams A, Murney E, et al. Ultrasound guided fascia iliaca block: a comparison with the loss of resistance technique. Reg Anesth Pain Med. 2008;33(6):526-531.
Kizelshteyn G, Crevecoeur E. Anatomic consideration of the fascia iliaca compartment block. Anesth Analg. 1990;71:210-212.
Paut O, Sallabery M, Schreiber-Deturmeny E, et al. Continuous fascia iliaca compartment block in children: a prospective evaluation of plasma bupivacaine concentrations, pain scores, and side effects. Anesth Analg. 2001;92:1159-1163.