Idiopathic Condylar Resorption
Evaluation and Treatment
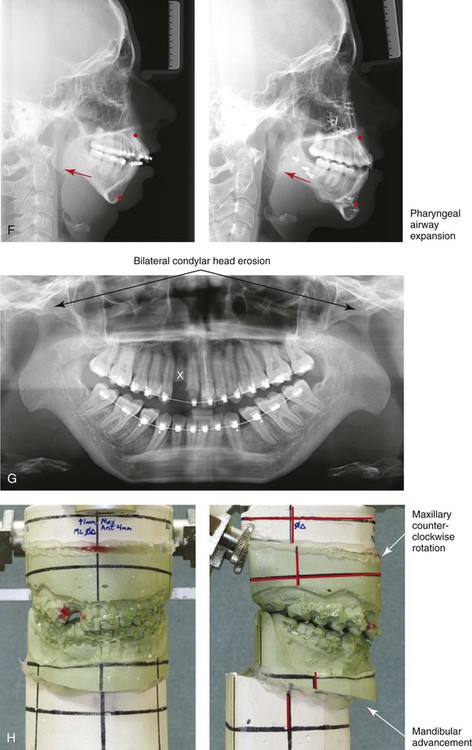
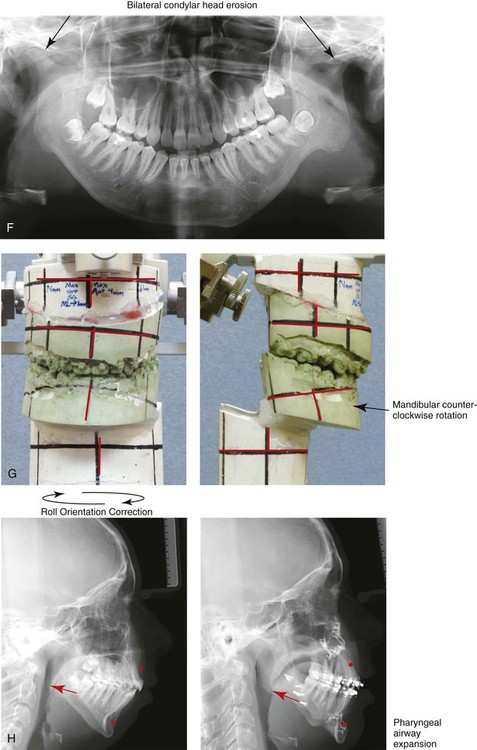
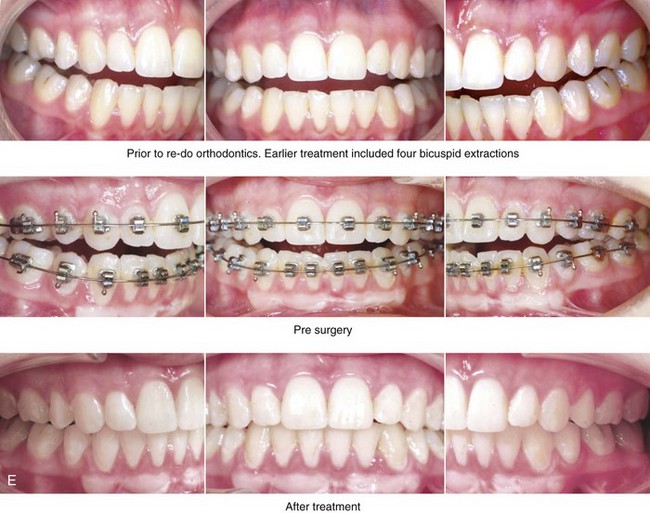
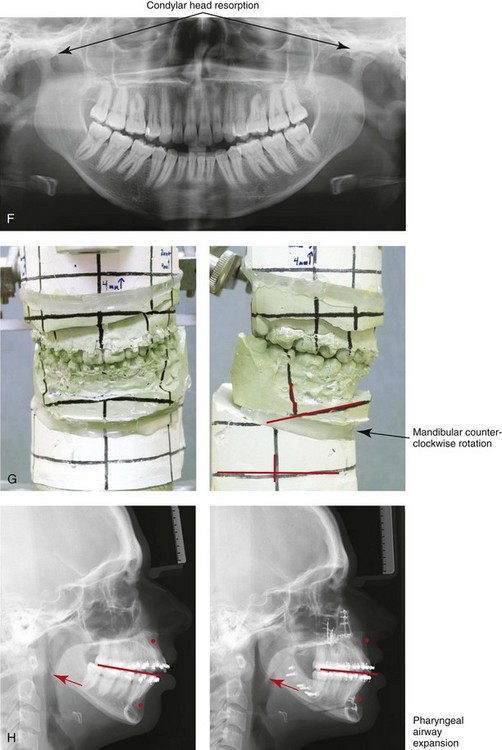
In patients with the condition of uncertain etiology that is commonly referred to as idiopathic condylar resorption (ICR)*, the condyles of the mandible partially resorb, thereby causing a loss of condylar height with secondary alterations of the maxillofacial morphology, occlusion, and head and neck function.34,43,100 Progressive condylar resorption (PCR)* is a general term that is used to describe conditions that result in a similar loss of condylar height and secondary effects but with known associations (e.g., juvenile idiopathic arthritis, including any of its seven subtypes).13,24,59,76,92,93
In general, ICR has the following features:
• It generally affects girls and women who are between the ages of 15 and 35 years.
• It is most frequent among teenage girls during the pubertal growth spurt.
• It typically results in bilateral symmetric condylar involvement followed by stabilization (remission). In the majority of affected individuals, limited further resorption occurs. Unfortunately, in some, a second episode will result in the further loss of condylar height.
• There is no agreed-upon and proven etiology. ICR frequently seems to occur as part of the natural course of events rather than in conjunction with active therapy or treatment. It may also coincide with or be observed during or after active dental restorative, orthodontic, or surgical interventions.
• During the active phase of condylar resorption, TMJ and masticatory muscle discomfort is expected. The active phase often subsides within 6 to 12 months.
• When the condition becomes quiescent, the individual is generally left with satisfactory TMJ function without significant limitations in mouth opening or intracapsular pain. Persistent joint noise is frequent.
• Head and neck functions are likely to be negatively impacted including: chewing; breathing; speech articulation; and body image.
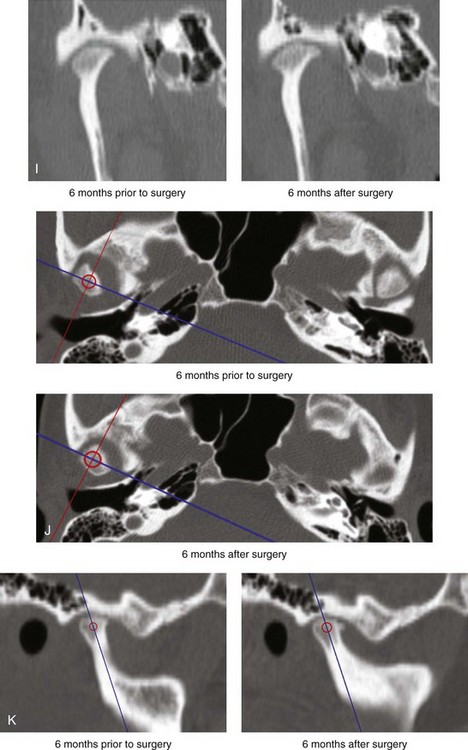
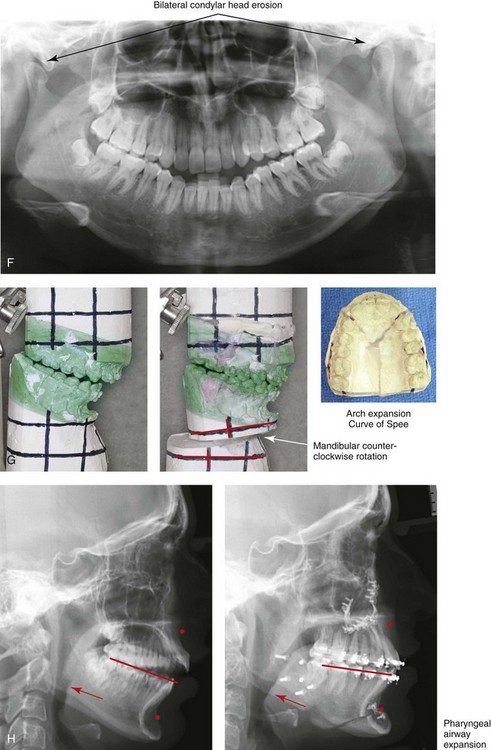
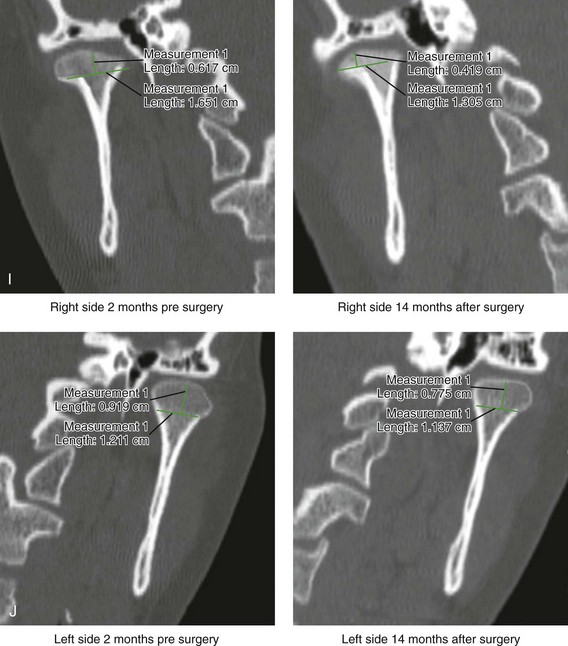
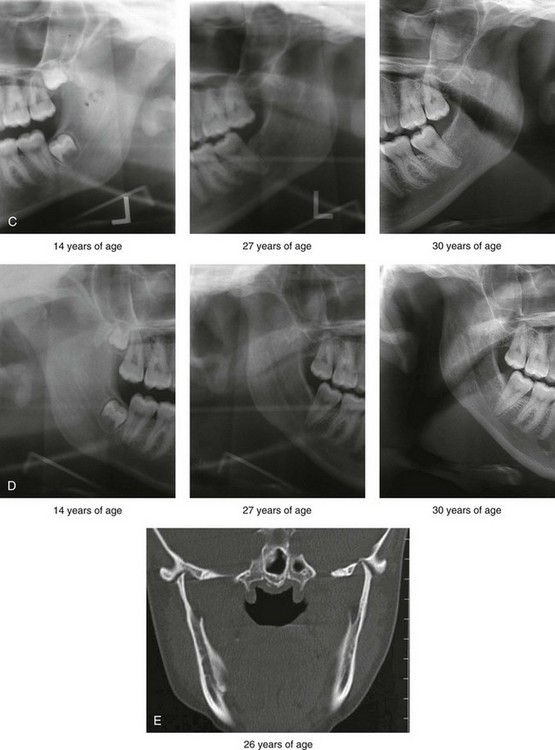
• When the condition is in remission, a cartilaginous cap over an intact cortical rim can generally be documented. A deflated or diminished condylar head is generally seen on imaging (e.g., magnetic resonance imaging or computed tomography scanning). The glenoid fossa and the articular disc typically remain biologically intact.
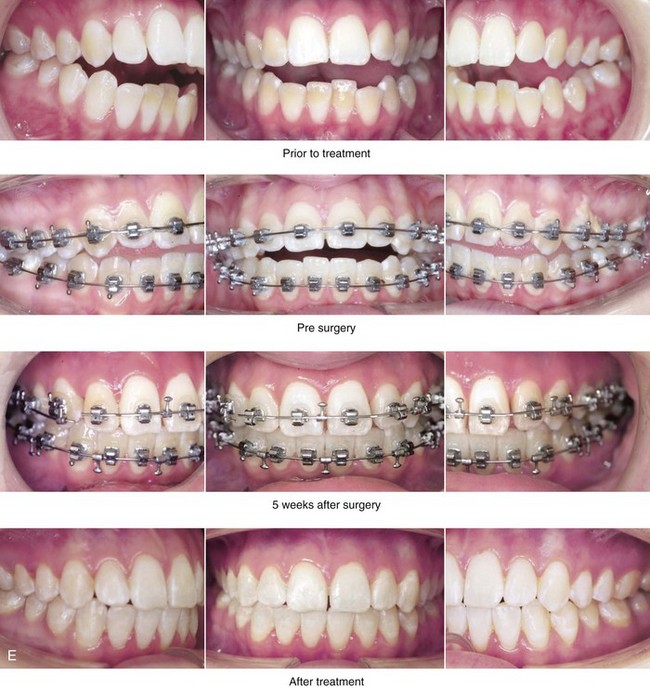
Mandibular and occlusal findings generally include the following:
• Change in the shape of the condylar heads (i.e., flattening and thinning)
• Loss of overall posterior facial height
• Mandibular retropositioning with clockwise rotation (high angle)
• Angle Class II anterior open bite, excess overjet malocclusion
Theories of Etiology
The current dominant theory holds that the etiology of ICR is hormonally mitigated, immunologically controlled and may arise in genetically susceptible individuals in conjunction with environmental factors.* Sex hormones are thought to modulate biochemical changes within the TMJ, which may then result in condylar resorption. For some time, it has been suggested that there is alteration in the serum hormonal levels in at least some affected girls and women with ICR.31 Gunson and colleagues described endocrine function among women who arrived at their clinic with a history, physical examination, and radiographic findings that were consistent with ICR. The average age at presentation was 26 years (range, 15 to 45 years).31 Twenty-five of the 27 patients (93%) had low levels of serum 17-beta estradiol at the mid-menstrual cycle. Two subgroups were further differentiated. The first group did not produce estrogen naturally (8 out of 27 patients), and the second group (19 out of 27 patients) had low 17-beta estradiol levels that were presumed to be the result of oral contraceptive pill usage. The authors theorize that, whether the condition is induced by ethinyl estradiol (i.e., oral contraceptive pills) or by premature ovarian failure, a low circulating 17-beta estradiol serum level negatively affects the natural reparative capacity of the condyles. The authors believe that, when 17-beta estradiol deficiency is coupled with the presence of local factors that cause compressive forces, condylar lysis is more likely to occur and to ultimately result in the observed condition called ICR.8,14,27,46,64 Unfortunately, the study did not include a control group for oral contraceptive pill use or precise knowledge of the phase of the menstrual cycle at the time of hormone serum sampling. Although hormone influences no doubt play a role, an autoimmune aspect is also likely.31
Gunson and Arnett comment that whatever the underlying etiology of ICR, all bone loss at the condylar level involves a common resorptive pathway that includes cytokine-activated osteoblasts that then recruit and promote the activity of osteoclasts.32 This in turn results in the secretion of enzymes that are responsible for the breakdown of hydroxyapatite and collagen. A case in point is juvenile idiopathic arthritis (ex. polyarticular arthritis, rheumatoid factor positive), which is caused by a B-cell–mediated autoimmune reaction to synovial tissues.33,80,105 A consequence of this reaction is the presence of local inflammatory cells, which secrete cytokines that cause the activation of osteoblast-mediated osteoclast catabolism.89 The end result is bone breakdown through the common resorptive pathway.30 In patients with juvenile idiopathic arthritis (JIA), a current treatment approach is to minimize articular bone loss by using pharmacologic drugs that interfere with specific cytokines and enzymes along the common resorptive pathway rather than open joint or joint replacement procedures. This may include non-steroidal anti-inflammatories (NSAIDS) or other drugs such as methotrexate or a newer class of medications called biologicals. 10,35,36,39,48,52,80,105 Gunson and Arnett point out that a similar approach to ICR may prove to be useful.32
Another theory of the cause of ICR is avascular necrosis of the condyle as a result of the compression of specific vessels that supply the condyle followed by condylysis, loss of condyle height with secondary jaw deformity and malocclusion.16,17,45,62,72,81–84 Piper and Choung had speculated that pathologic compressive forces of the posterior aspect of the condyle on the ligamentous retrodiscal soft tissues constrict the small vessels, thereby limiting circulation to the condyles with resulting in aseptic necrosis that accounts for the observed condylysis in patients with ICR.17,72 They went on to hypothesize that either a chronically dislocated non-reducing disc or specific patterns of malocclusion may also cause this cycle of events. As an extension of this thinking, preventative open-joint procedures were offered to alleviate the theoretical compression of the condylar circulation. Those of us that are skeptical of the non-reducing disc cause of ICR point out that the almost universally observed bilateral symmetric simultaneous nature of this condition and its occurrence only in females make the theory an improbable explanation.
Clinical Perspectives
Some clinicians suggest that, with a lack of clarity about either the etiology of the condition or the effects of various treatment modalities and without a guaranteed endpoint to the condylar degeneration in any given patient, it is best to remove the affected condyles and either reconstruct them with a costochondral (rib) graft or to remove the whole joint (i.e., the condyle, the disc, and the glenoid fossa) and replace it with an alloplastic total joint. Proponents of a partial or total joint replacement approach to the management of ICR are correct in their thinking that the only way to be certain that a further loss of posterior facial height will not continue is to remove and replace the condyle.55,56,107,110 For the great majority of patients with ICR, joint replacement treatment seems radical on the basis of the following: 1) the unlikely probability of long-term TMJ pain 2) the expected satisfactory long-term mandibular (mouth) opening 3) the expected condylar stabilization (“burn-out”) that is typically seen and 4) the known potential for perioperative complications with invasive open joint procedures and the long-term failure rates of total joint replacement.
Mercuri presents an alternative point of view with a recommendation for total joint replacement to “eliminate the variable issue of ongoing condylar resorption.”55,56 He offers total alloplastic reconstruction as a definitive solution. He also states that the non-alloplastic (biologic) condyle option (e.g., costochondral grafting) requires stabilization of the graft with minimal mobility while integration (union) to the host mandibular occurs. This limits early masticatory muscle rehabilitation, which he feels is contrary to the tenets of physical rehabilitation after joint surgery. The disadvantages of alloplastic total TMJ reconstruction include the following: 1) the cost of the device 2) the expected material wear 3) the potential for long-term instability and failure 4) the incidence of both early and late complications including infections with the associated need for device removal and 5) the fact that alloplastic implants will not follow a patient’s normal growth pattern. Joint replacement advocates admit that patients must be advised that alloplastic total TMJ reconstruction devices are expected to have a limited functional life. In addition, the total joint replacement approach requires the removal of the functional glenoid fossa and disc along with excision of the condylar head, neck, and posterior ramus on both sides.
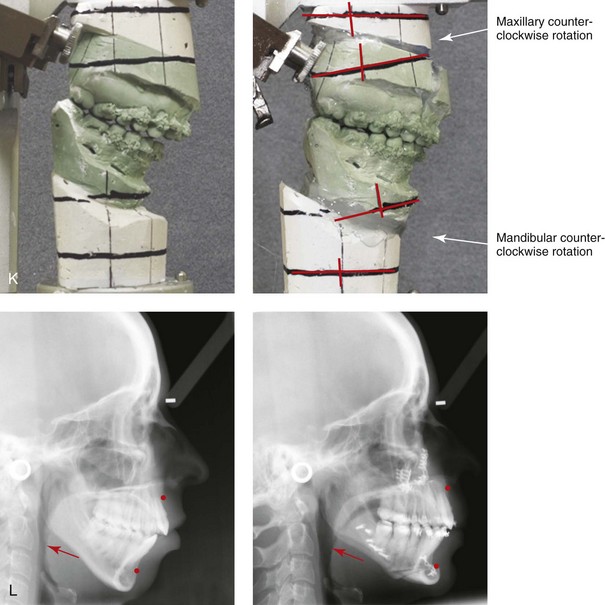
Some clinicians speculate that, if “decompressive” TMJ treatment is initiated early during the clinical course of active ICR, then less condylar resorption will occur. Others believe that, after the resorptive process has begun, it runs its course despite any attempt to “unload” the joint. Even with a lack of evidence-based research into the subject, most clinicians recommend attempts to limit mechanical compressive TMJ forces through the use of conservative measures (i.e., splints, muscle relaxants, medications and, diet modifications) in the hopes that less resorption (condylysis) will occur.11,12,19,21,25,37,40,47,63,66,101 Some authors believe that counterclockwise rotation of the maxillomandibular complex as part of the orthognathic correction will increase the compressive condylar forces, whereas others state that it is actually a method of “unloading” the joint.20,22,41,44,50,57,61,71,85,88,105,108 I agree with the published studies that document long-term skeletal stability when counterclockwise rotation of the maxillomandibular complex is carried out as part of the correction of mandibular-deficient dentofacial deformity.74,75,77,109 A common concern is that TMJ “loading” (i.e., the presence of compressive forces) will occur if the condyles are “overseating” or if medial or lateral condylar torquing is allowed to occur during orthognathic surgery.3–6 Some clinicians speculate that individuals who have persistent TMJ symptoms (e.g., popping, clicking) after the orthodontic treatment and corrective orthognathic surgery are at higher risk for progression.2 Most published studies confirm that joint noise (e.g., popping, clicking, grating) is not in itself an indicator of future condylar resorption.60,87,104
Current Clinical Approach to Correction of the Secondary Jaw Deformities
After the diagnosis of ICR is made, non-invasive measures (e.g., splint therapy, muscle relaxants, medications, and diet modification) to “unload” and “stabilize” the condyles or at least to relieve masticatory muscle hyperactivity and discomfort are initiated. Orthognathic procedures and orthodontic treatment carried out to correct the secondary malocclusion, the facial dysmorphology, and to open the airway are more likely to be maintained if the condylar resorption process has been stable for a period of time.49,77,112 Stability can be documented by minimal ongoing change in the occlusion, an intact cartilaginous cap, and an underlying rim of cortical bone over the partially resorbed condyle. The judicious use of technetium-99m methylene diphosphonate quantitative condylar bone scintigraphy can be a helpful tool for assessing whether or not condylysis is active.9,18,26,53,69,70,73,78,90,103 Unfortunately, these and other tests only confirm the current anatomy and activity level; they cannot predict the future.
The suggestion that, for the patient who has experienced ICR, the use of distraction osteogenesis techniques rather than standard orthognathic procedures will achieve a more stable long-term occlusion is not supported by the literature.38,54,68,91,94,95,102 The distraction approach 1) generally limits the region of reconstruction to the mandible 2) it requires greater patient convalescences and compliance, and 3) it may increase (rather than decrease) the compressive forces on the condyles.
When the condylar resorption process is believed to be “burnt out,” a comprehensive approach to correct the secondary deformities that involves an orthodontist, an orthognathic surgeon, a TMJ specialist, and appropriate imaging studies is recommended. Periodontal and restorative dental work may also be needed. Evaluation by a rheumatologist should also be considered. A thorough evaluation of the upper airway is essential to clarify any day and nighttime breathing difficulties. The simultaneous correction of chronic nasal airway obstruction and any baseline obstructive sleep apnea should be a primary objective (see Chapters 10 and 26).
The key to a favorable reconstruction for an individual with end-stage ICR or PCR is to define the functional disability (i.e., breathing, chewing, speech, swallowing, lip closure) and the extent of skeletal dysmorphology. The establishment of a functional occlusion that limits stress in the entire masticatory system without significant centric relation–centric occlusion discrepancies and without parafunctional habits is desirable (see Chapter 9). The successful performance of orthognathic, intranasal, and dental procedures to achieve these objectives represents our standard approach; see the case presentations later in this chapter.
Kaban and colleagues offers an alternative approach when the patient is not willing to take the risk that a degree of resorption may continue or reoccur at some point in the future.24,43,67,92,96–98 The authors completed a retrospective case series of 15 patients with the diagnosis of active bilateral ICR who chose a condylar replacement approach between 1999 and 2004. Each patient underwent bilateral endoscopic-assisted condylectomy and autogenous costochondral graft reconstruction. Patients with the following characteristics were included:
Brief Overview of Author’s Current Thinking
The definitive correction of the secondary maxillomandibular deformity through standard osteotomies in combination with appropriate orthodontics has proven beneficial to improve the occlusion, to open the airway, and to enhance facial aesthetics. Concern about further resorption of the “fragile” condyles is best managed by avoiding masticatory activities that “load” (i.e., compress) the joint and with the use of systemic medications when indicated.32
The treatment of juvenile idiopathic arthritis (JIA) has improved dramatically during recent years with the advent of disease-modifying anti-rheumatoid drugs. The orthognathic surgeon will encounter patients on a drug regimen that consists of nonsteroidal anti-inflammatory drugs [NSAIDS], glucocorticoids, methotrexate, and biologic agents. In these cases, consultation with a rheumatologist is recommended, but the surgeon should also be aware of these medications, because their presence could affect surgical outcome. Prudent perioperative management of these drugs is necessary to optimize surgical outcome. A balance must be struck between minimizing potential surgical complications and maintaining disease control to prevent further joint damage (i.e., condylar resorption) that would negatively affect the outcome.41A
References
1. Abubaker, AO, Arslan, W, Sotereanos, GC. Estrogen and progesterone receptors in the temporomandibular joint disk of symptomatic and asymptomatic patients. J Oral Maxillofac Surg. 1993; 51:1096.
2. Anderson, Q. Discussion of: Mandibular retrusion, temporomandibular joint derangement, and orthognathic surgery planning. Plast Reconstr Surg. 1992; 2:230–232.
3. Arnett, GW, Milam, SB, Gottesman, L. Progressive condylar resorption: Host adaptive capacity factors. Am J Orthod Dentofacial Orthop. 1995.
4. Arnett, GW, Milam, SB, Gottesman, L. Progressive mandibular retrusion—idiopathic condylar resorption. Part I. Am J Orthod Dentofacial Orthop. 1996; 110:8–15.
5. Arnett, GW, Milam, SB, Gottesman, L. Progressive mandibular retrusion—idiopathic condylar resorption. Part II. Am J Orthod Dentofacial Orthop. 1996; 110:117–127.
6. Arnett, GW, Tamborello, JA. Progressive Class II development: Female idiopathic condylar resorption. Oral Maxillofac Clin North Am. 1990; 2:699.
7. Aufdemorte, TB, Van Sickels, JE, Dolwick, MF, et al. Estrogen receptors in the temporomandibular joint of the baboon: An autoradiographic study. Oral Surg. 1986; 61:307.
8. Bain, SD, Gross, TS. Structural aspects of bone resorption. In: Bronner F, Farach-Carson MC, eds. Bone resorption. London, UK: Springer-Verlag; 2005:58–66.
9. Barrett, MB, Smith, PHS. Bone imaging with 99Tc in polyphosphate: A comparison with 18F and skeletal radiology. Br J Radiol. 1974; 17:387.
10. Bergink, AP, Uitterlinden, AG, Van Leeuwen, JP, et al. Vitamin D status, bone mineral density, and the development of radiographic osteoarthritis of the knee: The Rotterdam study. J Clin Rheumatol. 2009; 15:230.
11. Bilodeau, JE. Retreatment of a patient who presented with condylar resorption. Am J Orthod Dentofacial Orthop. 2007; 131:897.
12. Bouwman, JPB, Kerstens, HCJ, Tuinzing, DB. Condylar resorption in orthognathic surgery: The role of intermaxillary fixation. Oral Surg Med Oral Pathol. 1994; 78:138–141.
13. Brennan, MT, Patronas, NJ, Brahim, JS. Bilateral condylar resorption in dermatomyositis: A case report. Oral Surg Oral Med Oral Path Oral Radiol Endod. 1999; 87:446.
14. Burr, DB. Muscle strength, bone mass, and age-related bone loss. J Bone Miner Res. 1997; 12:1547.
15. Censi, S, Weitzmann, MN, Roggia, C, et al. Estrogen deficiency induces bone loss by enhancing T-cell production of TNF-alpha. J Clin Invest. 2000; 106:1229.
16. Chuong, R, Piper, MA. Avascular necrosis of the mandibular condyle: Pathogenesis and concept of management. Oral Surg Oral Med Oral Pathol. 1993; 75:428.
17. Chuong, R, Piper, MA, Boland, TJ. Osteonecrosis of the mandibular condyle: Pathophysiology and core decompression. Oral Surg Oral Med Oral Pathol. 1995; 79:539.
18. Cisneros, G, Kaban, LB. Computerized skeletal scintigraphy for assessment of mandibular asymmetry. J Oral Maxillofac Surg. 1985; 42:513.
19. Copray, JCVM, Jansen, HWB, Duterloo, HS. The role of biomechanical factors in mandibular condylar cartilage growth and remodeling in vitro. In: McNamara JA, Jr., eds. Craniofacial growth series. Center for Human Growth and Development. Ann Arbor, Mich: University of Michigan Press, 1984.
20. Crawford, JG, Stoelinga, JW, Blijdorp, PA, Brouns, JJ. Stability after reoperation for progressive condylar resorption after orthognathic surgery: Report of seven cases. J Oral Maxillofac Surg. 1994; 52:460–466.
21. Cutbirth, M, Sickels, JE, Thrash, WJ. Condylar resorption after bicortical screw fixation of mandibular advancement. J Oral Maxillofac Surg. 1998; 56:178–182.
22. De Clercq, CA, Neyt, LF, Mommaerts, MY, et al. Condylar resorption in orthognathic surgery: A retrospective study. Int J Adult Orthodon Orthognath Surg. 1994; 9:233–240.
23. Eghbali-Fatoureschi, G, Khosla, S, Sanyal, A, et al. Role of RANK ligand in mediating increased bone resorption in early postmenopausal women. J Clin Invest. 2003; 111:1221.
24. Ferguson, JW, Luyk, NH, Parr, NC. A potential role for costo-chondral grafting in adults with mandibular condylar destruction secondary to rheumatoid arthritis: A case report. J Craniomaxillofac Surg. 1993; 21:15.
25. Forwood, MR, Turner, CH. Skeletal adaptations to mechanical usage: Results from tibial loading studies in rats. Bone. 1995; 17(4 Suppl):197S.
26. Frost, HM. Tetracycline-based histological analysis of bone remodeling. Calcif Tissue Res. 1969; 3:211.
27. Frost, HM. The skeletal intermediary organization. Metab Bone Dis Relat Res. 1983; 4:281.
28. Frost, HM. Changing concepts in skeletal physiology: Wolff’s Law, the mechanostat and the “Utah Paradigm. ”. J Hum Biol. 1998; 10:599.
29. Frost, HM. Perspective on the estrogen-bone relationship and postmenopausal bone loss: A new model. J Bone Miner Res. 1999; 14:1473.
30. Guler, N, Yatmaz, PI, Ataoglu, H, et al. Temporomandibular internal derangement: Correlation of MRI findings with clinical symptoms of pain and joint sounds in patients with bruxing behavior. Dentomaxillofac Radiol. 2003; 32:304.
31. Gunson, MJ, Arnett, GW, Formby, B, et al. Oral contraceptive pill use and abnormal menstrual cycles in women with severe condylar resorption: A case for low serum 17B-estradiol as a major factor in progressive condylar resorption. Am J Orthod Dentofacial Orthop. 2009; 136:772–779.
32. Gunson, MJ, Arnett, GW, Milam, SB. Pathophysiology and pharmacologic control of osseous mandibular condylar resorption. J Oral Maxillofac Surg. 2012; 70:1918–1934.
33. Hajati, AK, Alstergren, P, Masstrom, K, et al. Endogenous glutamate in association with inflammatory and hormonal factors modulates bone tissue resorption of the temporomandibular joint in patients with early rheumatoid arthritis. J Oral Maxillofac Surg. 2009; 67:1895.
34. Handelman, CS. Ask us: Condylar resorption. Am J Orthod Dentofacial Orthop. 2004; 125:16A.
35. Heidari, B, Hajian-Tilaki, K, Heidari, P. The status of serum vitamin D in patients with rheumatoid arthritis and undifferentiated inflammatory arthritis compared with controls. Rheumatol Int. 2012; 32:991–995.
36. Heidari, B, Heidari, P, Hajian-Tilaki, P. Association between serum vitamin D deficiency and knee osteoarthritis. Int Orthop. 2011; 35:1627–1631.
37. Herford, AS, Hoffman, R, Demirdji, S, et al. Comparison of synovial fluid pressure after immediate versus gradual mandibular advancement in the miniature pig. J Oral Maxillofac Surg. 2005; 63:775.
38. Hikiji, H, Takato, T, Matsumoto, S, et al. Experimental study of reconstruction of the temporomandibular joint using a bone transport technique. J Oral Maxillofac Surg. 2000; 58:1270.
39. Holick, MF. The vitamin D epidemic and its health consequences. J Nutr. 2005; 135:2739S.
40. Hoppenreijs, TJ, Freihofer, HP, Stoelinga, PJ, et al. Condylar remodeling and resorption after Le Fort I and bimaxillary osteotomies in patients with anterior open bite: A clinical and radiological study. Int J Oral Maxillofac Surg. 1998; 27:81–91.
41. Hoppenreijs, TJ, Stoelinga, PJ, Grace, KL, et al. Long-term evaluation of patients with progressive condylar resorption following orthognathic surgery. Int J Oral Maxillofac Surg. 1999; 28:411.
Howe, CR, Gardner, GC, Kadel, NJ. Perioperative medication management for the patient with rheumatoid arthritis. J Am Acad Orthop Surg. 2006; 14:544–551.
42. Hoyland, JA, Mee, AP, Baird, P, et al. Demonstration of estrogen receptors in association with primary knee osteoarthritis in Korean population. Arthritis Res Ther. 2004; 6:R415.
43. Huang, YL, Pogrel, MA, Kaban, LB. Diagnosis and management of condylar resorption. J Oral Maxillofac Surg. 1997; 55:114.
44. Hwang, SJ, Haers, PE, Zimmermann, A, et al. Surgical risk factors for condylar resorption after orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 89:542–552.
45. Jacobs, JS. Discussion of: Osteonecrosis of the temporomandibular joint: Correlation of magnetic resonance imaging and histology. J Oral Maxillofac Surg. 1999; 57:899.
46. Jilka, RL. Biology of the basic multicellular unit and the pathophysiology of osteoporosis. Med Pediatr Oncol. 2003; 41:182.
47. Kannus, P, Sievanen, H, Vuori, L. Physical loading, exercise and bone. Bone. 1996; 18(Suppl 1):1.
48. Kapila, S, Wang, W, Uston, K. Matrix metalloproteinase induction by relaxin causes cartilage matrix degradation in target synovial joints. Ann N Y Acad Sci. 2009; 1160:322.
49. Kato, Y, Hiyama, S, Kuroda, T, et al. Condylar resorption 2 years following active orthodontic treatment: A case report. Int J Adult Orthodon Orthognath Surg. 1999; 14:243.
50. Kerstens, HC, Tuinzing, DB, Golding, RP, et al. Condylar atrophy and osteoarthrosis after bimaxillary surgery. Oral Surg. 1990; 69:274.
51. Kusec, V, Virdi, AS, Prince, R, et al. Localization of estrogen receptor-alpha in human and rabbit skeletal tissues. J Clin Endrocrinol Metab. 1998; 83:2421.
52. Lane, NE, Gore, LR, Cummings, SR, et al. Serum vitamin D levels and incident changes of radiographic hip osteoarthritis: A longitudinal study. Study of osteoporotic fractures research group. Arthritis Rheum. 1999; 42:854.
53. Larheim, TA, Westesson, PL, Hicks, D, et al. Osteonecrosis of the temporomandibular joint: Correlation of magnetic resonance imaging and histology. J Oral Maxillofac Surg. 1999; 57:888.
54. McCormick, SU, McCarthy, JG, Grayson, BH, et al. Effect of mandibular distraction on the temporomandibular joint: Part 1. Canine study. J Craniofac Surg. 1995; 6:358.
55. Mercuri, LG. A rationale for total alloplastic temporomandibular joint reconstruction in the management of idiopathic/progressive condylar resorption. J Oral Maxillofac Surg. 2007; 65:1600–1609.
56. Mercuri, LG. Osteoarthritis, osteoarthrosis, and idiopathic condylar resorption. Oral Maxillofac Surg Clin North Am. 2008; 20:169–183.
57. Merkx, MA, Van Damme, PA. Condylar resorption after orthognathic surgery: Evaluation of treatment in eight patients. J Craniomaxillofac Surg. 1994; 22:53–58.
58. Milam, SB, Aufdemorte, TB, Sheridan, PJ, et al. Sexual dimorphism in the distribution of estrogen receptors in the temporomandibular joint complex of the baboon. Oral Surg Oral Med Oral Pathol. 1987; 64:527.
59. Milam, SB. Pathogenesis of degenerative temporomandibular joint arthritides. Odontology. 2005; 93:7–15.
60. Mongini, F. Anatomic and clinical evaluation of the relationship between the temporomandibular joint and occlusion. J Prosthet Dent. 1977; 38:539.
61. Moore, K, Gooris, P, Stoelonga, P. The contributing role of condylar resorption to skeletal relapse following mandibular advancement surgery: Report of five cases. J Oral Maxillofac Surg. 1991; 49:448.
62. Morales-Ryan, CA, Garcia-Morales, P, Wolford, LM. Idiopathic condylar resorption: Outcome assessment of TMJ disc repositioning and orthognathic surgery. J Oral Maxillofac Surg. 2002; 60(Suppl 1):53.
63. Moseley, JR, Lanyon, LE. Strain rate as a controlling influence on adaptive remodeling in response to dynamic loading of the ulna in growing male rats. Bone. 1998; 23:313.
64. Nanes, MS, Pacifici, R. Inflammatory cytokines. In: Bronner F, Farach-Carson MC, Rubin J, eds. Bone resorption. London, UK: Springer-Verlag; 2005:67–90.
65. Okuda, T, Yasuoka, T, Nakashima, M, et al. The effect of ovariectomy on the temporomandibular joints of growing rats. J Oral Maxillofac Surg. 1996; 54:1202.
66. O’Ryan, F, Epker, BN. Temporomandibular joint function and morphology: Observations on the spectra of normalcy. Oral Surg Oral Med Oral Pathol. 1984; 58:272.
67. Papadaki, ME, Tayebaty, F, Kaban, LB, Troulis, MJ. Condylar resorption. Oral Maxillofac Surg Clin North Am. 2007; 19:223–234.
68. Papageorge, MB, Apostolidis, C. Simultaneous mandibular distraction and arthroplasty in a patient with temporomandibular joint ankylosis and mandibular hypoplasia. J Oral Maxillofac Surg. 1999; 57:328.
69. Parfitt, AM. The coupling of bone formation to bone resorption: A critical analysis of the concept and its relevance to the pathogenesis of osteoporosis. Metab Bone Dis Relat Res. 1982; 4:1.
70. Parfitt, AM. The cellular basis for bone remodeling: The quantum concept reexamined in light of recent advances in the cell biology of bone. Calcif Tissue Int. 1984; 36:S37.
71. Phillips, RM, Bell, WH. Atrophy of mandibular condyles after sagittal ramus split osteotomy: Report of a case. J Oral Maxillofac Surg. 1978; 36:45.
72. Piper, MA. Microscope disk preservation surgery of the temporomandibular joint. Oral Maxillofac Clin North Am. 1989; 1:279.
73. Pogrel, MA, Kopf, J, Dodson, TB, et al. A comparison of single photon emission computed tomography and planar imaging for quantitative skeletal scintigraphy of the mandibular condyle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 80:226.
74. Posnick, J, Fantuzzo, J, Orchin, J. Deliberate operative rotation of the maxillo-mandibular complex to alter the A-point to B-point relationship for enhanced facial esthetics. J Oral Maxillofac Surg. 2006; 64:1687–1695.
75. Posnick, JC. (Discussion of) Occlusal plane rotation: Aesthetic enhancement in mandibular micrognathia. Plast Reconstr Surg. 1993; 91:1241.
76. Posnick, JC, Fantuzzo, JJ. Idiopathic condylar resorption: Current clinical perspective. J Oral Maxillofac Surg. 2007; 65(8):1617–1623.
77. Rosen, HM. Occlusal plane rotation: Aesthetic enhancement in mandibular micrognathia. Plast Reconstr Surg. 1993; 91:1231.
78. Roser, SM, Mena, I. Diphosphonate dynamic imaging of experimental bone grafts and soft tissue injury. Int J Oral Surg. 1978; 7:488.
79. Salem, ML, Hossain, MS, Nomoto, K. Mediation of the immunomodulatory effect of beta-estradiol on inflammatory responses by inhibition of recruitment and activation of inflammatory cells and their gene expression of TNF-alpha and IFN-gamma. Int Arch Allergy Immunol. 2000; 121:235.
80. Sano, H, Arai, K, Murai, T, et al. Tight control is important in patients with rheumatoid arthritis treated with an anti-tumor necrosis factor biological agent: Prospective study of 91 cases who used a biological agent for more than 1 year. Mod Rheumatol. 2009; 19:390.
81. Schellhas, KP, Piper, MA, Bessette, R, et al. Mandibular retrusion, temporomandibular joint derangement, and orthognathic surgery planning. Plast Reconstr Surg. 1992; 2:218.
82. Schellhas, KP, Piper, MA, Omlie, MR. Facial skeletal remodeling due to temporomandibular joint degeneration: An imaging study of 100 patients. AJR Am J Roentgenol. 1990; 155:373–383.
83. Schellhas, KP, Pollei, SR, Wilkes, CH. Pediatric internal derangements of the temporomandibular joint: Effect on facial development. Am J Orthod Dentofacial Orthop. 1993; 104:52.
84. Schellhas, KP, Wilkes, CH, Fritts, HM, et al. MR of osteochondritis dissecans and avascular necrosis of the mandibular condyle. AJR Am J Roentgenol. 1989; 152:551–560.
85. Schendel, S, Tulasne, JF, Linck, DW. Idiopathic condylar resorption and micrognathia: The case for distraction osteogenesis. J Oral Maxillofac Surg. 2007; 65:1610–1616.
86. Schiessl, H, Frost, HM, Jee, WSS. Perspectives: Estrogen and bone-muscle strength and mass relationships. Bone. 1998; 22:1.
87. Schiffman, E, Fricton, JR. Epidemiology of TMJ and craniofacial pain. In: Fricton JR, Hathaway KM, eds. TMJ and craniofacial pain: Diagnosis and management. St. Louis: IEA, 1988.
88. Sesenna, E, Raffaini, M. Bilateral condylar atrophy after combined osteotomy for correction of retrusion. A case report. J Maxillofac Surg. 1985; 13:263.
89. Simopoulos, AP. Omega-3 fatty acids in inflammation and autoimmune diseases. J Am Coll Nutr. 2002; 21:495–505.
90. Stevenson, JS, Bright, RW, Dunson, GL, et al. Technetium 99m phosphate bone imaging: A method for bone graft healing. Radiology. 1974; 110:391.
91. Stucki-McCormick, SU, Fox, RM, Mizrahi, RD. Reconstruction of a neocondyle using transport distraction osteogenesis. Semin Orthod. 1999; 5:59.
92. Svensson, BG, Adell, R. Costochondral grafts to replace mandibular condyles in juvenile chronic arthritis patients: Long-term effects on facial growth. J Craniomaxillofac Surg. 1998; 26:275–285.
93. Svensson, BG, Feldmann, G, Rindler, A. Early surgical-orthodontic treatment of mandibular hypoplasia in juvenile chronic arthritis. J Craniomaxillofac Surg. 1993; 21:67–75.
94. Thurmuller, P, Troulis, MJ, Rosenberg, A, et al. Changes in the condyle and disc in response to distraction osteogenesis of the minipig mandible. J Oral Maxillofac Surg. 2002; 60:1327.
95. Thurmuller, P, Troulis, MJ, Rosenberg, A, et al. Microscopic changes in the condyle and disc in response to distraction osteogenesis of the minipig mandible. J Oral Maxillofac Surg. 2005; 64:249.
96. Troulis, MJ, Tayebaty, FT, Papadaki, M, et al. Condylectomy and costochondral graft reconstruction for treatment of active idiopathic condylar resorption. J Oral Maxillofac Surg. 2008; 66:65–72.
97. Troulis, MJ, Williams, WB, Kaban, LB. Endoscopic condylectomy and costochondral graft reconstruction of the ramus condyle unit. J Oral Maxillofac Surg. 2003; 61:63.
98. Troulis, MJ, Williams, WB, Kaban, LB. Endoscopic mandibular condylectomy and reconstruction: Early clinical result. J Oral Maxillofac Surg. 2004; 62:460.
99. Tsai, CL, Liu, TK, Chen, TJ. Estrogen and osteoarthritis: A study of synovial estradiol and estradiol receptor binding in human osteoarthritic knees. Biochem Biophys Res Commun. 1992; 183:1287.
100. Tuinzing, DB. Diagnosis and management of condylar resorption [discussion]. J Oral Maxillofac Surg. 1997; 55:119.
101. Umemura, Y, Ishiko, T, Yamaguchi, M, et al. Five jumps per day increase bone mass and breaking force in rats. J Bone Miner Res. 1997; 12:1480.
102. Van Strijen, PJ, Breuning, KH, Becking, AG, et al. Condylar resorption following distraction osteogenesis: A case report. J Oral Maxillofac Surg. 2001; 59:1104.
103. Vidra, MA, Rozema, FR, Kostense, PJ, et al. Observer consistency in radiographic assessment of condylar resorption. Oral Surg Oral Med Oral Path Oral Radiol Endod. 2002; 93:399.
104. Wanman, A. Longitudinal course of symptoms of craniomandibular disorders in men and woman: A 10-year followup study of an epidemiologic sample. Acta Odontol Scand. 1996; 54:337–342.
105. Weiss, JE, Ilowite, NT. Juvenile Idiopathic Arthritis. Pediatr Clin N Am. 2005; 52:413–442.
106. Will, LA, West, RA. Factors influencing the stability of the sagittal split osteotomy for mandibular advancement. J Oral Maxillofac Surg. 1989; 47:813.
107. Wolford, LM. Concomitant temporomandibular joint and orthognathic surgery. J Oral Maxillofac Surg. 2003; 61:1198–1204.
108. Wolford, LM, Cardenas, L. Idiopathic condylar resorption: Diagnosis, treatment protocol, and outcomes. Am J Orthodon Dentofacial Orthop. 1999; 116:667–677.
109. Wolford, LM, Chemallo, PD, Hilliard, FW. Occlusal plane alteration in orthognathic surgery. J Oral Maxillofac Surg. 1993; 51:730.
110. Wolford, LM, Cottrell, DA, Henry, CH. Temporomandibular joint reconstruction of the complex patient with the Techmedica custom-made total joint prosthesis. J Oral Maxillofac Surg. 1994; 52:2–10.
111. Wronski, TJ, Dann, LM, Scott, KS, et al. Endocrine and pharmacological suppressors of bone turnover protect against osteopenia in rats. Endocrinology. 1989; 125:810.
112. Yamada, K, Hanada, K, Fukui, T, et al. Condylar bony change and self-reported parafunctional habits in prospective orthognathic surgery patients with temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 92:265.
113. Yasuoka, T, Nakashima, M, Okuda, T, et al. Effect of estrogen replacement on temporomandibular joint remodeling in ovariectomized rats. J Oral Maxillofac Surg. 2000; 58:189.