CHAPTER 8 Identifying Bone Metastases
The most common site of distant metastasis from breast cancer is bone. In a study of almost 600 patients dying of breast cancer, Coleman and Rubens found that 69% had radiologic evidence of bone metastases before death.1 These results antedated use of fluorodeoxyglucose (FDG) positron emission tomography (PET), suggesting the true incidence might be even higher. Bone metastases in breast cancer may be osteolytic, osteoblastic, or mixed blastic and lytic. This feature accounts for the variable sensitivity and specificity of different imaging modalities.2 Of interest is that patients with blastic (versus osteolytic) bone metastases have been reported to have prolonged survival.3
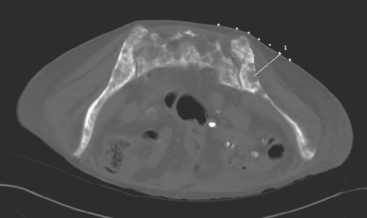
Plain radiographs require 30% to 50% loss of bone mineral to visualize a metastasis.4 Most breast cancer bone metastases demonstrate areas of lysis and sclerosis. Lesions can be permeative, moth-eaten, or geographic (Figure 1). Permeative and moth-eaten lesions predominate, whereas geographic lesions, exhibiting a sharp delineation between normal and abnormal bone, typically reflect a less aggressive metastasis.5 Advantages of plain radiography include widespread availability, minimal imaging time, absence of patient preparation, favorable radiation dosimetry, and relatively low cost. Based on the higher sensitivity of nuclear medicine bone scintigraphy, as well as its ability to survey the whole body, plain radiographs are now typically used to add specificity or to clarify bone scan findings.
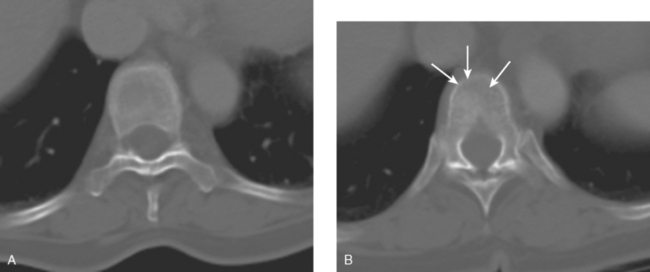
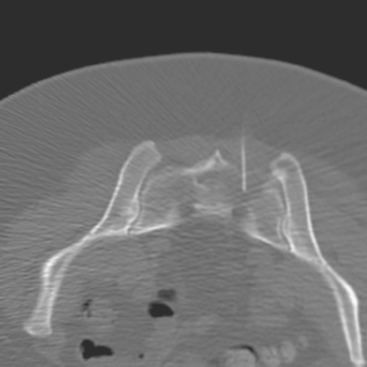
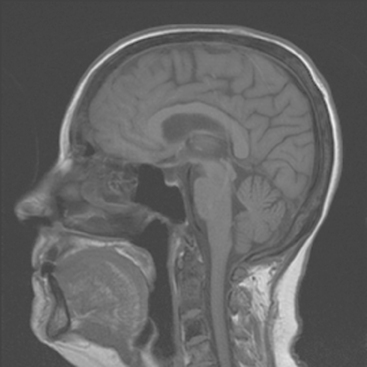
CT and MRI offer superb spatial resolution combined with excellent specificity. Nearly 50% of patients who are identified as having bony metastases on scintigraphy with negative plain radiographs will have detectable lesions on CT.6 Additionally, CT and MRI may be quite helpful in determining the etiology of bone pain (e.g., concomitant fracture, arthritis, soft tissue pathology). These modalities are preferred to answer questions related to a specific area (e.g., CT for ribs, MRI for vertebral column) (Figure 2). However, the nuclear medicine bone scan remains the procedure of choice for whole-body screening.7,8
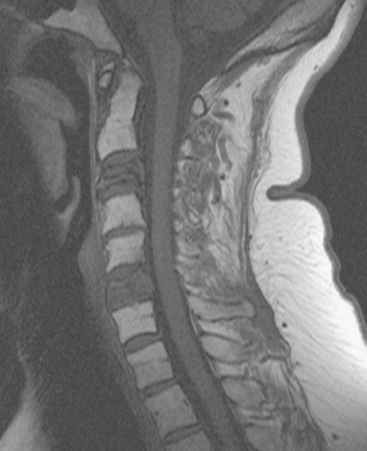
FIGURE 2 Same patient as in Figure 1. Sagittal T1-weighted, cervical spine MRI shows replacement of normal bright, fatty marrow signal in the C3 and C6 vertebral bodies, which show loss of height and end-plate invagination. The uniformly bright marrow signal elsewhere in the spine reflects prior radiation therapy.
Bone scintigraphy has withstood the test of time and is very sensitive in identifying areas of osteoblastic change. Findings on scintiscan may antedate findings on plain radiographs by many months. The bone scan is widely available, requires minimal patient preparation (increased fluid intake is recommended), delivers low radiation, and is cost effective. Disadvantages include reduced sensitivity in the vertebral column (improved with the use of single-photon emission computed tomography, or SPECT), significantly reduced sensitivity for purely osteolytic lesions, and suboptimal specificity. Routine bone scanning in patients with early-stage breast cancer, in the absence of symptoms, is not recommended.9
Bone scanning can also be performed with the positron emitter 18F sodium fluoride (NaF). Schirrmeister has published extensively on the use of 18F sodium fluoride and has shown high sensitivity and specificity in multiple tumor types, including breast.10–14 Compared with 99mTc-labeled polyphosphonates, 18F sodium fluoride shows about twice the uptake as well as a significantly improved target-to-background ratio. Current PET and PET/CT scanners provide improved sensitivity, higher spatial resolution, and tomographic capability (Figures 3 and 4).
Uptake of NaF is not tumor specific. Therefore, both benign and malignant lesions will demonstrate NaF uptake. Current PET/CT scanners, with improved spatial resolution and precise anatomic localization of lesions, result in better differentiation of benign from malignant lesions.14
There does not appear to be enough scientific data or clinical experience to recommend the routine use of NaF bone scintigraphy over FDG PET or bone scintigraphy. NaF may be helpful in selected patients; however, FDG PET is an accepted modality for use as a whole-body screen, can reliably detect primary tumors, and allows accurate assessment of soft tissue metastases.15–17
18F fluorodeoxyglucose (FDG) is the current radiopharmaceutical of choice for PET imaging in cancer. FDG enters tumor cells via glucose transporter proteins on the cell membrane and, once intracellular, is trapped. Uptake of FDG in bone metastases is incompletely understood; however, it has been shown that uptake in osteolytic metastases may be up to 7 times higher than osteoblastic metastases.18 Blastic metastases may not be demonstrated on FDG PET (Figure 5). Most studies comparing bone scintigraphy and FDG PET suggest an advantage for FDG PET with respect to osteolytic metastases and specificity. Bone scintigraphy appears to be more sensitive for osteoblastic lesions, and the two studies are best viewed as complementary.
An important area of bone metastases is the spinal column. A patient’s quality of life can be dramatically affected by metastases to the spine.19 Available imaging modalities include plain radiography, MRI, and CT. PET/CT has gained popularity because of its ability to combine metabolic and anatomic data. Frontal, lateral, and dynamic plain films (e.g., flexion and extension views) are helpful in identifying instability. Neural compression is best evaluated with MRI. The presence and extent of metastases are well delineated by altered signal within bone. Bony anatomy is best defined by thin-section axial CT. Contrast enhancement is helpful in enhancing tumor visualization and more clearly defining neural compression.
1 Coleman RE, Reubens RO. The clinical course of bone metastases from breast cancer. Br J Cancer. 1987;55:61-66.
2 Even-Sapir E. Imaging of malignant bone involvement by morphologic, scintigraphic, and hybrid modalities. J Nucl Med. 2005;46:1356-1367.
3 Yamashita K, Koyama H, Inaji H. Prognostic significance of bone metastasis from breast cancer. Clin Orthop. 1995;312:89-94.
4 Edelstyn GA, Gillespie PJ, Grebell FS. The radio-logical demonstration of osseous metastases: experimental observations. Clin Radiol. 1967;18:158-162.
5 Wittig JC, Lamont JG. Bone metastases from breast cancer. In: Roses DF, editor. Breast Cancer. Phil-adelphia: Elsevier Churchill Livingstone; 2005:666-675.
6 Muindi J, Coombes RC, Golding S, et al. The role of computed tomography in the detection of bone metastases in breast cancer patients. Br J Radiol. 1983;56:233-239.
7 Hamaoka T, Madewell JE, Podoloff DA, et al. Bone Imaging in metastatic breast cancer. J Clin Oncol. 2004;22:2942-2953.
8 Love C, Din AS, Tomas MB, et al. Radionuclide bone imaging: an illustrative review. RadioGraphics. 2003;23:341-358.
9 Yeh KA, Fortunato L, Ridge JA, et al. Routine bone scanning in patients with T1 and T2 breast cancer: a waste of money. Ann Surg Oncol. 1995;2:319-324.
10 Schirrmeister H, Guhlmann CA, Elsner K, et al. Planar bone imaging vs 18 F-PET in patients with cancer of the prostate, thyroid and lung. J Nucl Med. 1999;40(10):1623-1629.
11 Schirrmeister H, Guhlmann CA, Kotzerke J, et al. Early detection and accurate description of extent of metastatic bone disease in breast cancer with 18F-fluoride ion and positron emission tomography. J Clin Oncol. 1999;17(8):2381-2389.
12 Schirrmeister H, Glatting G, Hetzel J, et al. Prospective evaluation of the clinical value of planar bone scans, SPECT and F-18 labeled NaF PET in newly diagnosed lung cancer. J Nucl Med. 2001;42(12):1800-1804.
13 Schirrmeister H. Detection of bone metastases in breast cancer by positron emission tomography. PET Clinics: Breast Cancer. 2006;1(1):25-32.
14 Schirrmeister H, Diedrichs CG, Rentschler M, et al. Positron-emission tomography of the skeletal sys-tem using 18-F Na: the incidence, pattern of the findings and distribution of benign changes. Fortschr Rontgenstr. 1998;169(3):310-314. (in German)
15 Crippa F, Agresti R, Seregni E, et al. Prospective evaluation of fluorine–18-FDG PET in presurgical staging of the axilla in breast cancer. J Nucl Med. 1998;39(1):4-8.
16 Moon DH, Maddahi J, Silverman DHS, et al. Accuracy of whole body fluorinie-18 FDG PET for the detection of recurrent or metastatic breast carcinoma. J Nucl Med. 1998;39(3):431-435.
17 Even-Sapir E, Mester U, Flusser G, et al. Assessment of malignant skeletal disease: initial experience with 18F-fluoride PET/CT and comparison between 18F-fluoride PET and 18F-fluoride PET/CT. J Nucl Med. 2004;45(2):272-278.
18 Cook GJ, Houston S, Rubens R, et al. Detection of bone metastases in breast cancer by 18 FDG PET: differing metabolic activity in osteoblastic and osteolytic lesions. J Clin Oncol. 1998;16(10):3375-3379.
19 Douglas AF, Cooper PR. Spinal column metastases from breast cancer. In: Roses DF, editor. Breast Cancer. Philadelphia: Elsevier Churchill Livingstone; 2005:644-652.
CASE 1 Stage IV presentation of breast cancer with bone metastases
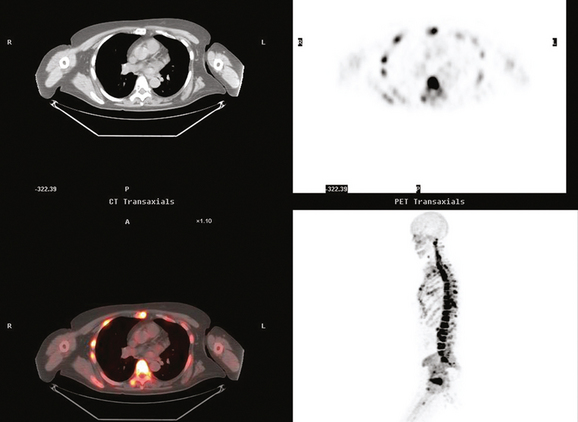
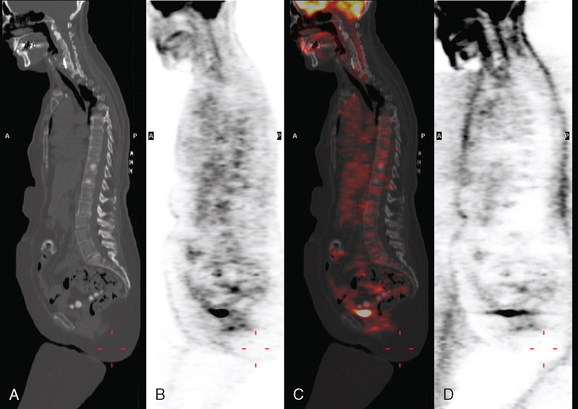
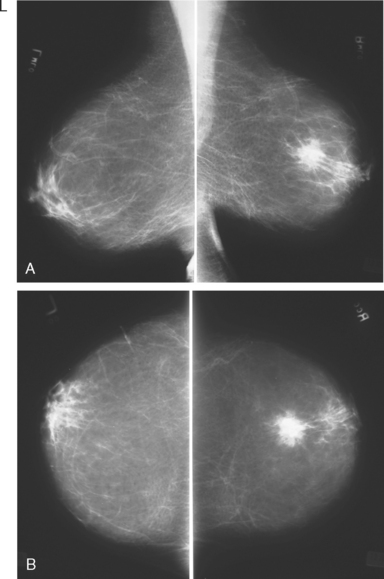
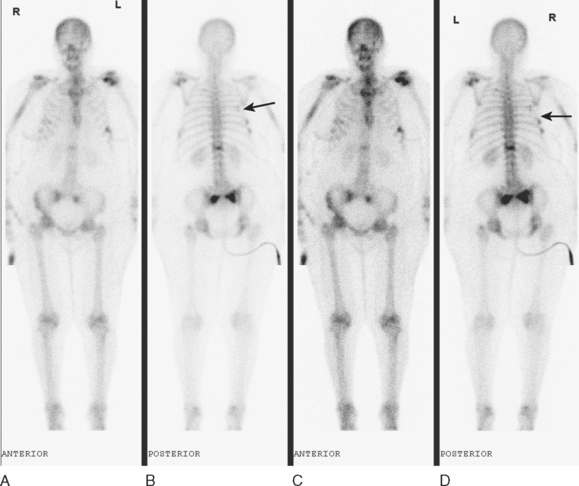
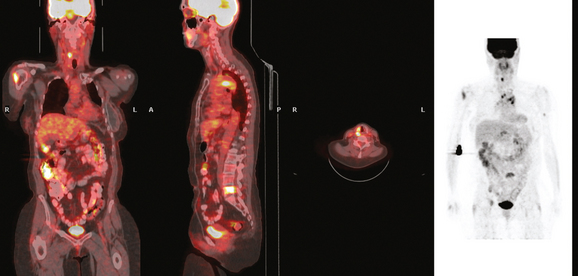
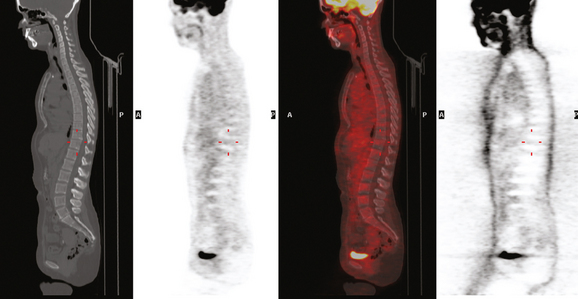
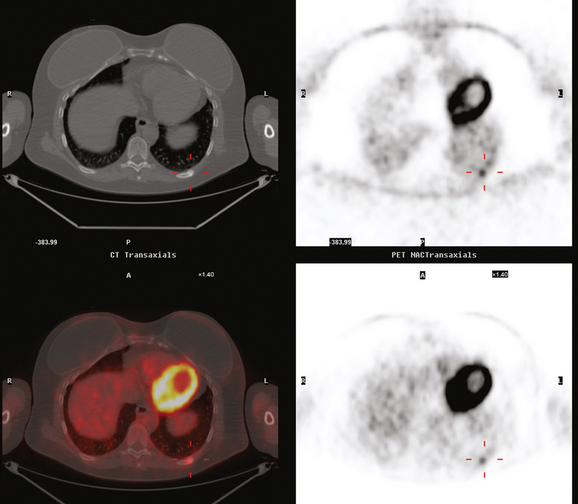
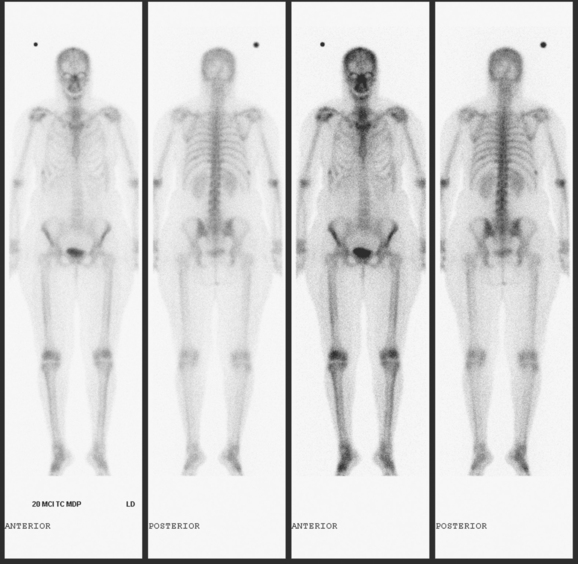
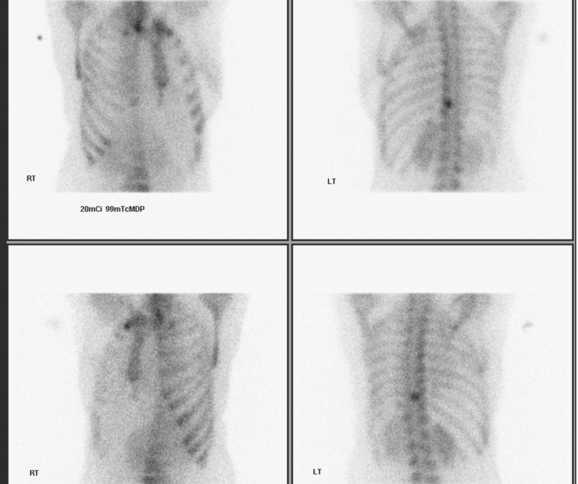
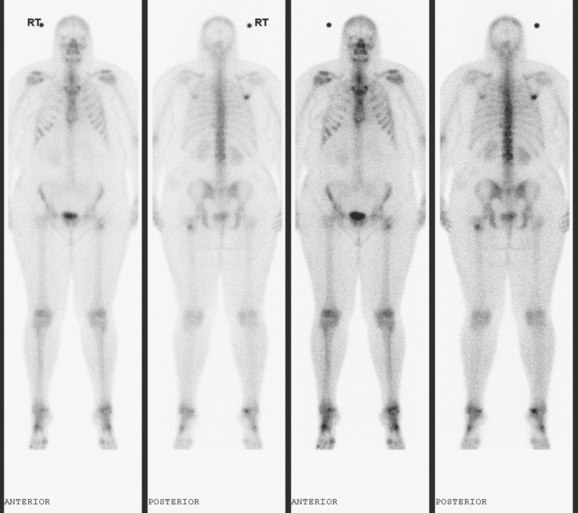
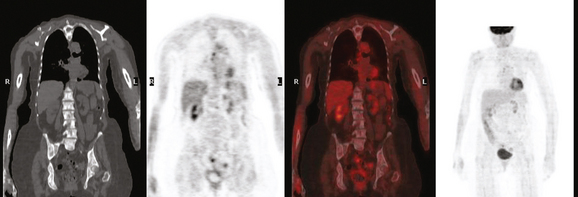
A 60-year-old woman presented with a large, palpable right breast mass (same patient as in Case 19 in Chapter 4). Imaging workup, including mammography, ultrasound, breast MRI, and ultrasound-guided core needle biopsy and axillary lymph node aspiration, confirmed node-positive multifocal infiltrating ductal carcinoma (IDC). Based on physical examination, the patient was thought to have an advanced breast cancer, at least T3 by size, and she was started on neoadjuvant chemotherapy while her staging workup was completed. The staging evaluation included a bone scan and positron emission tomography (PET)/CT. The bone scan, obtained before starting chemotherapy, showed several foci of increased activity, including in the left anterior third rib, one focus each in the cervical and thoracic spine, and a focus at the left upper sacroiliac joint region (Figure 1). A breast MRI, obtained a few days after the first round of chemotherapy, included a coronal short tau inversion recovery (STIR) series of the thorax, obtained with the body coil. This showed evidence of widespread bone metastases, with hyperintense foci in the right medial clavicle and in a lower thoracic vertebral body (Figure 2). A PET/CT scan was performed about 1 week after the first cycle of chemotherapy. In addition to showing hypermetabolism of the multifocal breast carcinoma, hypermetabolic foci were identified in multiple bony sites, including the right clavicular head, right upper cervical spine, two adjacent lower thoracic vertebrae, the left medial iliac crest, and a left anterior rib (Figure 3). These sites of abnormal activity overlapped in distribution with the abnormalities noted previously on limited chest MRI and the prechemotherapy bone scan. No definite correlates were found at these sites on CT. Thus, as the staging was completed in this patient, it became apparent that what was initially thought to be T3N1 disease (stage IIIA) was actually stage IV disease.
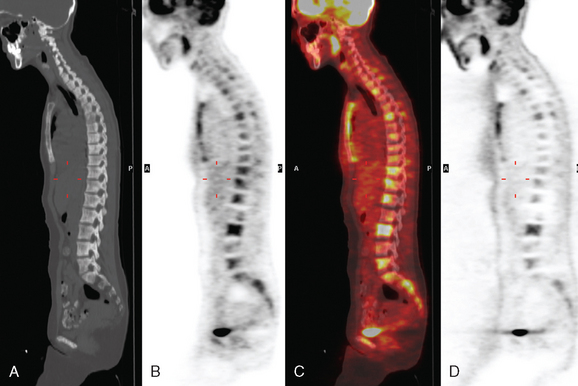
After one cycle of chemotherapy, CT scanning was repeated. The large breast mass and axillary adenopathy showed improvement, and new sclerosis was now evident at several levels in the spine (Figure 4).
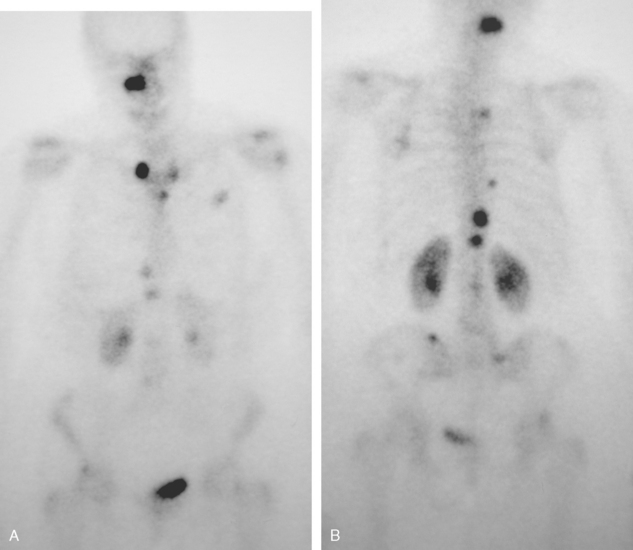
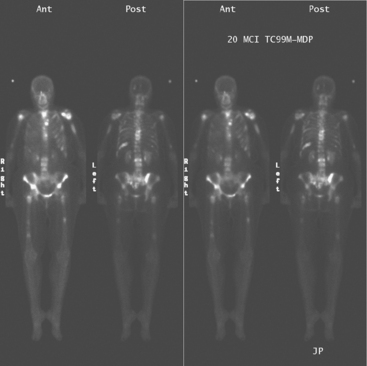
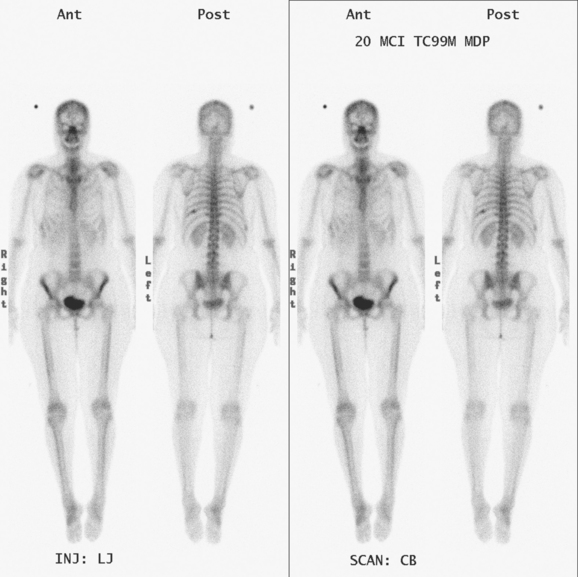
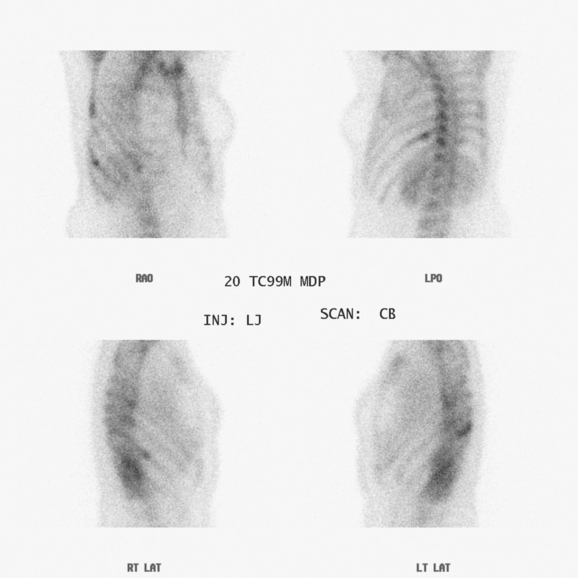
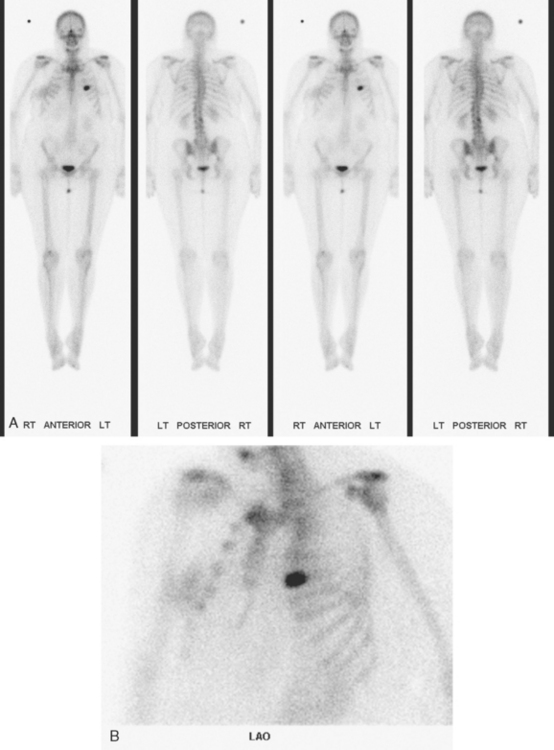
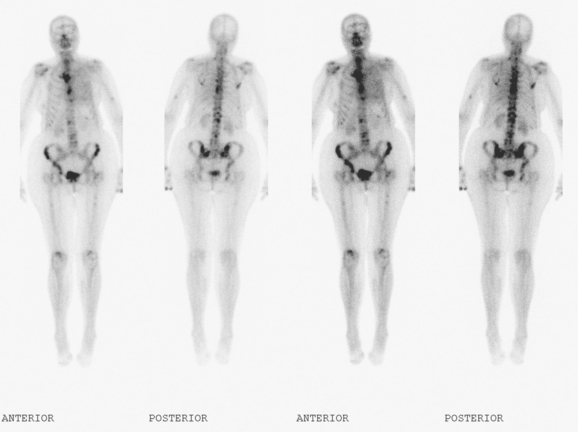
Before undergoing repeat bone scanning and spine MRI, a second cycle of chemotherapy was given. The repeat bone scan, obtained 1 month after the prechemotherapy study, showed an increase in number of foci of increased activity (Figure 5). Several preexisting foci of activity appeared larger and more intensely active. MRI of the lumbar spine showed multiple areas of abnormal signal intensity, at levels corresponding to the prior bone and PET scans (Figure 6).
Two weeks after surgery, CT-guided sampling of the sclerotic T11 lesion was performed and did not confirm metastatic disease. The needle biopsy was repeated 2 months later, confirming metastasis. A nearly concurrent repeat PET/CT for restaging had normalized (Figure 7).
TEACHING POINTS
The initial bone scan, obtained before starting chemotherapy, was abnormal, although not definitively diagnostic of bone involvement. Without imaging correlation, provided subsequently by a limited chest MRI, a number of the bone scan findings could have been accounted for by other explanations. The rib lesion, for example, could have been post-traumatic, and a possible trauma history was elicited from the patient. The activity is less punctate than generally seen with fractures, but a long segment of involvement, which would more compellingly suggest neoplasia, is not seen either. The patient had had prior cervical spine surgery, raising the possibility of accelerated de-generative change at an adjacent level. At the same time, the activity in both the cervical and thoracic levels is disturbingly focal and relatively intense. Degenerative findings frequently involve multiple adjacent levels and, unless actively degenerating, are often less intense in activity than the findings seen here.
What is the significance of the apparent increase in disease seen on the second bone scan, performed 1 month later, after two cycles of chemotherapy? Does this mean the metastases are progressing? Not necessarily. In fact, the changes we see between these two bone scans are an excellent example of the flare phenomenon, whereby a patient responding to hormonal therapy or chemotherapy may actually appear worse on bone scanning. Increased activity of previously identified lesions and even new lesions may be seen (as in this case). Recall that it is the osteoblastic response to a bone abnormality (neoplastic, infectious, or traumatic) that we see as an increase in activity on a bone scan. Metastases that are initially lytic may become sclerotic in response to treatment, and this is demonstrated in this case on the PET/CT. The hypermetabolic bone foci that were seen on the initial PET/CT were without a clear CT correlate (indicating they were lytic) but became sclerotic (within 3 weeks, after one cycle of chemotherapy!) and readily visible on the CT portion of the follow-up PET/CT, at which time the PET activity had resolved. This does not mean the patient is cured or that the disease is not active. This patient had biopsy confirmation of metastatic involvement of T11, concurrent with normalization of PET scan activity. This constellation of findings reflects the reality that initially lytic bone metastases, best seen on PET imaging, responded to treatment by developing sclerosis. In the process, the bone metastases became increasingly visible on CT and bone scan, and inactive on PET.
CASE 2 Stage IV presentation with bone metastases (breast cancer presenting with back pain)
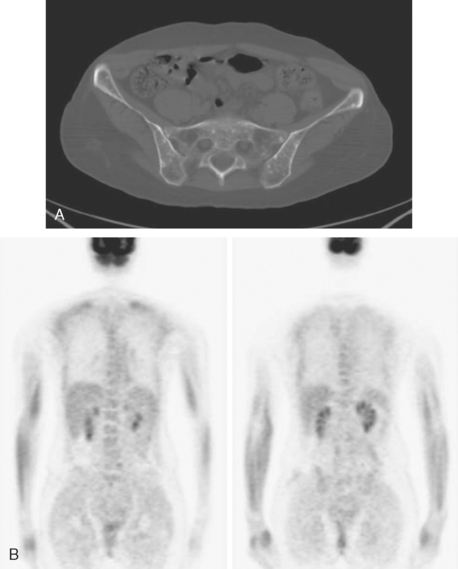
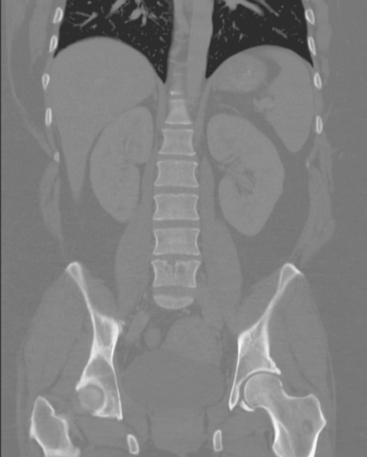
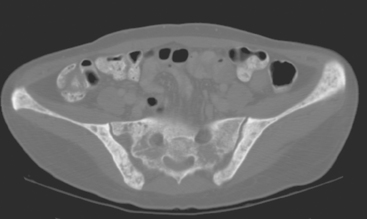
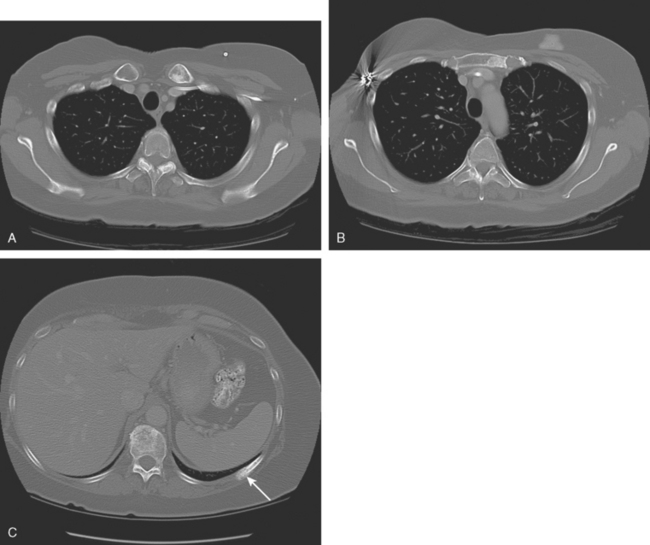
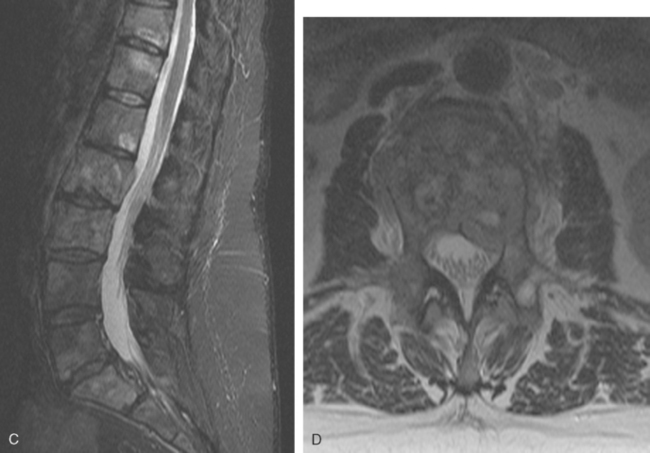
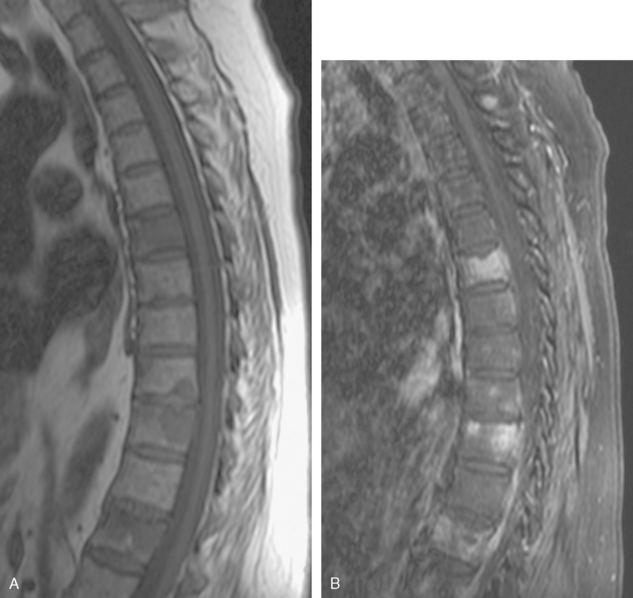
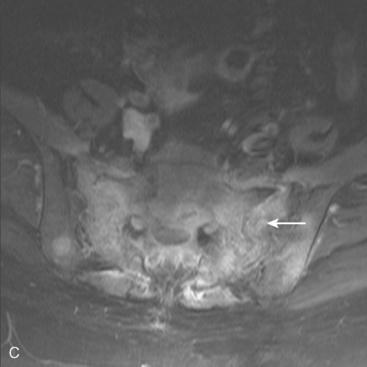
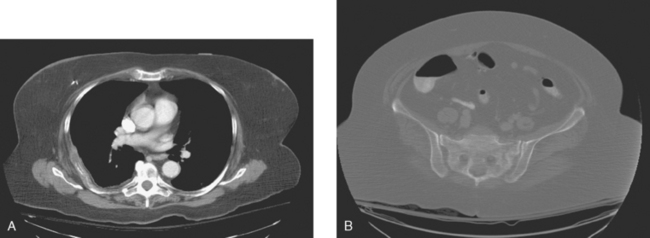
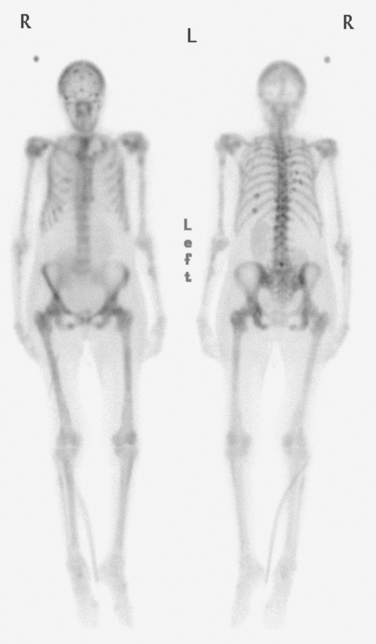
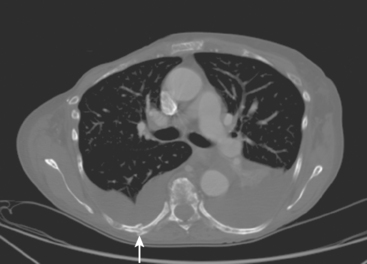
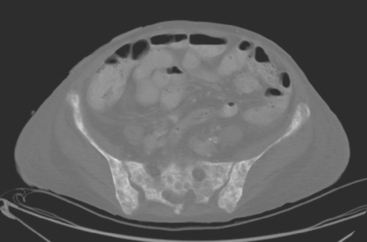
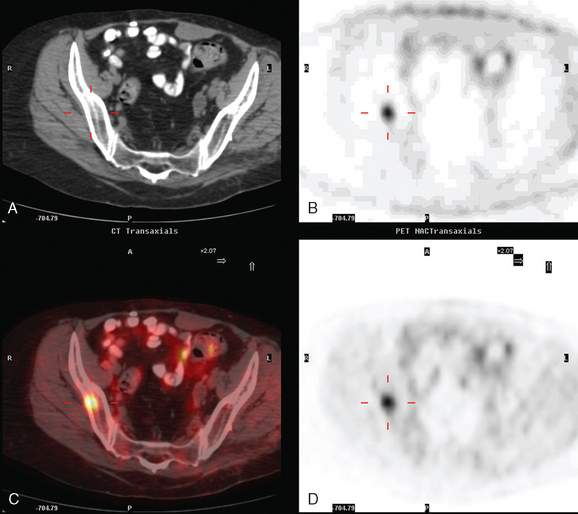
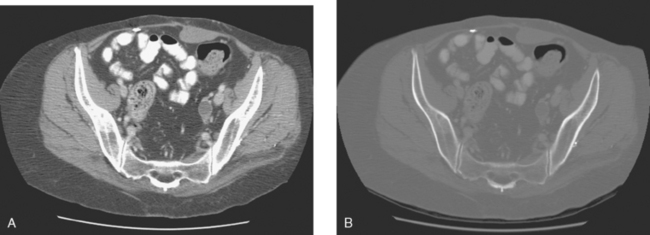
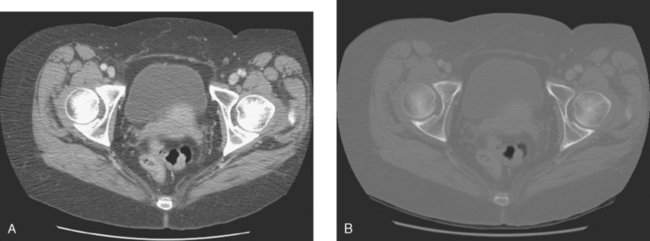
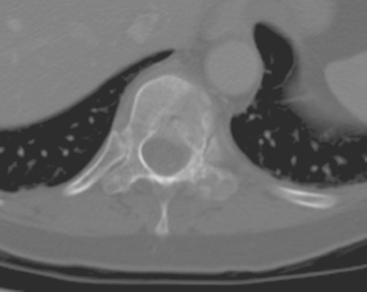
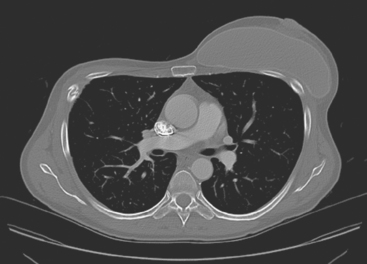
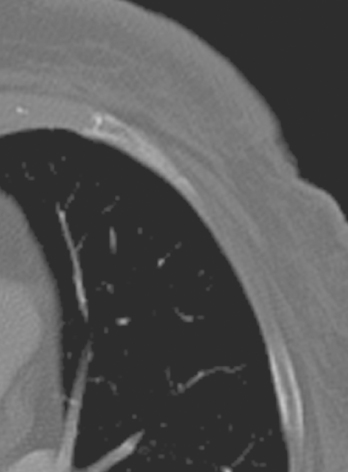
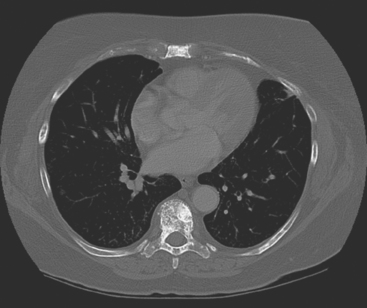
A 35-year-old obese woman presented with severe low back, knee, and hip pain and 5 days of intermittent fever up to 102 degrees. She was evaluated with abdominal, pelvic, and lumbar spine CT scans for suspicion of a spinal infection. These studies showed multiple lytic lesions in bone, including the L5 vertebral body, and left sacrum, ilium, and proximal femur (Figures 1, 2, 3, and 4). Bony metastatic disease was suspected, and a lung primary was sought with a chest CT. This showed a 2-cm spiculated right breast mass, suspicious for a breast cancer primary (Figure 5).
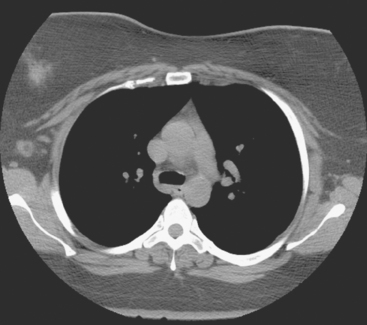
FIGURE 5 Axial unenhanced chest CT image shows a central right breast mass in largely fatty breasts.
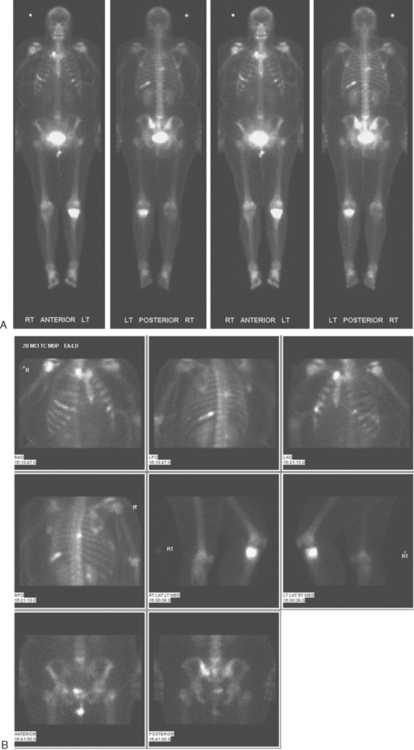
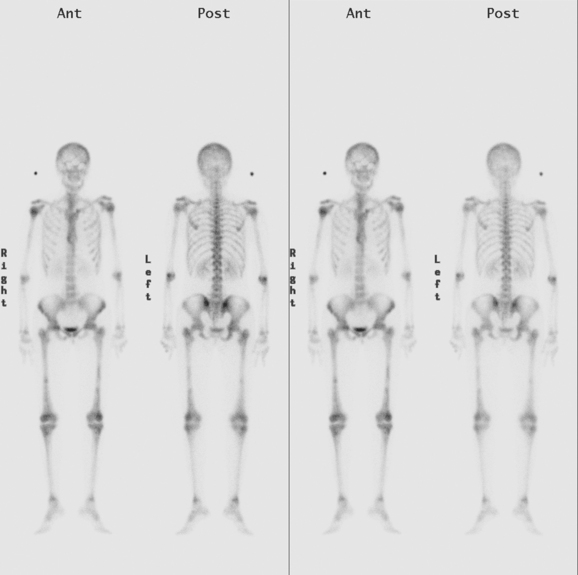
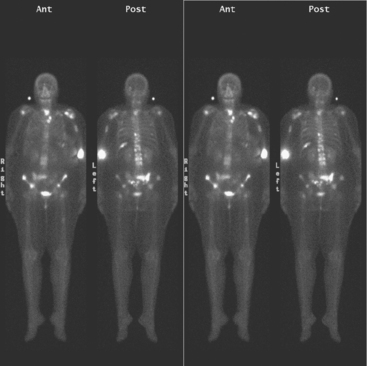
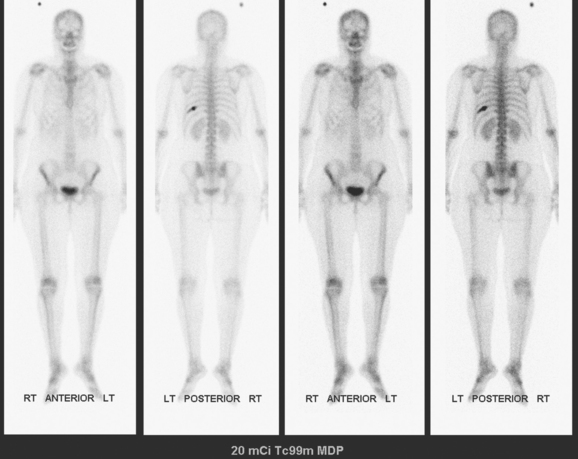
Bone scan showed corresponding, highly suspicious, multifocal findings suggesting bone metastases (Figure 6).
Breast imaging workup with diagnostic mammography, breast ultrasound, and ultrasound-guided core needle biopsy confirmed right breast cancer. The mammogram showed a dominant, central, 5-cm spiculated mass (Figure 7). Ultrasound showed a corresponding irregular hypoechoic mass in the retroareolar region, with a separate 1.7-cm suspicious shadowing focus in the upper outer quadrant (UOQ) (Figures 8 and 9). A suspicious axillary lymph node was also noted, with mild cortical mantle thickening (Figure 10).
Histologic sampling of the breast masses confirmed infiltrating ductal carcinoma (IDC) from both sites, estrogen receptor and progesterone receptor positive, and HER-2/neu positive. Fine-needle aspiration of the axillary lymph node demonstrated metastatic carcinoma.
CT-guided sampling of a lucent sacral lesion showed metastatic adenocarcinoma, consistent with breast primary (Figure 11).
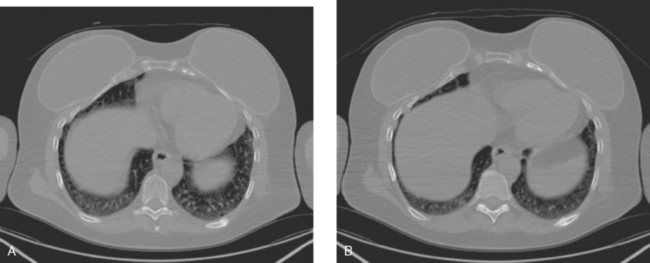
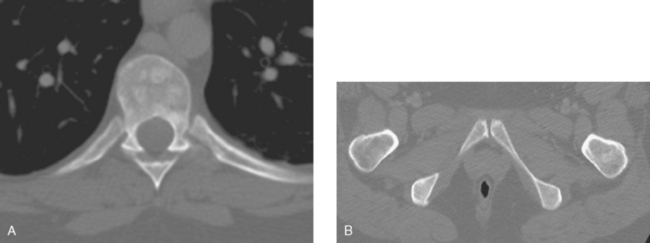
Palliative radiation therapy to the lumbar spine (L5 and sacroiliac region) and left knee were given for pain relief, and the patient was started on tamoxifen and zoledronic acid (Zometa). Repeat CT images, 7 months later, show a variety of bone responses to these interventions (Figure 12).
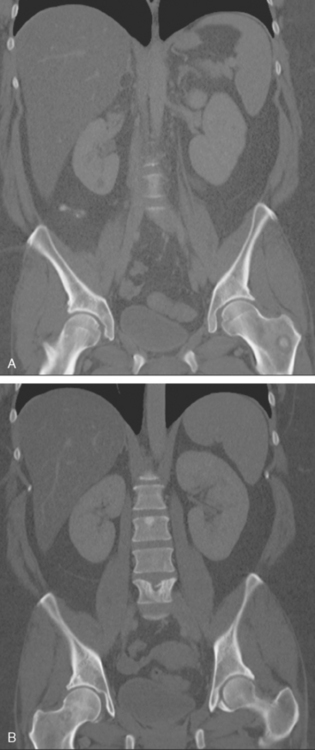
FIGURE 12 Coronal CT reconstructions (A anterior to B), 7 months after initial CT in Figure 4, after lumbar spine radiation, and treatment with tamoxifen and Zometa. In A, the left intertrochanteric metastasis has grown. It now displays a dominant central sclerotic component, with a lucent rim. In B, the lytic focus at the superior end plate of L5 remains visible, but now shows a thick surrounding blastic response. At the superior end plate of L3, a blastic lesion is now seen. This may reflect healing of a subradiographic lytic metastasis.
TEACHING POINTS
This is a distinctly unusual presentation of breast cancer, with symptomatic bone metastases bringing this pre-screening-age patient with no notable family history to attention. Less than 10% of breast cancer patients present with stage IV disease. This patient’s primary tumor was also identified through an unusual route, being first seen on a chest CT. Breast cancers can certainly be picked up initially on chest CT, which usually is performed for other reasons. (See Case 15 in Chapter 1 for another example.) For this reason, CT interpreters should always scrutinize chest wall soft tissues and breasts as part of their routine search pattern.
CASE 3 Relapse with bone metastases
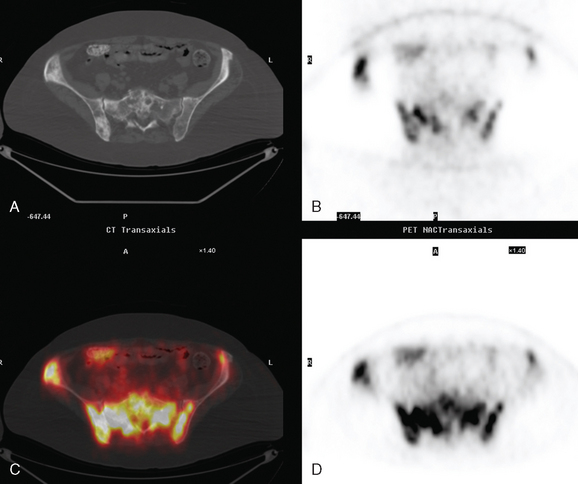
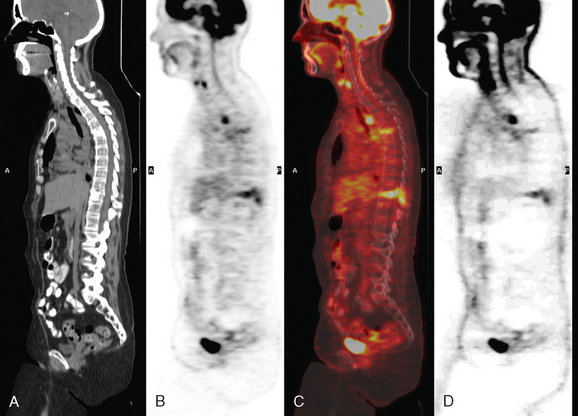
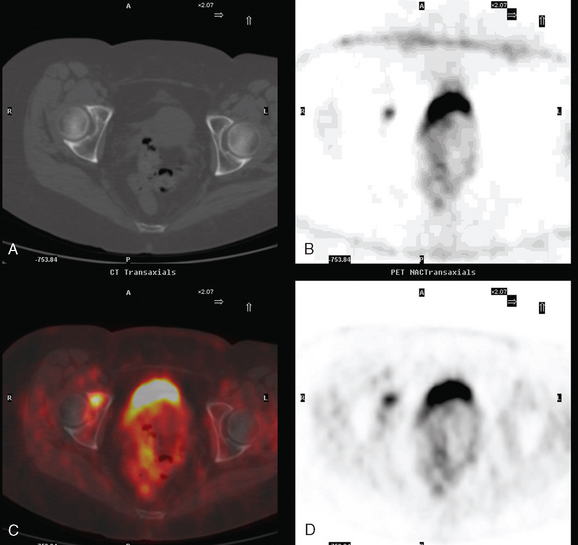
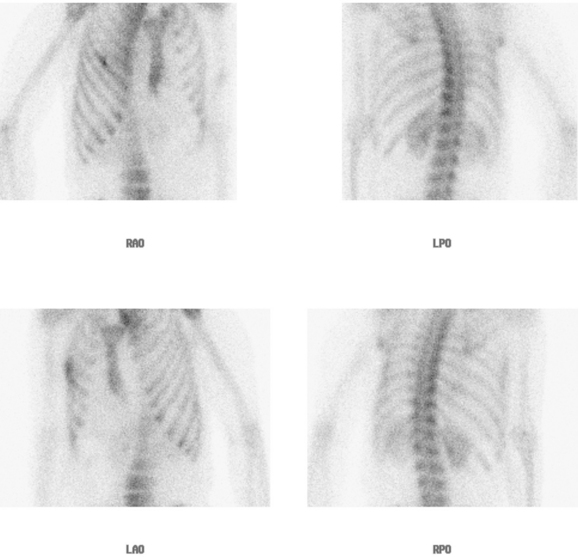
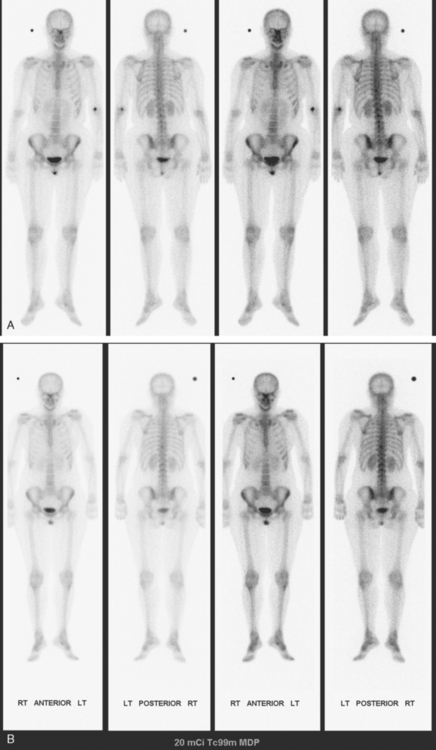
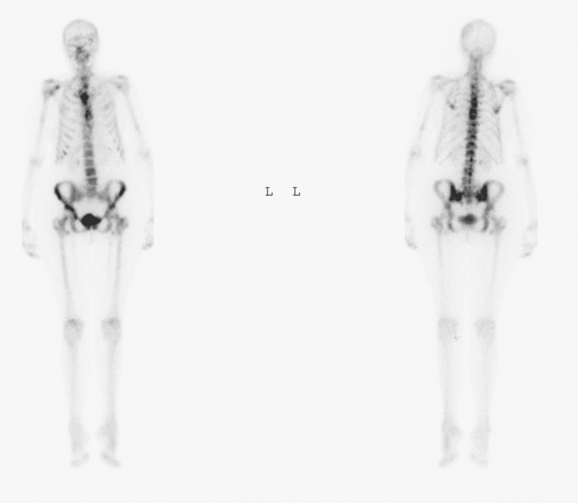
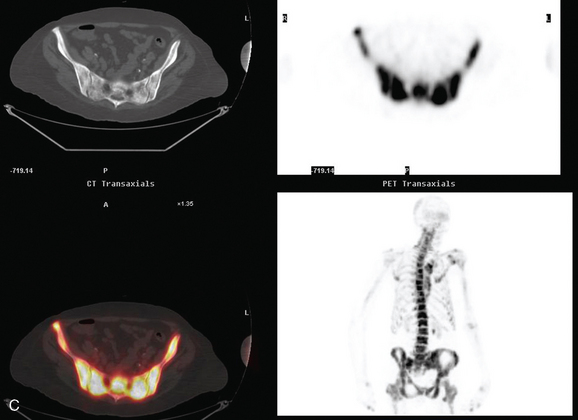
A pelvis x-ray was abnormal, with a moth-eaten appearance of the right ischium (Figure 1). Subsequent evaluations with pelvis and lumbar spine MRI, body CT scans, positron emission tomography (PET), and bone scan suggested extensive bony metastases (Figures 2, 3, 4, and 5). A bone marrow aspirate confirmed metastatic breast cancer. The patient was placed on goserelin acetate (Zoladex), zoledronic acid (Zometa), and anastrozole (Arimidex).
A year later, while on Zoladex, Zometa, and exemestane (Aromasin), the patient was restaged with PET/CT for symptoms of increased aching, weight loss, depressed appetite, and rising tumor markers. PET/CT showed new liver metastases. Chemotherapy was recommended, but declined. The patient was started on fulvestrant (Faslodex). Restaging after 2 months, at which time the patient had fatigue, shortness of breath, and rising tumor markers, showed progression of liver metastases as well as evidence of lung involvement (see Case 13 in Chapter 10). She died a month later, 15 months after bony metastases were detected.
TEACHING POINTS
Higher in the hierarchy is bone scintigraphy. In most cancers, bone scans are 50% to 80% more sensitive than radiographs for detection of bone metastases. However, as in this case, there are instances in which bone scans can severely underestimate the extent of skeletal involvement (see also Case 5). A possible explanation is the very diffuse distribution, with such extensive involvement that there is essentially no normal intervening bone between lesions to increase the conspicuity of metastatic lesions. Such extensive bony metastases could result in a “superscan” pattern of diffuse increased skeletal activity, with high target-to–soft tissue ratio and minimal renal and bladder activity. In such scans, tracer uptake is so increased in the skeleton that less tracer is available to excrete through the urinary system. This bone scan does not demonstrate the classic features of a superscan, but shows some features in the spectrum of a superscan.
CASE 4 Progression of bone metastases, epidural extension, radiation therapy effects
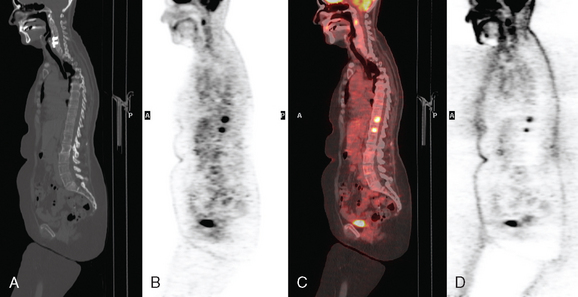
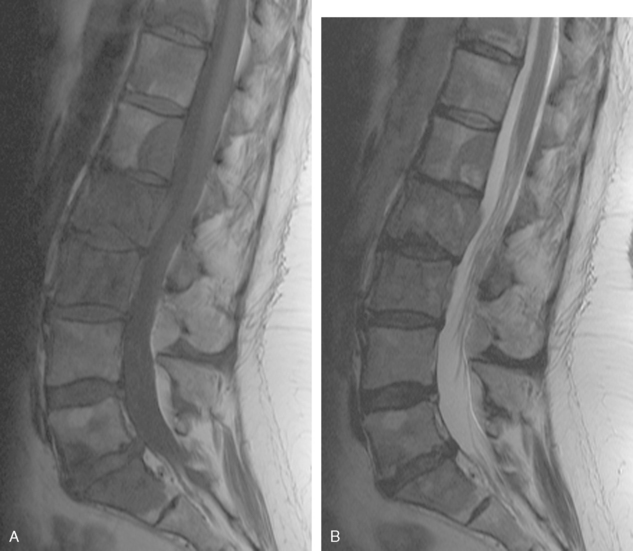
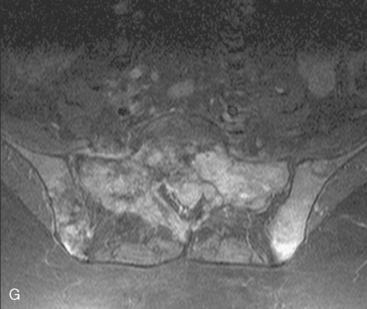
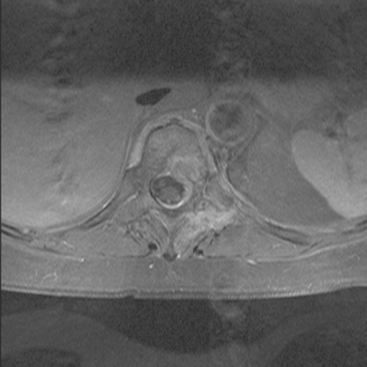
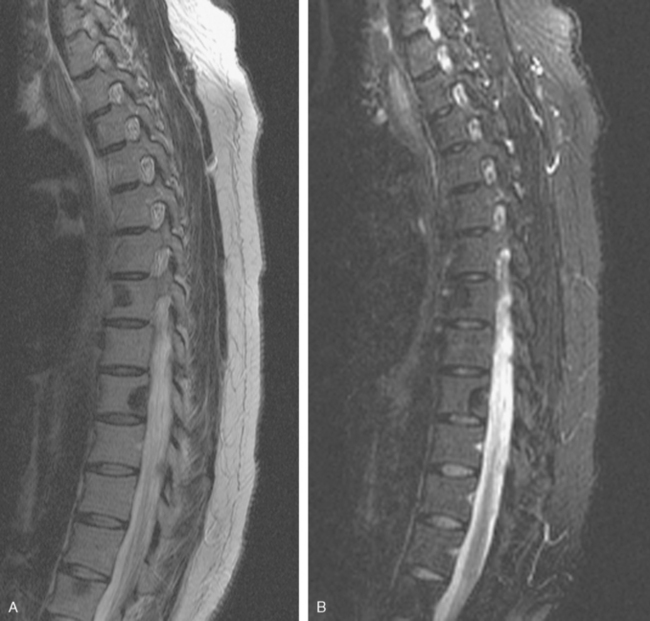
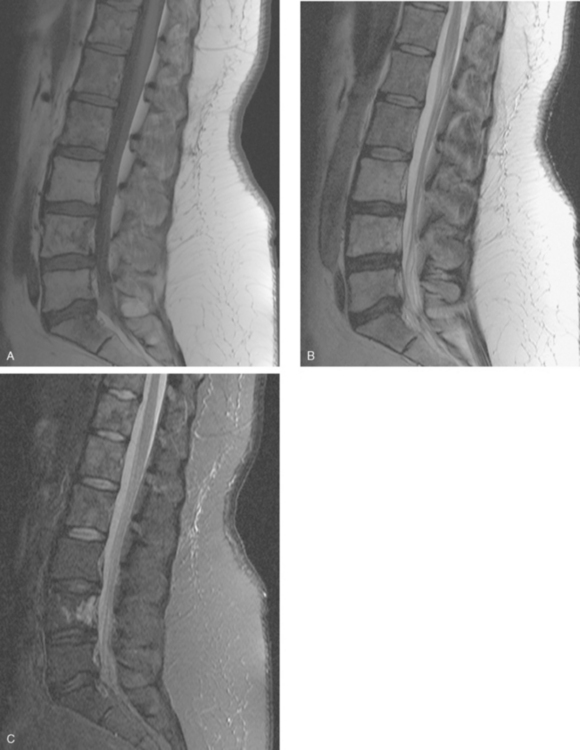
A 55-year-old woman with a remote history of treated breast cancer presented with breast recurrence and bone metastases. Her breast cancer history was 14 years earlier, a right T2N0 infiltrating ductal carcinoma (IDC), estrogen receptor and progesterone receptor positive, treated with lumpectomy and radiation. Tamoxifen had been declined. At this presentation with recurrent disease, her left breast showed firm hardening, partial nipple inversion, and peau d’orange. Core needle biopsy confirmed IDC. Increased right breast firmness and nipple retraction were also noted, as well as left supraclavicular fullness and nodularity. The patient noted right hip and back discomfort, and bone scan showed findings suspicious for bone metastases. Bone metastases were subsequently confirmed by lumbar spine MRI (Figures 1 and 2), and corresponding findings were noted on CT scans as well (Figure 3). The patient was placed on tamoxifen and monthly zoledronic acid (Zometa) after treatment with doxorubicin (Adriamycin) plus cyclophosphamide (Cytoxan) (AC) chemotherapy and monitored periodically with bone scans (Figures 4 and 5).
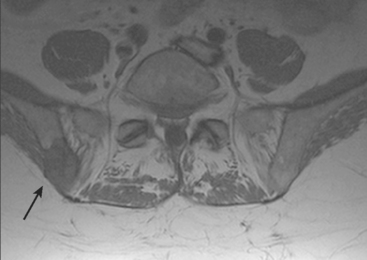
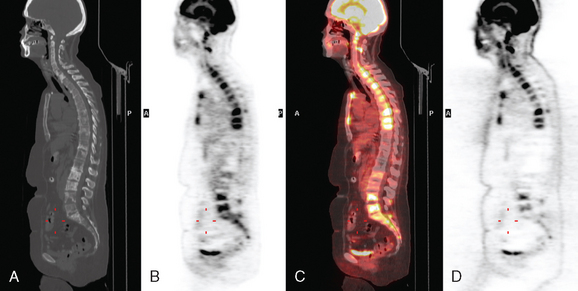
Four years after bone metastases were demonstrated, the patient was evaluated with PET, which showed multiple metabolically active bone lesions (Figures 6 and 7). At the time, the patient noted new left anterior thigh paresthesia, which progressed to excruciating. Lumbar spine MRI showed progression of bone metastases and new epidural disease at L2 (Figure 8). Radiation therapy was administered, with marked improvement in pain (Figure 9). The patient’s therapy at this time included exemestane (Aromasin) and Aredia.
Six months later, repeat spine MRI was obtained to evaluate new left leg sciatica. The patient noted increased fatigue, and her tumor markers were rising. Spine MRI showed progression of osseous metastases to near confluence (Figure 10). New epidural tumor was identified at the S1 level in the left lateral recess, explaining the patient’s symptoms. Chemotherapy was restarted, with docetaxel (Taxotere).
TEACHING POINTS
At this writing, reports of the use of whole-body MRI to identify bone metastases are appearing in the literature. Validation of this approach is ongoing, and in general today, MRI is used more selectively to image symptomatic regions or regions suspected based on other modalities to harbor metastatic disease. Bone metastases are identified on MRI as areas of marrow replacement. T1-weighted sequences are sensitive for the detection of bone metastases because in adults, the normal marrow signal on T1-weighted sequences will be bright because of yellow (fatty) marrow. The signal intensity of metastases on T2-weighted sequences can help separate lytic from sclerotic lesions, with lytic metastases being relatively bright on T2 and STIR and sclerotic metastases hypointense on all sequences. Use of contrast enhancement, particularly with fat saturation, is useful to assess epidural tumor extension.
PET findings of bony breast cancer metastases can be complementary to bone scintigraphy. PET is sensitive to active bone metastases, particularly lytic disease, but may underestimate sclerotic bone metastases, which are identifiable on scintigraphy (see Case 10 in this chapter).
Hattner RS, Hartmeyer J, Wara WM. Characterization of radiation-induced photopenic abnormalities on bone scans. Radiology. 1982;145:161-163.
Yankelevitz DF, Henschke CI, Knapp PH, et al. Effect of radiation therapy on thoracic and lumbar bone marrow: evaluation with MR imaging. AJR Am J Roentgenol. 1991;157:87-92.
CASE 5 Recurrence with bone metastases: Disease extent discordant between imaging and bone scan; pathologic fractures
Her laboratory data were abnormal at the time of presentation with hip pain, with elevated alkaline phosphatase and CA27.29. The patient was admitted with suspicion of metastatic disease. The workup included a head CT; brain and spine MRI; chest, abdomen, and pelvis CT; and bone scan. Head CT and MRI showed intracranial metastases. CT showed suspicious findings for liver and lung metastases. Bone metastases were shown on spine MRI (Figure 1), as well as on CT (Figure 2). Bone scan was abnormal, most notably for rib, verte-bral, and sacral fracture findings, but underrepresented the extent of diffuse osseous metastases (Figure 3).
TEACHING POINTS
The importance of imaging correlation when interpreting bone scans, PET scans, and other nuclear medicine studies cannot be overemphasized. Bone scans are highly variable in their depiction of metastases, depending on the size of the bone lesion, the location in the skeleton, and, importantly, the type of bone reaction incited (lytic, blastic, or mixed). There are patients with radiographic and imaging findings of extensive osseous metastases whose bone scans can appear deceptively benign. At first glance, the bone scan of this patient appears simply to be that of an elderly woman with typical scintigraphic findings of rib, vertebral compression, and sacral insufficiency fractures, with only subtle evidence on scintigraphy of metastatic disease as the etiology of the pathologic fractures. One of the most compelling findings on this bone scan for metastatic disease is the hardest to recognize: the cold lesion or absence of the destroyed right rib. With the roadmap provided by correlation with the CT, consequential oversights like this may be avoidable. At the same time, when presented with apparently discordant findings, the interpretation should reflect the fact that in individual patients, bone scintigraphy may not be the most accurate reflection of the full extent of osseous disease burden.
CASE 6 Diffuse bone metastases, underrepresented on bone scan
A 63-year-old woman was admitted from a rehabilitation center for evaluation of progressive anemia. She was recovering from an admission to another hospital for perforated ulcer, treated with gastrectomy. Her past medical history of right breast cancer was 7 years earlier, Stage 2, T1N2M0, treated with mastectomy, 6 months of adjuvant chemotherapy, and tamoxifen. A bone scan, performed for diffuse aches and bone pain, suggested metastatic disease as well as multiple fractures (Figure 1). Correlation with a concurrent body CT scan showed extensive bone mineral alterations of advanced and extensive osseous metastases, as well as multiple pathologic fractures (Figures 2 and 3). Metastatic adenocarcinoma, consistent with breast primary, was confirmed by CT-guided biopsy of a lytic focus in the left ilium (Figure 4).
TEACHING POINTS
Considerations in choosing a site for biopsy of a suspected bone metastasis include ease and safety of access (Can the patient lie prone? What structures might be injured?) and factors influencing the likelihood of obtaining adequate material (soft tissue replacing bone is easier to sample than bone forming tumor). In a case like this, in which there are diffuse changes, it makes sense to biopsy the pelvis, rather than risk a pneumothorax or neural injury sampling a rib or vertebral body. It is technically easier to obtain satisfactory material for analysis from a lytic bone metastasis than from sclerotic sites, when there is a choice.
CASE 7 Recurrence with mediastinal lymphadenopathy, vocal cord paralysis, and sclerotic bone metastases
Oncologic evaluation included tumor markers, which were elevated (CEA and CA27.29). Positron emission tomography (PET) and CT imaging showed hypermetabolic mediastinal and hilar adenopathy and bone metastases (Figures 1, 2, 3, 4, 5, and 6). The patient had been noted to be hoarse on physical examination, and PET showed asymmetrical muscular activity of the vocal cords. Metastases in the spine were further evaluated with MRI to assess epidural tumor extension (Figures 7, 8, 9, and 10).
TEACHING POINTS
Development of musculoskeletal symptoms is a clear clinical indication for restaging of a breast cancer patient. Systemic metastases occur most commonly to bone and are seen in up to one third of patients with recurrent disease. Traditionally, new focal pain would be evaluated with a radiograph of the joint or extremity, with the entire skeletal system surveyed with bone scintigraphy. Today, bone scanning is still indicated as a cost-effective modality, which is particularly efficacious in identifying sclerotic metastases. If bone scanning does not provide an explanation for new symptoms, PET/CT may be indicated as the next imaging step for a highly sensitive comprehensive total-body evaluation for soft tissue and lytic bony metastases.
CASE 8 Significance of solitary rib activity on bone scan; chemotherapy-related marrow activation changes on PET
When the patient developed constitutional symptoms, she was restaged with CT scans, which showed extensive hepatic metastases. Chemotherapy with carboplatin, docetaxel (Taxotere), and trastuzumab (Herceptin) was initiated, with good response. Later the same year, brain metastases were identified, and treated with whole brain radiation therapy, with MRI resolution of lesions.
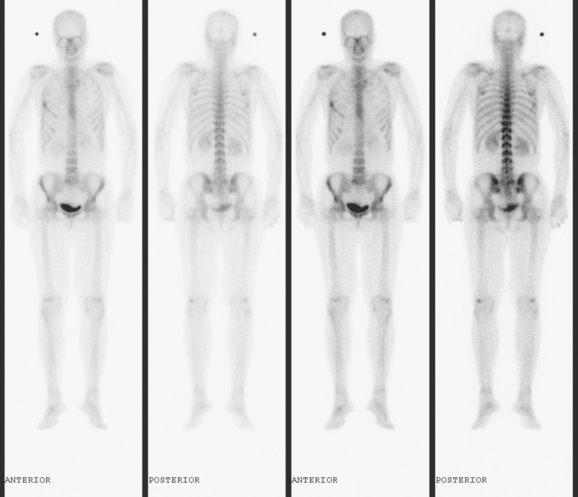
Evaluations for persistent right rib pain showed a fracture, seen on bone scan (Figures 1, 2, 3, and 4), CT (Figure 5), and PET scan. The patient had been coughing, and the activity seen on PET associated with the fracture was demonstrated subsequently to resolve on repeat PET.
PET scans obtained to monitor the patient’s response to the chemotherapy given for liver metastases show typical findings of the frequently encountered treatment phenomenon of marrow activation (Figures 6 and 7).
TEACHING POINTS
A new, solitary bone scan finding in any patient with cancer poses a diagnostic dilemma. Unlike the more conclusive bone scan pattern of multifocal metastatic activity, such a bone scan result is often equivocal and will generally require correlation with imaging studies of the area with x-ray, CT, or MRI. Biopsy may ultimately be necessary to confirm or exclude metastatic bony disease. See a similar case, Case 9 in this chapter, for a discussion of bone scan rib findings.
This case also illustrates typical PET findings of marrow activation.
Granulocyte colony-stimulating factor (G-CSF) is frequently given in conjunction with myelosuppressive chemotherapy to stimulate neutrophil precursors in bone marrow. On PET imaging, a diffuse increase in marrow activity is seen, which resolves after cessation of therapy. Generally, the increased marrow activity is diffuse and uniform. Rarely, this process may be less uniform and more difficult to differentiate from diffuse osseous metastases.
CASE 9 Significance of solitary rib activity on bone scan
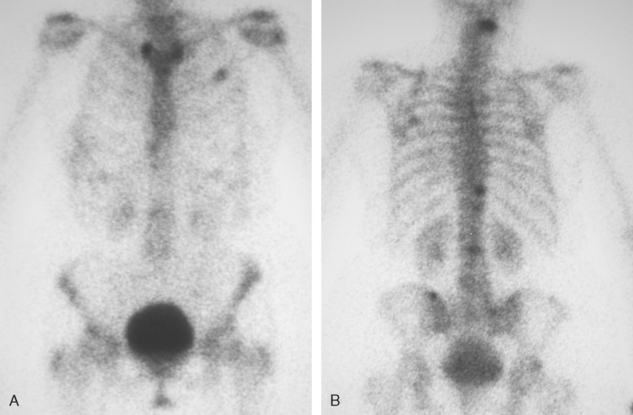
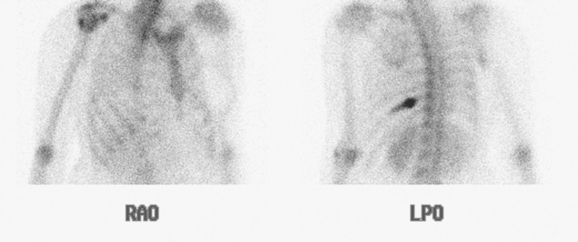
Tumor markers were negative. Bone scan showed a solitary focus of increased activity in the left eighth rib posteriorly (Figures 1 and 2). Rib x-rays suggested cortical loss of the corresponding rib. A positron emission tomography (PET)/CT scan showed a single site of modest increased metabolic activity at the same level (Figure 3). The corresponding CT identified an expansile focus at the level in question (Figure 4). This was biopsied under CT guidance, with specimens showing remodeling, with no evidence of malignancy. The patient’s pain largely resolved over the next month. Repeat bone scan (Figures 5 and 6), 2 months later (4 months after the prior bone scan) showed the left rib activity to be resolving, but there was new right rib focal activity. The patient had recently fallen, resulting in recurrent left chest wall pain and new, more severe right chest wall pain. Her tumor markers remained normal throughout.
Another bone scan obtained 4 months later showed complete resolution of the original left rib focus, consistent with fracture healing, with persistence of the newer right rib fracture activity (Figures 7 and 8).
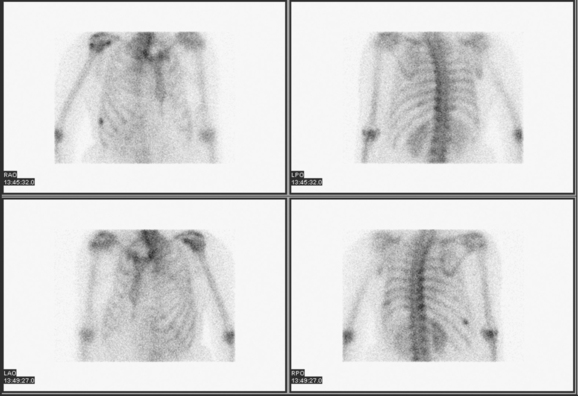
FIGURE 8 Oblique views of the thorax show persistent, very focal right lower lateral rib fracture activity.
TEACHING POINTS
Chest wall pain occurring in a breast cancer patient may herald the development of recurrent or metastatic disease. Chest wall pain could be due to metastatic involvement of a rib, with or without pathologic fracture, or could be due to development of soft tissue recurrent disease, and must be differentiated from benign disease, such as rib fracture. If the symptoms seem likely to be due to a rib fracture (there is a history of trauma or coughing), and tumor markers are negative, bone scan is probably the most cost-effective means of assessing the rib cage. More sensitive to the presence of rib abnormalities than radiographs, the bone scan also provides a whole-body context against which to assess the significance of any identified rib activity.
If bone scan does show a rib focus of activity on the anterior or posterior whole-body views, oblique and lateral views of the thorax are often helpful to better visualize the scintigraphic morphology of the activity. The pattern of activity can be helpful in differentiating malignant involvement of a rib from trauma. Of course, fractures can be pathologic, which adds to the difficulty. Views should be obtained to best visualize the pattern of activity, to determine whether the rib activity is solitary or multiple, and if multiple, whether it is scattered and randomly distributed or involving adjacent ribs. Multifocal involvement of adjacent ribs is a pattern strongly predictive of trauma as the etiology. This must be differentiated from longer segment involvement of adjacent ribs, which could signify chest wall invasion by neoplasia. If the activity is solitary, an assessment of the pattern of activity is helpful: Is the activity focal (punctate), which would favor fracture, or is there a longer segment of involvement, favoring tumor? This case illustrates that differentiation based on pattern of activity is not always possible. Fractures can have activity that is not typically focal.
CASE 10 Solitary sclerotic rib metastasis (positive on bone scan, negative on PET)
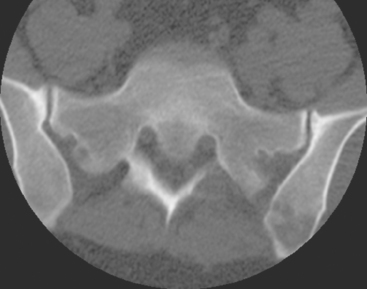
The patient was staged with enhanced body CT scans, PET/CT, and bone scan. These evaluations showed a highly suspicious left anterior fourth rib focus of increased activity on bone scan (Figure 1), with subtle corresponding sclerosis at the same level on CT (Figure 2). There was no corresponding abnormal activity on PET. CT-guided biopsy showed metastatic adenocarcinoma, consistent with breast primary.
TEACHING POINTS
Systemic screening of this patient was indicated because of her high-risk tumor status (HER-2/neu positive and eight lymph nodes involved). The combination of studies obtained in this case to systemically stage this patient (PET/CT, enhanced body CT, and bone scan) is quite comprehensive, and arguably a very cost-effective combination. Even more cost-effective would be for the CT component of the PET/CT to be contrast enhanced, thereby eliminating one of the two CT scans obtained in the evaluation illustrated in this case. There are advantages and disadvantages to this approach.
CASE 11 Assessing activity of sclerotic bone metastases
When the development of symptoms prompted reimaging, a bone scan was obtained initially and showed new activity at T9 (Figures 1, 2, and 3), corresponding to a sclerotic metastasis known from CT (Figure 4). PET scan showed no associated hypermetabolism, and the size of the lesion on CT was unchanged. Spine MRI showed signal intensity characteristics of sclerosis at this and other levels. Subtle partial enhancement was noted of the T9 lesion, correlating with the new bone scan activity (Figure 5).
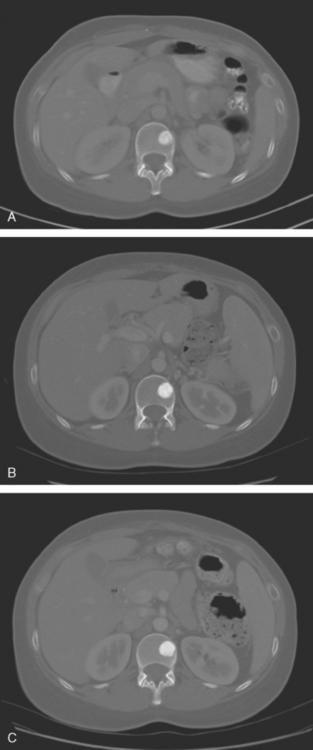
FIGURE 4 CT images for correlation (bone windows) from 3 years before (A), 1 year before (B), and concurrent with the bone scan in Figure 1 (C), show relatively stable findings of a sclerotic metastasis in the left side of the T9 vertebral body. No change in size is seen over this series of examinations. The lesion appears progressively more sclerotic, but the significance of this is uncertain.
TEACHING POINTS
Assessing the activity of sclerotic metastases is difficult. Generally, radiography and CT are not particularly helpful. Only in the rare instance of development of a new superimposed soft tissue mass or lytic components might x-ray or CT suggest clear progression or activation of a blastic metastasis. Assessing degrees of sclerosis of blastic me-tastases, either qualitatively or quantitatively, is problematic. PET and PET/CT also are frequently limited in their utility for assessment of the activity of sclerotic bone metastases, with many such lesions not associated with increased activity on PET. Development of new activity on PET associated with a sclerotic bone metastasis is helpful in suggesting disease reactivation (e.g., see Case 1 in Chapter 12). However, as this case illustrates, bone scan is very sensitive to changes in sclerotic metastases and may be the first or only modality to suggest disease reactivation. Typical imaging findings of sclerotic metastases are demonstrated by this case: focal increased activity on bone scan, increased bone density on CT, and hypointensity on all sequences on MRI. It is interesting to note the subtle enhancement seen on MRI at the level of the newly bone scan active T9 blastic metastasis. Other sclerotic bone metastases seen on the spine MRI of this patient did not show any enhancement and were scintigraphically inactive.
CASE 12 Diffuse bone metastases (superscan)
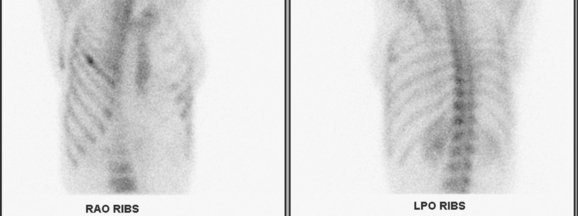
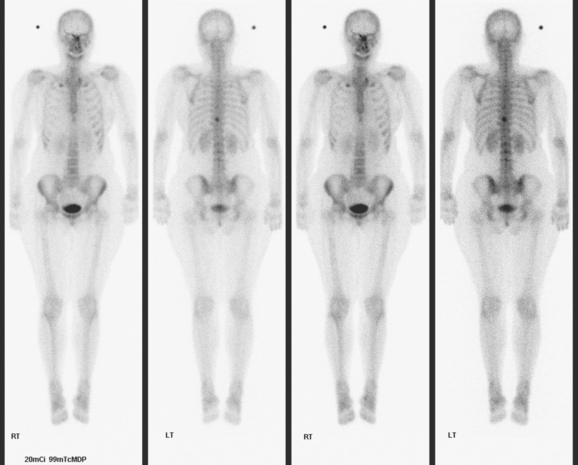
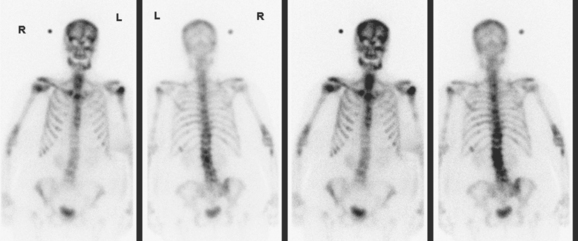
A 69-year-old woman with known extensive bony metastatic disease was evaluated with a bone scan (Figures 1, 2, and 3). Her bony metastatic disease had been diagnosed 6 years earlier, and she had undergone palliative radiation to the pelvis and hips, as well as systemic treatment with samarium. Her original diagnosis of left breast cancer was 18 years earlier. This was a T1cN1M0, left, 1.9-cm infiltrating ductal carcinoma (IDC) with 1 of 20 lymph nodes involved. She had been treated with mastectomy and with breast and regional lymphatic radiation.
TEACHING POINTS
The term superscan can be applied to bone scans with markedly increased skeletal uptake, resulting in less tracer available for renal excretion and visualization. Conditions resulting in a high bone-to–soft tissue activity ratio, with faint or little renal activity, include extensive bone metastases and metabolic bone diseases. The primary tumors most likely to produce the superscan pattern are carcinomas of the breast, lung, and prostate. Metabolic bone diseases that can produce a similar superscan pattern include renal osteodystrophy, osteomalacia, hyperparathyroidism, myelofibrosis, and systemic mastocytosis. As in this example, the diagnosis of diffuse osseous metastases is suggested by inhomogeneity of the activity, and correlation with x-rays, CT, or MRI often enables ready confirmation.
CASE 13 Radiation therapy effects on bone
A bone scan obtained 14 months after radiation therapy showed photopenia in the radiated lumbosacral spine. New metastatic foci of increased activity were noted at the inferior tip of the right scapula and at the left proximal femoral level (Figure 1). The patient did have progressive left hip aching. Radiographs did not show a corresponding abnormality, but CT bone windows showed a corresponding sclerotic focus (Figure 2).
Radiation therapy was given to the left proximal femur, with complete relief of her pain. While on radiation therapy, the patient’s regimen was changed from letrozole (Femara) to fulvestrant (Faslodex), while continuing on monthly zoledronic acid (Zometa). A repeat bone scan, 2 months after completion of hip radiation, showed resolution of the hip activity (Figure 3). Lumbar spine MRI was obtained for correlation and showed radiation therapy effects (Figure 4). Concurrent PET/CT and enhanced body CT scans, obtained to assess increased aches, rising tumor markers, and the response to Faslodex, showed new liver metastases (see Case 5 in Chapter 9 for liver imaging findings). Faslodex was discontinued and chemotherapy started with docetaxel (Taxotere) and capecitabine (Xeloda).
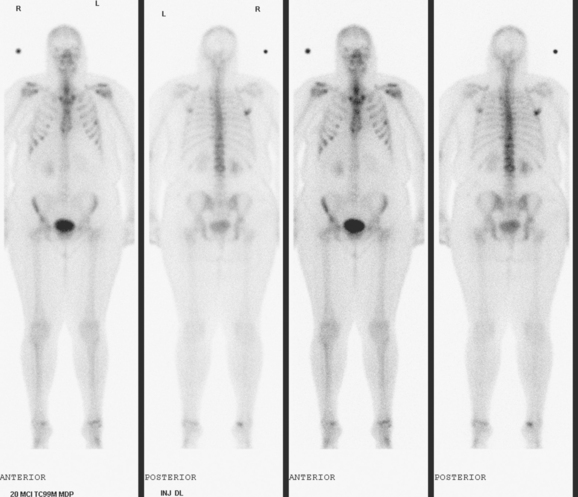
FIGURE 3 Repeat bone scan, 5 months after study in Figure 1 and 2 months after left hip radiation, shows resolution of the left proximal femoral uptake. The right inferior scapular focus is similar, but a new left anterolateral fifth rib focus of activity is seen.
TEACHING POINTS
Bone metastases are most commonly hematogenous. The vertebral venous plexus (Batson’s plexus) is thought to be an important route for hematogenous dissemination of tumor cells to the spine, the most common site of osseous metastases. Within the medullary space of bones is the lacy reticular network of trabecular bone, with marrow cells and fat within the interstices. Early bone metastases are probably to marrow through hematogenous dissemination. With growth, destruction of trabecular bone results. Eventually, a lesion of sufficient size will involve and destroy the denser cortical bone. Cortical bone is so much denser than trabecular bone that even extensive trabecular destruction without cortical involvement is generally not visualized on radiographs, CT, and bone scan. With sufficient cortical bone destruction, abnormalities may then be identified by these modalities. It has been estimated that at least 50% of cortical bone destruction must occur before a lesion can be seen on radiographs. CT is far more sensitive to cortical bone involvement than radiography, but less reliable in depicting medullary space involvement than MRI. Bone scintigraphy is 50% to 80% more sensitive than radiographs in identifying bone metastases but is not as sensitive as MRI. MRI is the most sensitive imaging modality for detection of bone metastases.
Several explanations can be considered to explain the discrepancy between MRI and bone scan in this case example. One explanation is the dominance of marrow involvement as a feature of this patient’s bone disease. The marrow involvement was essentially confluent in the spine from the initial diagnosis. Prior treatment may be another contributing factor. This patient had previously received both chemotherapy and hormonal therapy, and correlation with CT shows multiple sclerotic medullary foci in the thoracic spine, which appears uniformly active on bone scan. Confluence may be another partial explanation—the uniform appearance of the thoracic spine activity on bone scan being a manifestation of superscan-like diffuse increased activity of extensive disease. We are able to appreciate it by its contrast with the radiation-induced photopenia in the lumbar spine.
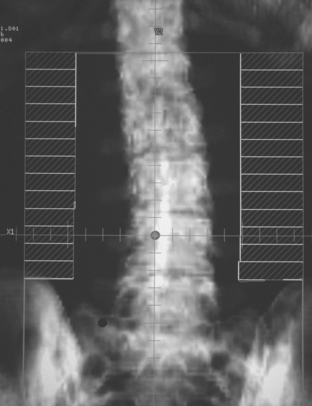
CASE 14 Extensive bone metastases; 18F bone scan
A 93-year-old woman with known breast cancer metastases to bone (Figures 1 and 2) was evaluated with positron emission tomography (PET)/CT for rising carcinoembryonic antigen (CEA) level. She had been diagnosed with left breast cancer 3 years before, and had been treated with breast conservation surgery and radiation therapy. She had been taking tamoxifen, and was now taking anastrozole (Arimidex). She had no symptoms of bone pain.
PET/CT showed diffuse bone sclerosis, with no associated fluorodeoxyglucose (FDG) avidity (Figure 3). Mildly hypermetabolic mediastinal lymph nodes were seen. 18F sodium fluoride bone scan showed intense uptake throughout the skeleton, which showed diffuse patchy sclerosis on CT (Figure 4).
TEACHING POINTS
Another possible explanation for inactivity of bone metastases on FDG PET is that the patient is being treated on an ongoing basis with Arimidex.
Even-Sapir E. Imaging of malignant bone involvement by morphologic, scintigraphic, and hybrid modalities. J Nucl Med. 2005;46(8):1356-1367.
Hall NC, Minerich SM. Focus: 18-F NaF for bone imaging. White paper
Schirrmeister H, Guhlmann A, Kotzerke J, et al. Early detection and accurate description of extent of metastatic bone disease in breast cancer with fluoride ion and positron emission tomography. J Clin Oncol. 1999;17:2381-2389.