Identifying and Avoiding Ureteral Injury
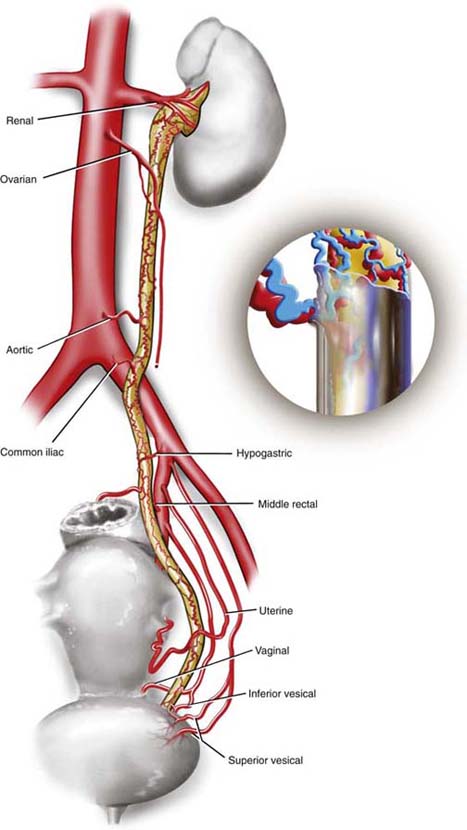
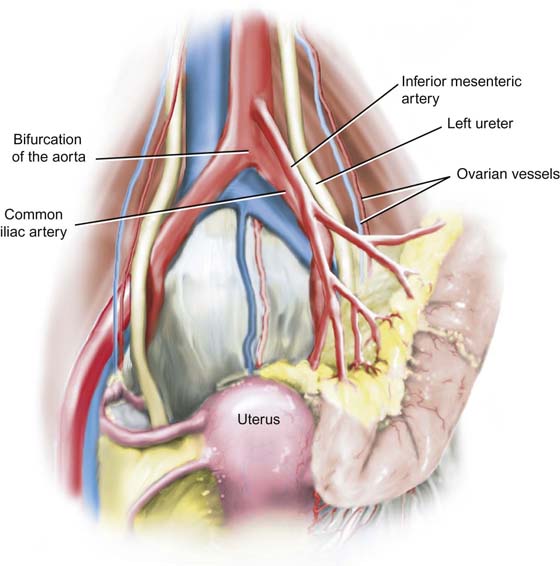
The ureter is covered by an anastomotic network of small arteries and veins. Several larger vessels feed and drain this network. Generally, above the ureteral crossover of the common iliac vessels, the arterial blood supply emanates from the medial aspect (e.g., aortic, ovarian, renal). Within the pelvis, the arterial supply to the ureter enters from the lateral direction (e.g., hypogastric, uterine, vesical, vaginal) (Fig. 37–1).
Although circulation is good, stripping the ureter of its adventitial sheath where its anastomotic network is located will result in segmental devitalization.
Ureteral length ranges between 22 and 30 cm and extends from the renal pelvis to the ureteral orifice located at either extremity of the trigonal, ureteric ridge. The lumen of the muscular ureter is approximately 3.0 to 4.0 mm in diameter (9- to 12-French).
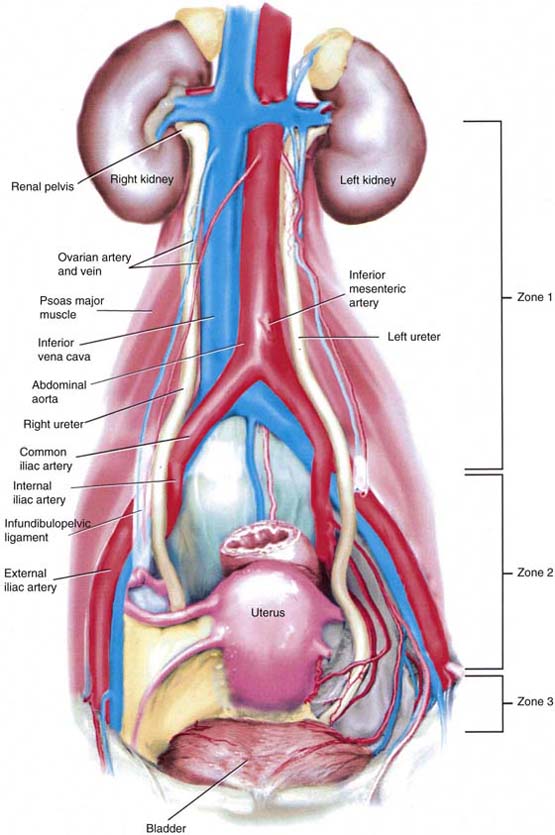
The course of the ureter may be divided into three anatomic zones (Fig. 37–2).
Zone 1: Between the renal pelvis and iliac arteries
Zone 2: Between the ureteral crossover of the iliac arteries and the point where the uterine arteries cross over the ureter
Zone 3: Between the uterine artery crossover of the ureter and the point where the ureters enter the urinary bladder
The ureter is naturally narrowed at the ureteropelvic junction, at the iliac vessel crossover, and at the ureterovesical junction. The ureter is narrowed in its intramural passage through the bladder wall. During pregnancy, hypertrophied ovarian vessels may create obstruction of the ureter above the point where they cross it. The resulting hydroureter and hydronephrosis may cause pain and urinary infection. The right ureter is more frequently and more significantly obstructed than the left.
Exposing the Ureter
Three techniques may be used to directly expose the pelvic ureter. These procedures require the surgeon to gain entry into the retroperitoneal space.
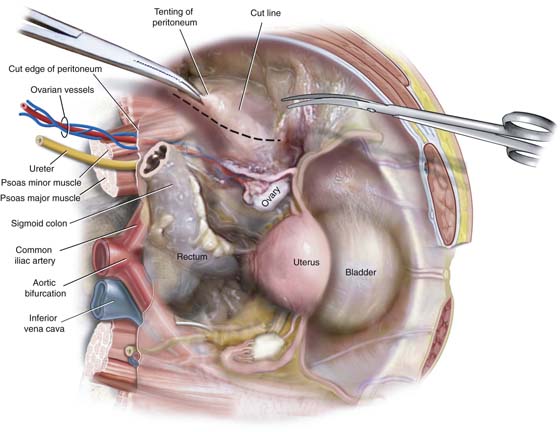
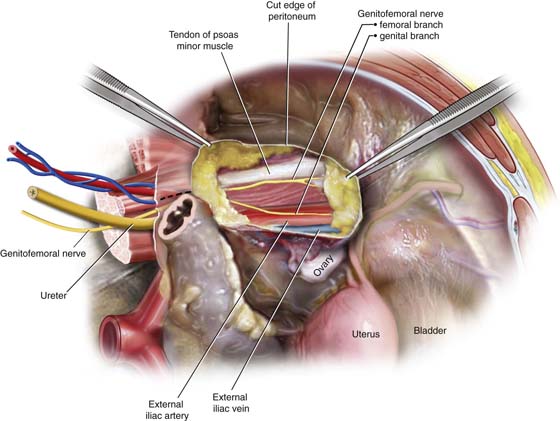
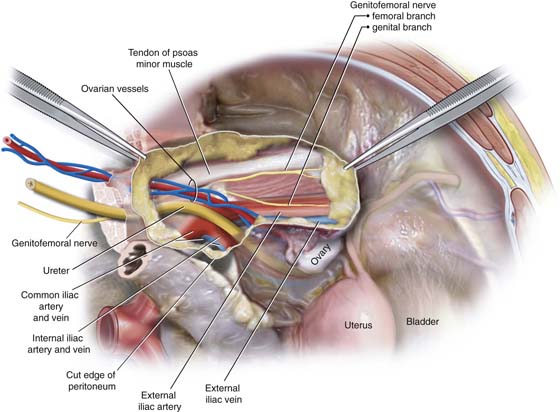
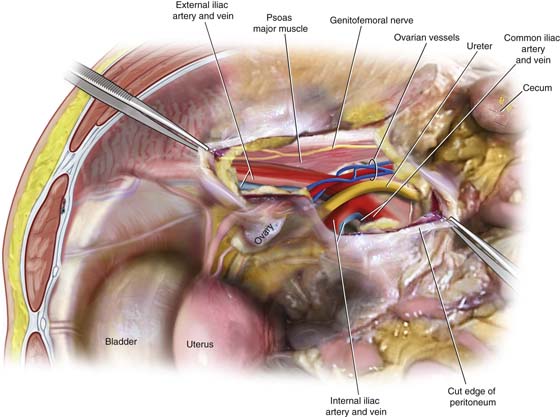
The first and most direct entry point is reached by grasping the posterior parietal peritoneum overlying the psoas major muscle (lateral to the external iliac artery) and cutting the peritoneum in a parallel direction to the external iliac artery (Fig. 37–3). The latter artery is easily palpated at the medial edge of the psoas major muscle (Fig. 37–4). The external iliac artery is dissected cranially to the iliac bifurcation, where the ureter crosses into the pelvis superficial to the common iliac vessels and medial to the hypogastric vessels (Fig. 37–5). The ureter is smaller in diameter and is lighter (white) in color than the iliac artery. The ureter does not pulsate; however, it does demonstrate peristaltic activity.
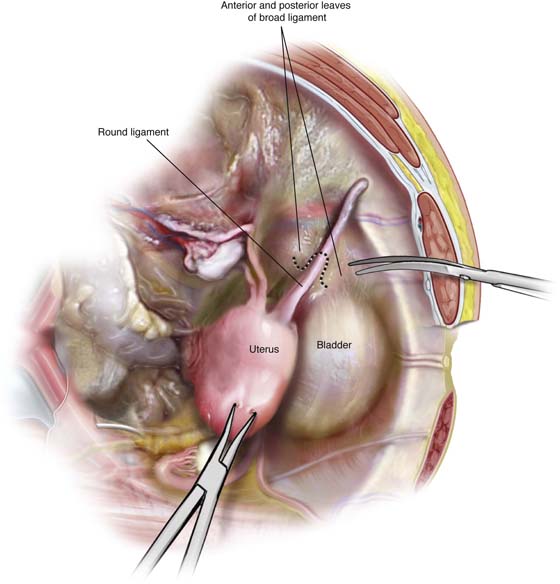
The second approach divides the round ligament so as to gain entry into the interior of the broad ligament (Fig. 37–6). The loose areolar tissue between the anterior and posterior leaves of the ligament is easily dissected with the tip of the Metzenbaum scissors or via a long tonsil clamp. As the dissection progresses deep to the floor of the broad ligament (i.e., passes the external iliac artery and vein), a white tubular structure comes into view, clinging to the medial leaf of the peritoneal edge. This is the ureter, which can be observed to undergo peristalsis (Fig. 37–7).
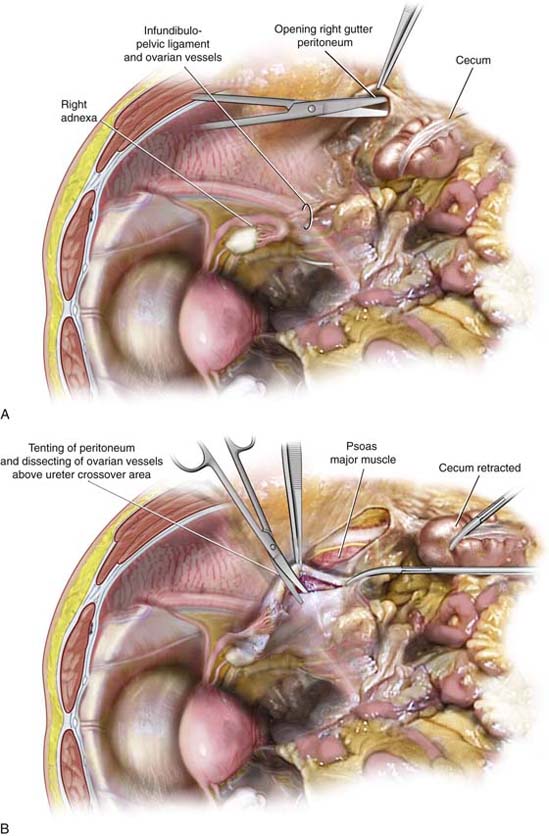
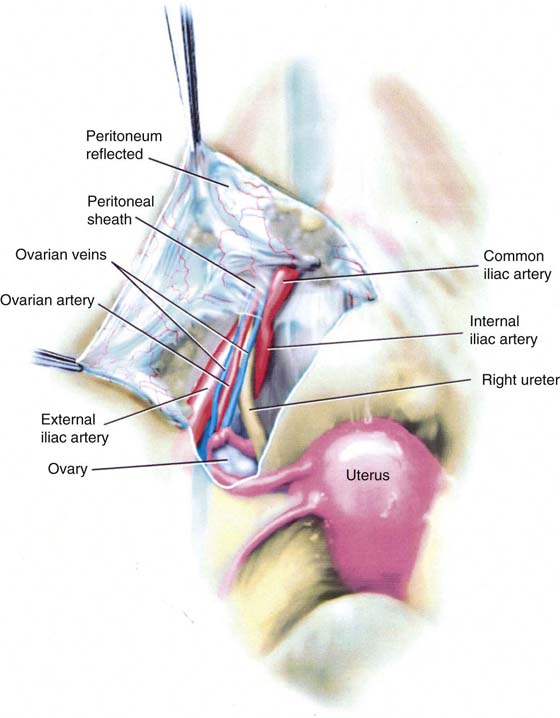
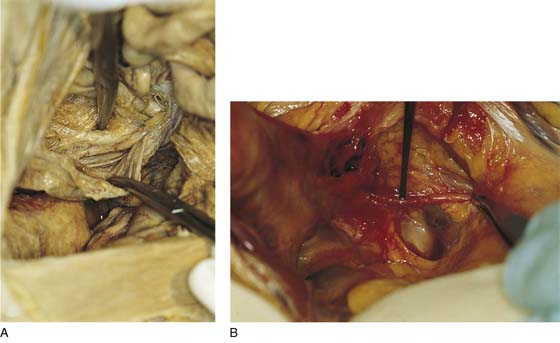
The third approach requires the surgeon to grasp the right or left adnexa and gently create traction by stretching the infundibulopelvic ligament. This is accomplished by pulling the ovary and tube anteriorly and in a slightly caudal direction.
The surgeon follows the infundibulopelvic ligament to the point where it enters the retroperitoneum (Fig. 37–8A). The peritoneum is picked up with a bayonet or other suitable toothed forceps and incised in a parallel direction to the ovarian vessels (Fig. 37–8B). The ureter lies posterior and medial to the ovarian vascular pedicle and in fact is attached to the ovarian vessels (one artery; two veins) at this location (Fig. 37–9). As in the other instances the ureter tends to be paler that the ovarian vessels and will be seen to undergo peristaltic activity.
FIGURE 37–1 The ureter has its own vascular supply, which emanates from several neighboring vessels. These vessels include renal, ovarian, aortic, iliac, rectal, uterine, and vaginal. The network of anastomotic vessels supplies the ureter from the renal pelvis to the bladder and lies in the adventitia of the ureter.
FIGURE 37–2 The three zones of ureteral anatomy. Although the shortest zone is zone 3, this is where most injuries occur. Note the anatomic differences between the right and left ureters. The left ureter is a bit more lateral in zones 1 and 2 and is lateral and to the left of the blood supply of the sigmoid colon (see Fig. 37–5).
FIGURE 37–3 The parietal peritoneum overlying the psoas major muscle is grasped with forceps and opened by cutting with Metzenbaum scissors. The cut is linear and parallel to the course of the muscle.
FIGURE 37–4 The tendon of the psoas minor muscle and the genitofemoral nerve is identified. At the medial margin of the psoas major muscle, the pulsations of the external iliac artery may be felt. The external iliac vein is immediately posterior and slightly medial to the artery.
FIGURE 37–5 Following the external iliac artery cephalad will lead the surgeon to the ureter, where it courses superficial to the common iliac vessels. Note that the ovarian vessels are anterior and slightly lateral to the ureter.
FIGURE 37–6 The round ligament is grasped with a Kelly or tonsil clamp and tented up. The ligament is divided between the two clamps (dotted line). This in fact opens the anterior and posterior leaves of the broad ligament.
FIGURE 37–7 The psoas major muscle and the external iliac vessels are identified first by palpation, then by dissection. The loose areolar tissue within the broad ligament is separated by spreading the tonsil clamp. Deep to the external iliac vessels, the surgeon can feel the hypogastric artery. Medial to it lies the ureter.
FIGURE 37–8 A. Traction is placed on the infundibulopelvic ligament, and it is followed to its retroperitoneal point of origin. B. The peritoneum is sharply opened lateral to the infundibulopelvic ligament and directly over the psoas major muscle.
FIGURE 37–9 The ureter is located just medial and slightly posterior to the ovarian vessels.
Anatomic Relationships of Right and Left Ureters
Clearly, differences should be noted between right and left ureteral anatomic relationships.
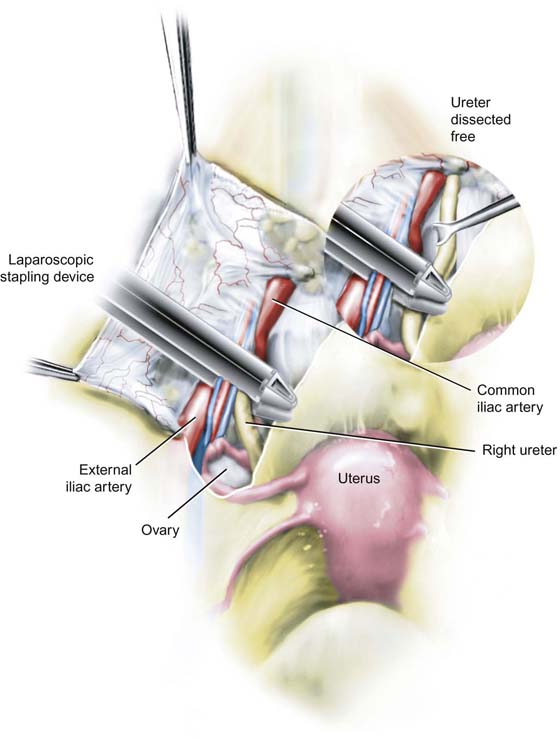
Because zone 1 is out of the pelvis, gynecologists uncommonly dissect in this area. However, the relationships will be described (see Fig. 37–2). The ureter leaves the renal pelvis and is located lateral to the ovarian artery and vein, as well as to the inferior vena cava. The ureter lies on the psoas major muscle. At approximately one third of the distance between the kidney and the iliac vessels, the ovarian vessels cross over and lie anterolateral to the ureter. As the ureter crosses the common iliac artery at its bifurcation into external and internal iliac arteries, it is posterior to the ovarian vessels but is encompassed in a common peritoneal sheath (Fig. 37–10). This is a common site for iatrogenic ureteral injury, which typically happens at the time of infundibulopelvic ligament clamping, cutting, suturing, and coagulation. Special care must be taken when a laparoscopic stapling device is applied to secure the infundibulopelvic ligaments (Fig. 37–11).
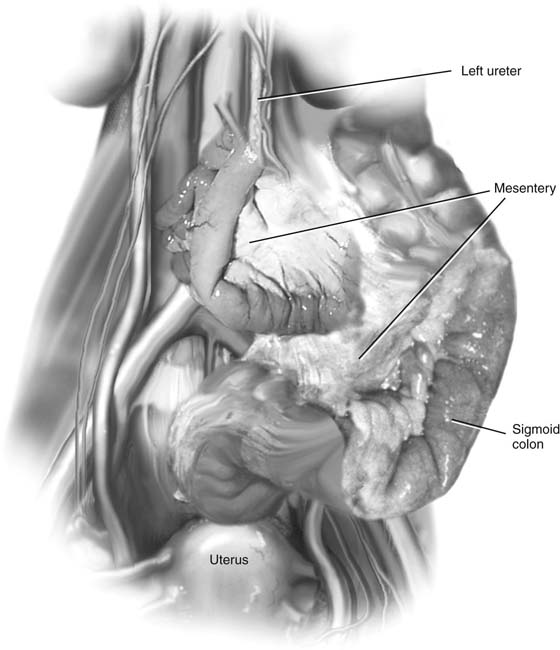
The right ureter is easier to isolate than the left because of the position of the sigmoid colon and its accompanying mesentery (Fig. 37–12). The space between the ureter and the left common iliac artery is occupied by the inferior mesenteric artery, which transverses the sigmoid mesentery to supply the large intestine (Fig. 37–13). This is a large vessel that emanates from the lower left side of the aorta just cephalad to the common iliac artery bifurcation of the aorta. Similarly, the primary branches from the inferior mesenteric artery are large vessels. These vascular channels may be confused with the ureter on the left side.
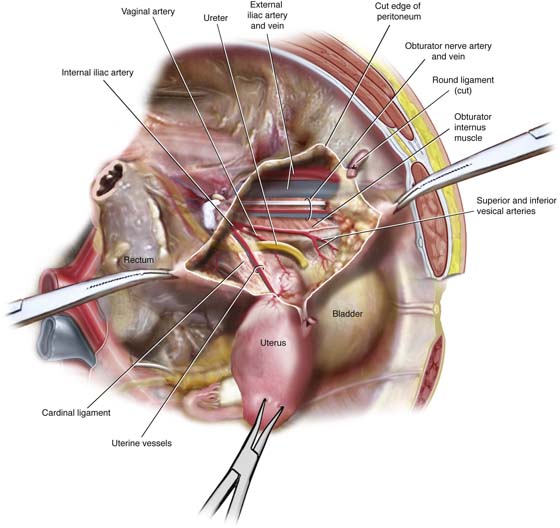
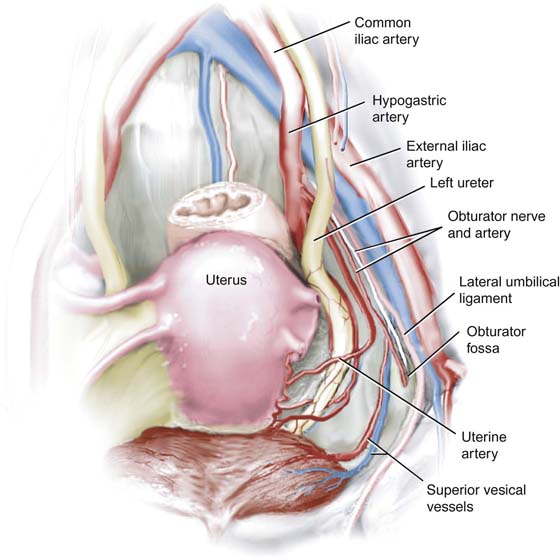
Both right and left ureters descend into the pelvis and occupy a position medial and parallel to the hypogastric arteries. The ureter is in close relationship to the obturator fossa. Again, the ureter is medial and is roughly parallel to the fossa at the level of the obturator artery and nerve. At the caudal end of the obturator fossa, the ureter sinks deeper into the pelvis and is crossed from lateral to medial obliquely by the uterine vessels. The uterine vessels continue medially to reach the lateral margin of the uterus at the cervicocorporal junction (Fig. 37–14).
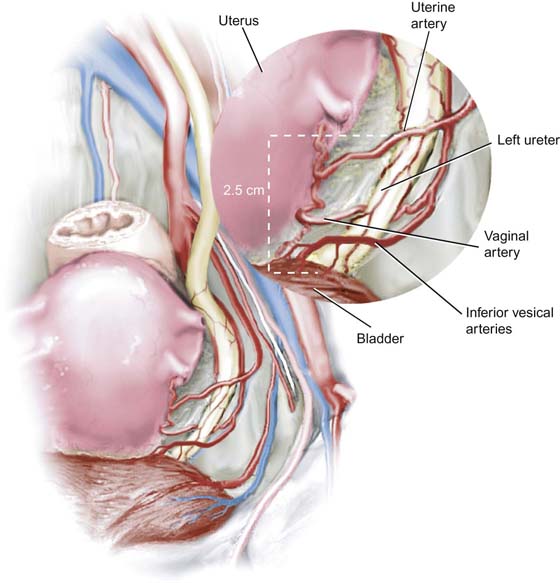
Ninety percent of ureteral injuries occur within zone 3. Not only is the 2.5-cm distance between uterine artery crossover and bladder entry a difficult area for exposure of the ureter, it is also replete with numerous and anomalous vascular channels.
The medial aspect of the ureter is sandwiched between the uterine artery (anteriorly) and the vaginal artery (posteriorly). Additionally, the ureter is crossed by the vesical arteries (Fig. 37–15).
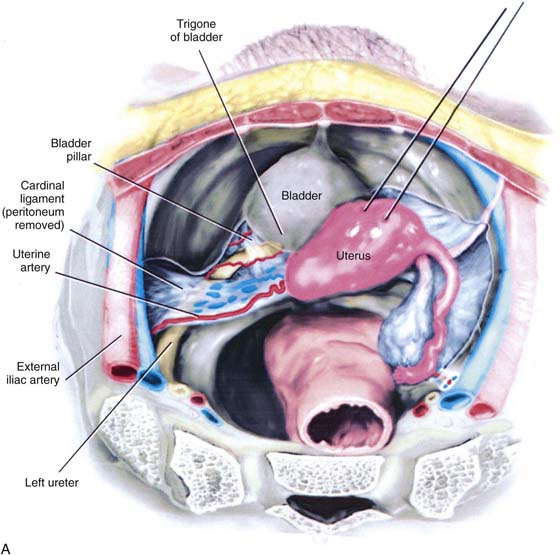
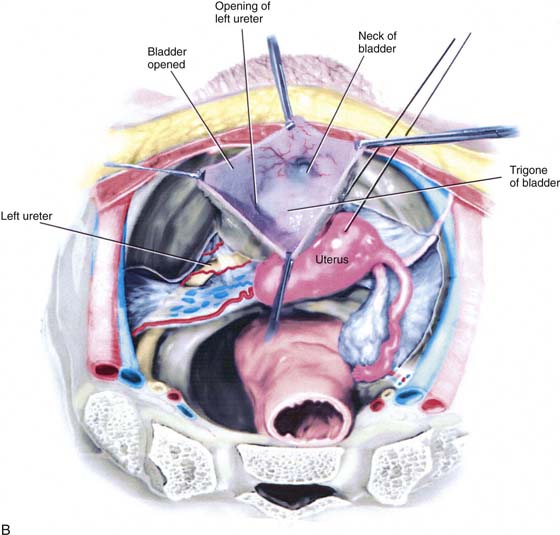
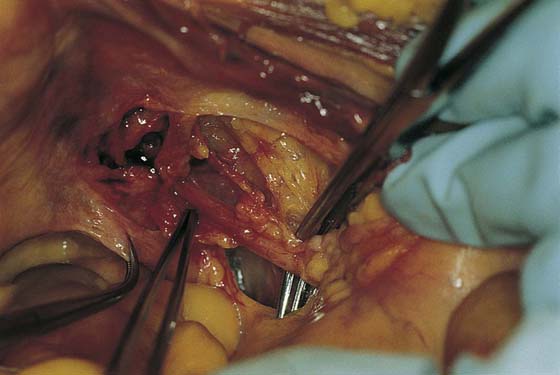
The ureter enters the upper portion of the cardinal ligament, which consists of condensed fat and fibrous tissue, honeycombed with venous sinuses. The ureter passes beneath the bladder pillar (vesicouterine ligament) to enter the base of the urinary bladder obliquely (trigone) (Fig. 37–16A, B).
FIGURE 37–10 The ureter leaves the renal pelvis and is located lateral to the ovarian artery and vein, as well as to the inferior vena cava. The ureter lies on the psoas major muscle. At approximately one third of the distance between the kidney and the iliac vessels, the ovarian vessels cross over and lie anterolateral to the ureter. As the ureter crosses the common iliac artery at its bifurcation into external and internal iliac arteries, it is posterior to the ovarian vessels but is encompassed in a common peritoneal sheath.
FIGURE 37–11 This is a common site for iatrogenic ureteral injury, which typically happens at the time of infundibulopelvic ligament clamping, cutting, suturing, and coagulation. Special care must be taken when a laparoscopic stapling device is applied to secure the infundibulopelvic ligaments.
FIGURE 37–12 The right ureter is easier to isolate than the left because of the position of the sigmoid colon and its accompanying mesentery.
FIGURE 37–13 The space between the ureter and the left common iliac artery is occupied by the inferior mesenteric artery, which traverses the sigmoid mesentery to supply the large intestine.
FIGURE 37–14 This large vessel emanates from the lower left side of the aorta just cephalad to the common iliac artery bifurcation of the aorta. Similarly, the primary branches from the inferior mesenteric artery are large vessels. These vascular channels may be confused with the ureter on the left side. Both right and left ureters descend into the pelvis and occupy a position medial and parallel to the hypogastric arteries. The ureter is in close relationship to the obturator fossa. Again, the ureter is medial and roughly parallel to the fossa at the level of the obturator artery and nerve. At the caudal end of the obturator fossa, the ureter sinks deeper into the pelvis and is crossed from lateral to medial obliquely by the uterine vessels. The uterine vessels continue medially to reach the lateral margin of the uterus at the cervicocorporal junction.
FIGURE 37–15 Ninety percent of ureteral injures occur within zone 3. Not only is the 2.5-cm distance between uterine artery crossover and bladder entry a difficult area for exposure of the ureter, it is also replete with numerous and anomalous vascular channels. The medial aspect of the ureter is sandwiched between the uterine artery (anteriorly) and the vaginal artery (posteriorly). Additionally, the ureter is crossed by the vesical arteries.
FIGURE 37–16 A and B. The ureter enters the upper portion of the cardinal ligament, which consists of condensed fat and fibrous tissue, honeycombed with venous sinuses. The ureter passes beneath the bladder pillar (vesicouterine ligament) to enter the base of the urinary bladder obliquely (trigone).
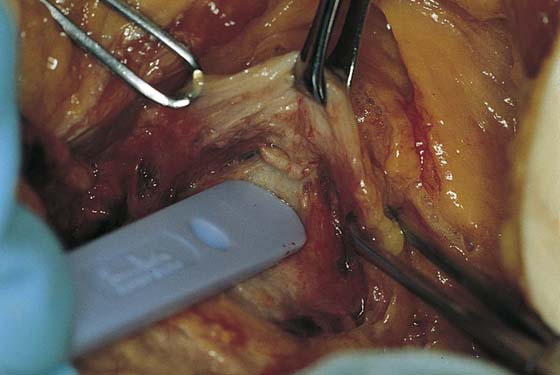
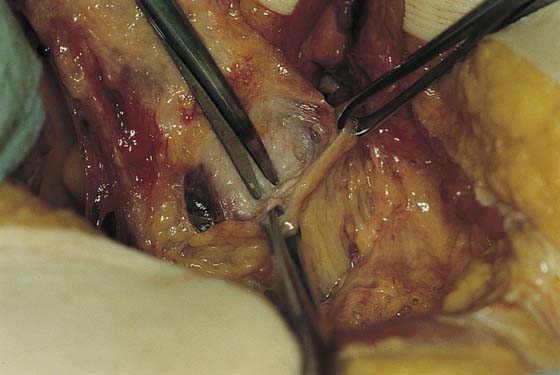
The lowest portion of the ureter as it enters the bladder can be exposed only by deeply dissecting the vesicouterine space. This is not difficult to accomplish. The pubovesicocervical fascia overlying the anterior surface of the uterine cervix is incised superficially and transversely with a sharp scalpel blade (Fig. 37–17). The space between the fascia and the substance of the outer wall of the cervix is dissected bluntly with the back of the scalpel handle to develop the initial plane (Fig. 37–18). Next, with a long scissors or the operator’s index finger, the dissection proceeds inferiorly to develop a wide space between the bladder and the vagina (Fig. 37–19). As with the rectouterine space, this can be extended all the way down to the level of the vaginal introitus (Fig. 37–20).
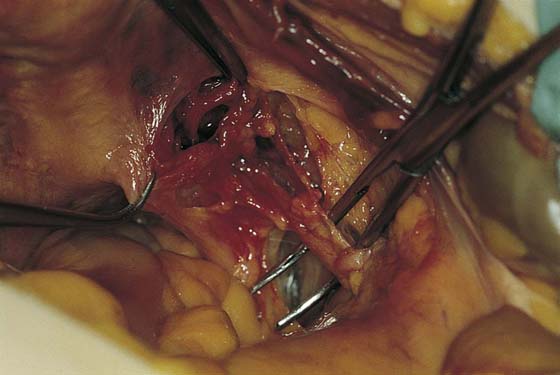
After the operator enters the retroperitoneal space (see Chapter 36), the most convenient point at which the ureter can be identified is where it crosses lateral to and medial above the common iliac artery. By careful dissection with a long tonsil clamp and with the use of an untied hammock of umbilical tape to provide counteraction, the ureter can be clearly viewed to the point of uterine artery crossover (Fig. 37–21A, B).
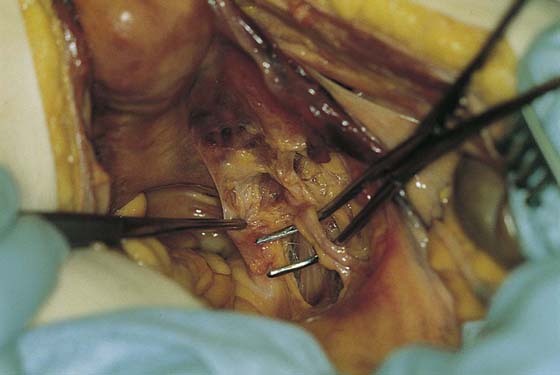
Any procedure performed on or around the uterosacral ligaments must take into account the position of the ureter relative to the operative site. In other words, the location must be precisely known (Fig. 37–22). Palpation of what the operator believes to be the ureter is not accurate. The ureter is relatively closer to the ligament posteriorly and laterally (Fig. 37–23).
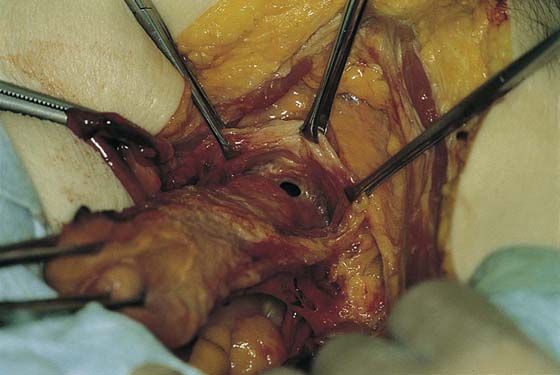
At the level of the cardinal ligament, the ureter passes obliquely toward the bladder base and is closely applied to the lateral angle of the vagina (Fig. 37–24). Dissection of the ureter through the cardinal ligament is difficult because the ligament is honeycombed with thin-walled vessels. The ureter can be unroofed by clamping above and excising that portion of the cardinal ligament.
FIGURE 37–17 The lowest portion of the ureter as it enters the bladder can be exposed only by deeply dissecting the vesicouterine space. This is not difficult to accomplish. The pubovesicocervical fascia overlying the anterior surface of the uterine cervix is incised superficially and transversely with a sharp scalpel blade.
FIGURE 37–18 The space between the fascia and the substance of the outer wall of the cervix is dissected bluntly with the back of the scalpel handle to develop the initial plane.
FIGURE 37–19 Next, with the use of long scissors or the operator’s index finger, the dissection proceeds inferiorly to develop a wide space between the bladder and the vagina.
FIGURE 37–20 As with the rectouterine space, this can be extended all the way down to the level of the vaginal introitus.
FIGURE 37–21 A and B. After the operator enters the retroperitoneal space (see Chapter 36), the most convenient point at which the ureter can be identified is where it crosses lateral to medial above the common iliac artery. By careful dissection with a long tonsil clamp and with the use of an untied hammock of umbilical tape to provide counteraction, the ureter can be clearly viewed to the point of uterine artery crossover.
FIGURE 37–22 Any procedure performed on or around the uterosacral ligaments must take into account the position of the ureter relative to the operative site. In other words, the location must be precisely known.
FIGURE 37–23 Palpation of what the operator believes to be the ureter is not accurate. The ureter is relatively closer to the ligament posteriorly and laterally.
FIGURE 37–24 At the level of the cardinal ligament, the ureter passes obliquely toward the bladder base and is closely applied to the lateral angle of the vagina.