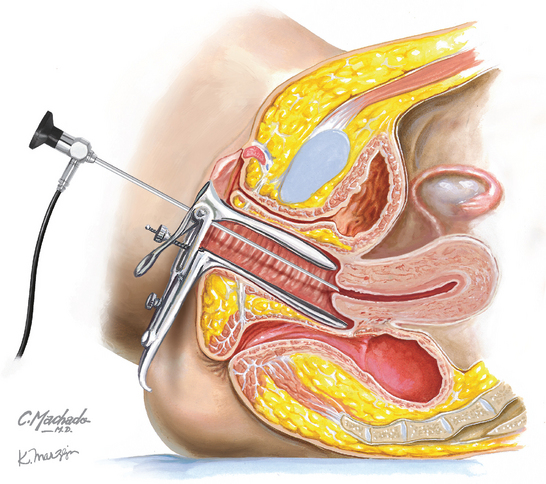
Chapter 245 Hysteroscopy
REQUIRED EQUIPMENT
CPT CODE(S)
Bain C, Parkin DE, Cooper KG. Is outpatient diagnostic hysteroscopy more useful than endometrial biopsy alone for the investigation of abnormal uterine bleeding in unselected premenopausal women? A randomised comparison. BJOG. 2002;109:805.
Barik S. Topical anaesthesia for diagnostic hysteroscopy and endometrial biopsy for postmenopausal women: a randomised placebo-controlled double-blind study. Br J Obstet Gynaecol. 1997;104:1326.
Cicinelli E, Didonna T, Ambrosi G, et al. Topical anaesthesia for diagnostic hysteroscopy and endometrial biopsy in postmenopausal women: a randomised placebo-controlled double-blind study. Br J Obstet Gynaecol. 1997;104:316.
Kremer C, Duffy S, Moroney M. Patient satisfaction with outpatient hysteroscopy versus day case hysteroscopy: randomized controlled trial. BMJ. 2000;320:279.
Lau WC, Lo WK, Tam WH, Yuen PM. Paracervical anaesthesia in outpatient hysteroscopy: A randomised double-blind placebo-controlled trial. Br J Obstet Gynaecol. 1999;106:356.
Nagele F, Lockwood G, Magos AL. Randomised placebo controlled trial of mefenamic acid for premedication at outpatient hysteroscopy: a pilot study. Br J Obstet Gynaecol. 1997;104:842.
Sagiv R, Sadan O, Boaz M, et al. A new approach to office hysteroscopy compared with traditional hysteroscopy: a randomized controlled trial. Obstet Gynecol. 2006;108:387.
Soriano D, Ajaj S, Chuong T, et al. Lidocaine spray and outpatient hysteroscopy: randomized placebo-controlled trial. Obstet Gynecol. 2000;96:661.
Clark TJ, Voit D, Gupta JK, et al. Accuracy of hysteroscopy in the diagnosis of endometrial cancer and hyperplasia: a systematic quantitative review. JAMA. 2002;288:1610.
Sharma M, Taylor A, di Spiezio Sardo A, et al. Outpatient hysteroscopy: traditional versus the “no-touch” technique. BJOG. 2005;112:963.
van Dongen H, de Kroon CD, Jacobi CE, et al. Diagnostic hysteroscopy in abnormal uterine bleeding: a systematic review and meta-analysis. BJOG. 2007;114:664.
American College of Obstetricians and Gynecologists. Management of anovulatory bleeding. ACOG Practice Bulletin 14. Washington, DC: ACOG, 2000.
Apgar BS, DeWitt D. Diagnostic hysteroscopy. Am Fam Physician. 1992;46:19S. 29S, 35S.
Gambone JC, Munro MG. Office sonography and office hysteroscopy. Curr Opin Obstet Gynecol. 1993;5:733.
Gimpelson RJ. Office hysteroscopy. Clin Obstet Gynecol. 1992;35:270.
Katz VL. Diagnostic procedures. In: Katz VL, Lentz GM, Lobo RA, Gershenson DM, editors. Comprehensive Gynecology. 5th ed. Philadelphia: Mosby/Elsevier; 2007:230.
Lewis BV. Hysteroscopy for the investigation of abnormal uterine bleeding. Br J Obstet Gynaecol. 1990;97:283.
March CM. Hysteroscopy. J Reprod Med. 1992;37:293.
Siegler AM. Office hysteroscopy. Obstet Gynecol Clin North Am. 1995;22:457.
Siegler AM, Kemmann E. Hysteroscopy. Obstet Gynecol Surv. 1975;30:567.
Siegler AM, Valle RF. Therapeutic hysteroscopic procedures. Fertil Steril. 1988;50:685.