Hypothyroidism
Clinical features
Causes
Over 90% of cases of hypothyroidism occur as a consequence of:
Diagnosis
Clinical features other than those of hypothyroidism may indicate the need for investigation of pituitary function (see pp. 84–85), and the TRH test will be included in such a protocol.
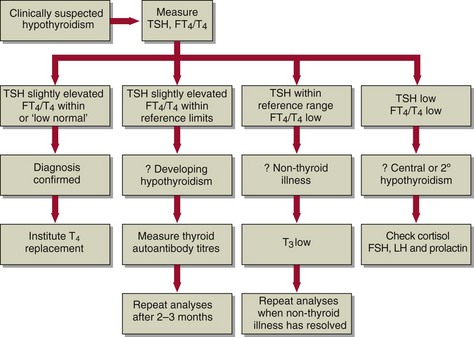
A strategy for the biochemical investigation of clinically suspected hypothyroidism is shown in Figure 45.1.
Treatment
Replacement therapy with T4 is the treatment of choice since the hormone is readily available in a pure stable form, and is inexpensive. Monitoring TSH concentrations can be helpful in assessing the adequacy of treatment. Once the dosage is established, the patient will be required to continue treatment for life (Fig 45.2).
Figure 45.3 shows the need for careful monitoring of treatment. This graph shows the changes in thyroid hormone results as a hyperthyroid woman patient became hypothyroid after radioiodine treatment, and it subsequently proved difficult to stabilize her on a replacement dose of thyroxine.
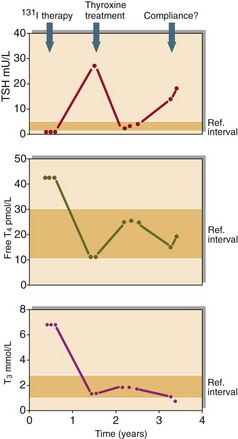
Fig 45.3 Biochemical monitoring of a patient during treatment for thyroid disease. This 55-year-old woman was first diagnosed as hyperthyroid, and received radioiodine therapy. She became profoundly hypothyroid, and was treated with thyroxine. Her thyroid hormone results at first indicated good replacement, but recently they indicate that she is under-replaced. It is possible that she is not taking her thyroxine tablets regularly.
Screening for neonatal hypothyroidism
Congenital hypothyroid disorders occur with a frequency of one in every 4000 live births (pp. 156–157). If they are diagnosed at an early age, replacement thyroid hormone can be given and normal development can occur. Delays in treatment result in cretinism (see p. 156). Elevated TSH, measured in blood spots, is diagnostic of disorders of the thyroid itself, i.e. primary neonatal hypothyroidism. The TSH screening test does not pick up pituitary dysfunction in the newborn.