Hyperuricaemia
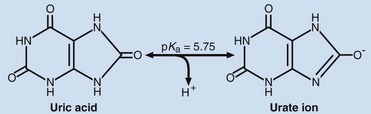
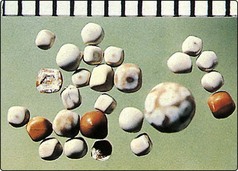
Nucleic acids contain bases of two different types, pyrimidines and purines. The catabolism of the purines, adenine and guanine, produces uric acid. At physiological hydrogen ion concentration, uric acid is mostly ionized and present in plasma as sodium urate (Fig 72.1). An elevated serum urate concentration is known as hyperuricaemia. Uric acid and sodium urate are relatively insoluble molecules that readily precipitate out of aqueous solutions such as urine or synovial fluid (Fig 72.2). The consequence of this is the medical condition gout.
Urate formation and excretion
Urate is formed in three ways. These are:
Urate is excreted in two ways:
 Via the kidney. The majority of urate is excreted via the kidney. Renal handling of urate is complex. It is freely filtered at the glomerulus, but 99% is reabsorbed in the proximal tubule. The distal tubules also secrete urate, but again much is reabsorbed. The amount of urate excreted in the urine is around 10% of that filtered at the glomerulus.
Via the kidney. The majority of urate is excreted via the kidney. Renal handling of urate is complex. It is freely filtered at the glomerulus, but 99% is reabsorbed in the proximal tubule. The distal tubules also secrete urate, but again much is reabsorbed. The amount of urate excreted in the urine is around 10% of that filtered at the glomerulus.
 Via the gut. Smaller amounts of urate are excreted into the gut where it is broken down by bacteria. This process is called uricolysis.
Via the gut. Smaller amounts of urate are excreted into the gut where it is broken down by bacteria. This process is called uricolysis.
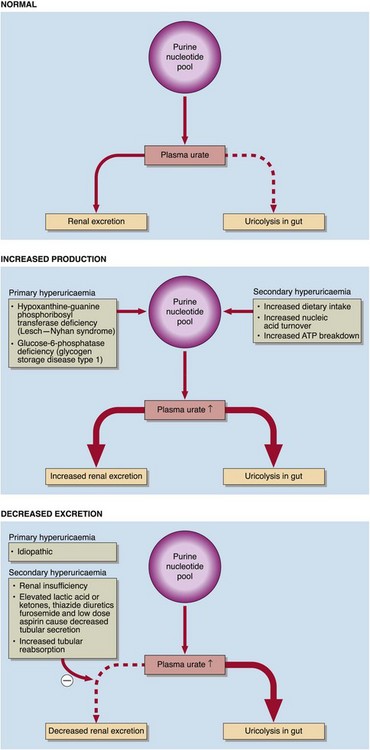
Urate concentrations in serum are higher in men than women. Even within the reference interval, serum urate is near its aqueous solubility limit. The presence of protein helps to keep the molecule in solution. A high serum urate may arise from increased urate formation, or from decreased excretion. The common causes of hyperuricaemia are summarized in Figure 72.3. Genetic causes of hyperuricaemia are known as primary disorders, and there are also secondary causes. Most primary causes are due to decreased excretion of urate (90% of cases) rather than increased production (10%).
Gout
Acute gout is triggered by the tissue deposition of sodium urate crystals that cause an intense inflammatory response. In the chronic situation, tophaceous deposits of sodium urate may form in the tissues (Fig 72.4). Gout is exacerbated by alcohol. The reason for this is twofold. Ethanol increases the turnover of ATP and urate production. Ethanol in excess may cause the accumulation of organic acids that compete with the tubular secretion of uric acid. Disorders such as ethanol intoxication, diabetic ketoacidosis and starvation lead to elevations of lactic acid, β-hydroxybutyric acid and acetoacetic acid, and will cause hyperuricaemia.
Renal disease and hyperuricaemia
Renal disease is a common complication of hyperuricaemia. Several types of renal disease have been identified. The most common is urate nephropathy, which is caused by the deposition of urate crystals in renal tissue or the urinary tract to form urate stones. This may be associated with chronic hyperuricaemia. Acute renal failure can be caused by the rapid precipitation of uric acid crystals that commonly occurs during treatment of patients with leukaemias and lymphomas. In the ‘acute tumour lysis syndrome’ (p. 139), nucleic acids are released as a result of tumour cell breakdown, are rapidly metabolized to uric acid and this sometimes results in very high concentrations, precipitating gout or nephropathy. In these cases, urate oxidase is sometimes administered prophylactically to metabolize the uric acid to allantoin, which is safely excreted by the kidney.