Hyperthyroidism
Clinical features
The clinical features of hyperthyroidism may be dramatic and include:
Causes
Hyperthyroidism can result from:
 Graves’ disease (diffuse toxic goitre)
Graves’ disease (diffuse toxic goitre)
 exogenously administered iodine and iodine-containing drugs, e.g. amiodarone
exogenously administered iodine and iodine-containing drugs, e.g. amiodarone
Although the eyelid retraction commonly seen in the patient with Graves’ disease (Fig 46.3) is due to the effects of high thyroid hormone concentration, not all of the eye signs are caused this way. Rather, the thyroid and orbital muscle may have a common antigen that is recognized by the circulating autoantibodies. The inflammatory process in the eye may lead to severe exophthalmos. This may even occur in the euthyroid patient.
Diagnosis
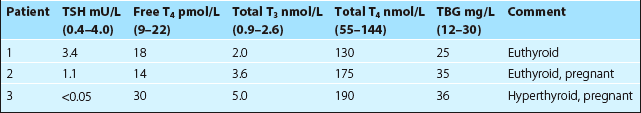
Occasionally, biochemical confirmation of suspected hyperthyroidism will prove more difficult. The total T4 concentration in a serum sample does not always reflect metabolic status, because of changes in binding protein concentration. In pregnancy, high circulating oestrogens cause stimulation of thyroid binding globulin (TBG) synthesis in the liver. Total T4 concentrations will be above the reference interval although free T4 will be normal (Fig 46.1). Congenital TBG deficiency can also cause confusion if a specimen is screened for thyroid hormones, even if thyroid disease is not suspected (Fig 46.1). TBG deficiency is encountered much less frequently than increased TBG.
Free T4 assays are routinely used as first-line tests of thyroid dysfunction. TSH secretion is very sensitive to changes in free T4, and many laboratories use TSH on its own to screen for thyroid disease. Free T4 analyses are invaluable in diagnoses where binding proteins are altered, e.g. in pregnancy, in women on the oral contraceptive pill and in patients with the nephrotic syndrome (Table 46.1).
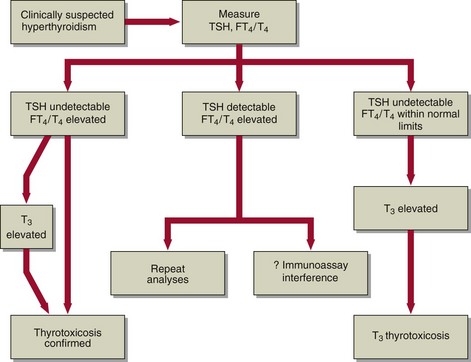
A strategy for the biochemical investigation of clinically suspected hyperthyroidism is shown in Figure 46.2.
Treatment
There are three methods for the treatment of Graves’ disease:
 Antithyroid drugs (such as carbimazole and propylthiouracil). These are of most use in the younger patient.
Antithyroid drugs (such as carbimazole and propylthiouracil). These are of most use in the younger patient.
 Radioiodine. Therapy with sodium 131I is commonly used in older patients. Most will eventually require replacement thyroxine. Thus ‘thyroid function tests’ should be checked regularly to detect developing hypothyroidism.
Radioiodine. Therapy with sodium 131I is commonly used in older patients. Most will eventually require replacement thyroxine. Thus ‘thyroid function tests’ should be checked regularly to detect developing hypothyroidism.
 Surgery. Many patients who have subtotal thyroidectomy may later require thyroxine replacement. Occasionally the parathyroids may be damaged and the patient may become hypocalcaemic post-operatively due to lack of PTH.
Surgery. Many patients who have subtotal thyroidectomy may later require thyroxine replacement. Occasionally the parathyroids may be damaged and the patient may become hypocalcaemic post-operatively due to lack of PTH.
Thyroid eye disease
Clinically, thyroid eye disease can be a prominent feature of Graves’ disease (Fig 46.3). It may pursue a separate or similar course to the thyroid disease; typically it takes longer to resolve. It may be exacerbated by the administration of radioiodine, and steroid treatment may be required.