Hypertension
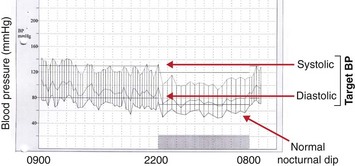
Hypertension is a common clinical problem. It is defined as chronically increased systemic arterial blood pressure. The definition of hypertension has changed over the years, as more effective treatments have become available. The WHO classification of hypertension is shown in Table 68.1. It is important not to base clinical decisions on a single blood pressure reading. Some patients have ‘white coat’ hypertension, where readings taken by doctors or other health professionals are misleadingly high. Ambulatory blood pressure measurement over a whole day provides the most detailed information (Fig 68.1).
Table 68.1
WHO classification of hypertension
| Category | BP (mmHg) |
| Optimal blood pressure | <120/80 |
| Normal blood pressure | <130/85 |
| Mild hypertension | 140/90–159/99 |
| Moderate hypertension | 160/100–179/109 |
| Severe hypertension | ≥180/110 |
If hypertension is left untreated, patients are at risk of several complications. These include:
Causes of hypertension
 Renal parenchymal disease. This is strongly suggested by the finding of a reduced estimated glomerular filtration rate (eGFR) and/or proteinuria.
Renal parenchymal disease. This is strongly suggested by the finding of a reduced estimated glomerular filtration rate (eGFR) and/or proteinuria.
 Renal artery stenosis. This should be suspected in refractory hypertension, especially if creatinine rises on treatment with angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs). This is best diagnosed with magnetic resonance angiography. It may be associated with grossly elevated renin concentrations.
Renal artery stenosis. This should be suspected in refractory hypertension, especially if creatinine rises on treatment with angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs). This is best diagnosed with magnetic resonance angiography. It may be associated with grossly elevated renin concentrations.
 Primary hyperaldosteronism. This is dealt with in more detail on page 99. It should be suspected if hypokalaemia (often with associated alkalosis) is present, especially if there is a failure to respond to potassium supplementation. The ratio of aldosterone to renin is characteristically elevated, although imaging studies (CT or MRI) are required to make the diagnosis.
Primary hyperaldosteronism. This is dealt with in more detail on page 99. It should be suspected if hypokalaemia (often with associated alkalosis) is present, especially if there is a failure to respond to potassium supplementation. The ratio of aldosterone to renin is characteristically elevated, although imaging studies (CT or MRI) are required to make the diagnosis.
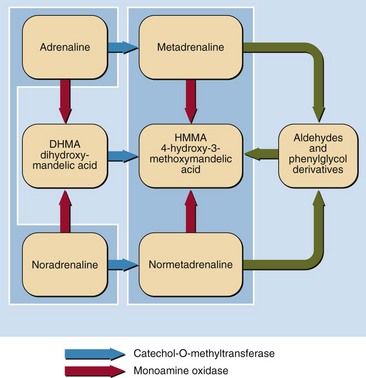
 Phaeochromocytoma. This is a relatively rare cause of secondary hypertension. It should be suspected if hypertension is paroxysmal, or if symptoms (like palpitations, headaches) are episodic. Urinary catecholamines are usually but not always raised, and there are often false positive results as well. Urine or, especially, plasma metadrenalines (catecholamine metabolites) are more sensitive and specific for diagnosis. Isotope (MIBG) scans are very specific and help to localize the tumour. The biochemical pathways involved in the production of catecholamines are illustrated in Figure 68.2.
Phaeochromocytoma. This is a relatively rare cause of secondary hypertension. It should be suspected if hypertension is paroxysmal, or if symptoms (like palpitations, headaches) are episodic. Urinary catecholamines are usually but not always raised, and there are often false positive results as well. Urine or, especially, plasma metadrenalines (catecholamine metabolites) are more sensitive and specific for diagnosis. Isotope (MIBG) scans are very specific and help to localize the tumour. The biochemical pathways involved in the production of catecholamines are illustrated in Figure 68.2.
 Cushing’s syndrome. This is dealt with in more detail on pages 98–99. It is not usually a diagnostic dilemma, since the signs and symptoms of Cushing’s syndrome, and the association with hypertension, are well recognized. However, if there is doubt, a dexamethasone suppression test (p. 83) may be useful.
Cushing’s syndrome. This is dealt with in more detail on pages 98–99. It is not usually a diagnostic dilemma, since the signs and symptoms of Cushing’s syndrome, and the association with hypertension, are well recognized. However, if there is doubt, a dexamethasone suppression test (p. 83) may be useful.
 Obesity/sleep apnoea. Obesity is an increasingly common cause of secondary hypertension, especially if it is associated with sleep apnoea. The latter is likely in the presence of an increased neck circumference.
Obesity/sleep apnoea. Obesity is an increasingly common cause of secondary hypertension, especially if it is associated with sleep apnoea. The latter is likely in the presence of an increased neck circumference.
 Other. Less common causes of secondary hypertension include acromegaly, hyperthyroidism and hypothyroidism, and coarctation of the aorta.
Other. Less common causes of secondary hypertension include acromegaly, hyperthyroidism and hypothyroidism, and coarctation of the aorta.
Treatment of hypertension
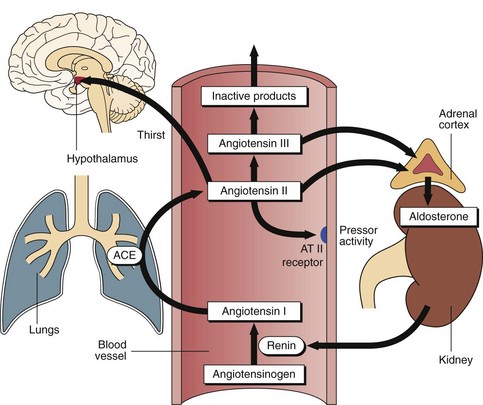
 ACEIs/ARBs. ACEIs inhibit angiotensin-converting enzyme, and so reduce production of angiotensin II (a potent vasoconstrictor) and, ultimately, aldosterone (a potent mineralocorticoid). ARBs block angiotensin receptors (Fig 68.3). Both groups of drugs may in some patients reduce the renal damage induced by hypertension; this can be monitored by their effect on reducing proteinuria. In some patients with refractory hypertension, the introduction of ACEI/ARBs is associated with a rapid rise in creatinine. In this scenario, the drug should be stopped and renal artery stenosis suspected (see above; Fig 68.4).
ACEIs/ARBs. ACEIs inhibit angiotensin-converting enzyme, and so reduce production of angiotensin II (a potent vasoconstrictor) and, ultimately, aldosterone (a potent mineralocorticoid). ARBs block angiotensin receptors (Fig 68.3). Both groups of drugs may in some patients reduce the renal damage induced by hypertension; this can be monitored by their effect on reducing proteinuria. In some patients with refractory hypertension, the introduction of ACEI/ARBs is associated with a rapid rise in creatinine. In this scenario, the drug should be stopped and renal artery stenosis suspected (see above; Fig 68.4).
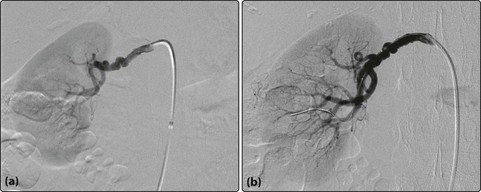
Fig 68.4 Renal artery stenosis: (a) pre-angioplasty and (b) post-angioplasty. Note the substantial increase in blood flow into the kidney post procedure. The functional impact of renal artery stenosis can be assessed clinically by the response to antihypertensive treatment, and biochemically by measurement of plasma renin activity.
 Beta blockers. Although these drugs now compete with more effective alternatives, they are still widely used. They act by blocking beta-adrenergic receptors in the heart, kidneys and brain, thereby reducing cardiac output, renin and noradrenaline release.
Beta blockers. Although these drugs now compete with more effective alternatives, they are still widely used. They act by blocking beta-adrenergic receptors in the heart, kidneys and brain, thereby reducing cardiac output, renin and noradrenaline release.
 Calcium channel blockers. These drugs are also widely used. They reduce entry of calcium into vascular smooth muscle, thereby reducing vascular tone and peripheral arterial resistance.
Calcium channel blockers. These drugs are also widely used. They reduce entry of calcium into vascular smooth muscle, thereby reducing vascular tone and peripheral arterial resistance.
 Diuretics. These all induce natriuresis. Thiazide diuretics like bendroflumethiazide enhance the efficacy of other drugs, and are commonly used, especially in the elderly; they may cause clinically significant hyponatraemia. Furosemide also induces a natriuresis, but there is no significant hyponatraemia. The hypovolaemia it causes induces secondary hyperaldosteronism and absorption of the sodium in the distal tubule, in exchange for potassium, and a risk of hypokalaemia. Spironolactone and other aldosterone antagonists (also known as potassium-sparing diuretics) are often associated with hyperkalaemia; potassium should be checked before and after their introduction.
Diuretics. These all induce natriuresis. Thiazide diuretics like bendroflumethiazide enhance the efficacy of other drugs, and are commonly used, especially in the elderly; they may cause clinically significant hyponatraemia. Furosemide also induces a natriuresis, but there is no significant hyponatraemia. The hypovolaemia it causes induces secondary hyperaldosteronism and absorption of the sodium in the distal tubule, in exchange for potassium, and a risk of hypokalaemia. Spironolactone and other aldosterone antagonists (also known as potassium-sparing diuretics) are often associated with hyperkalaemia; potassium should be checked before and after their introduction.
 Other drugs. Doxazosin (an alpha blocker) and moxonidine (centrally acting) are also used. Other drugs are reserved for specialist care.
Other drugs. Doxazosin (an alpha blocker) and moxonidine (centrally acting) are also used. Other drugs are reserved for specialist care.