Adenomyomatosis: Mural GB wall thickening due to formation of intramural diverticula (Rokitansky-Aschoff sinuses) with smooth muscle and epithelial proliferation
IMAGING
• Adenomyomatosis
 US: Focal, segmental, or diffuse wall thickening with anechoic intramural spaces, intramural echogenic foci ± acoustic shadowing, “comet tail” artifacts, & twinkle artifact
US: Focal, segmental, or diffuse wall thickening with anechoic intramural spaces, intramural echogenic foci ± acoustic shadowing, “comet tail” artifacts, & twinkle artifact
 US: Focal, segmental, or diffuse wall thickening with anechoic intramural spaces, intramural echogenic foci ± acoustic shadowing, “comet tail” artifacts, & twinkle artifact
US: Focal, segmental, or diffuse wall thickening with anechoic intramural spaces, intramural echogenic foci ± acoustic shadowing, “comet tail” artifacts, & twinkle artifact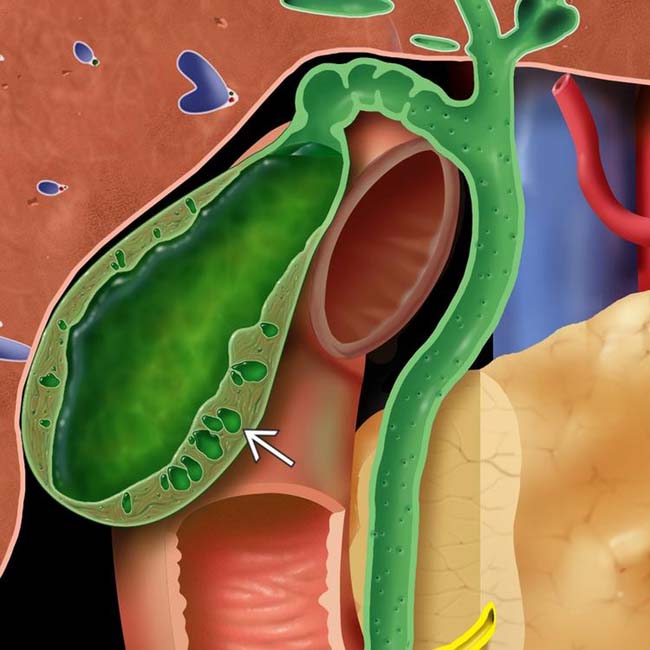
 .
.
 within the anterior wall of the GB and posterior “comet tail” artifacts
within the anterior wall of the GB and posterior “comet tail” artifacts  . This appearance is likely caused by reverberation of the ultrasound pulse within cholesterol crystals in the GB subepithelium.
. This appearance is likely caused by reverberation of the ultrasound pulse within cholesterol crystals in the GB subepithelium.
 , classic for adenomyomatosis. Note the presence of a gallstone
, classic for adenomyomatosis. Note the presence of a gallstone  , found in 90% of cases.
, found in 90% of cases.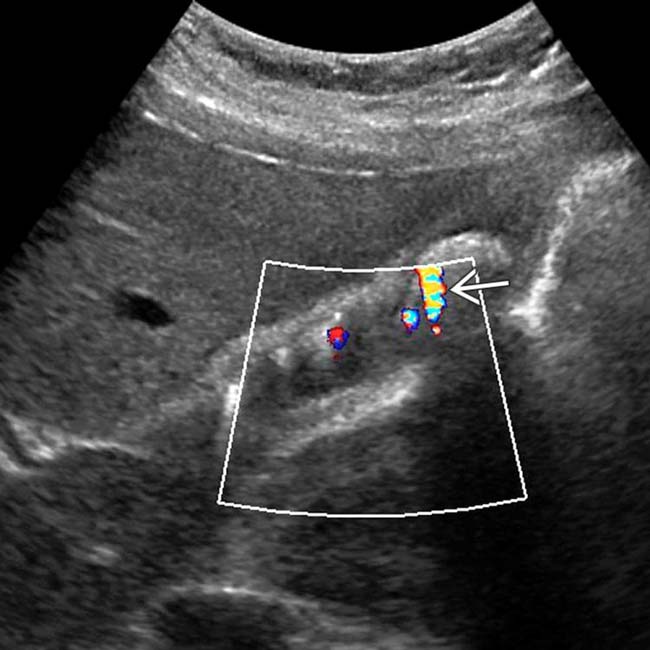
 associated with the echogenic reflectors within the thickened GB wall. “Comet tail” and twinkle artifacts are due to reverberation within cholesterol deposited within epithelial penetrations (Rokitansky-Aschoff sinuses).
associated with the echogenic reflectors within the thickened GB wall. “Comet tail” and twinkle artifacts are due to reverberation within cholesterol deposited within epithelial penetrations (Rokitansky-Aschoff sinuses).IMAGING
General Features
MR Findings
Ultrasonographic Findings
• Grayscale ultrasound
 Adenomyomatosis
Adenomyomatosis
 Adenomyomatosis
Adenomyomatosis
– Focal, segmental, or diffuse wall thickening
DIFFERENTIAL DIAGNOSIS
Chronic Cholecystitis
PATHOLOGY
General Features
• Etiology
CLINICAL ISSUES
Presentation
Treatment
• Cholesterol polyps: Although benign, nonspecific appearance often prompts intervention; may be resected when large or when growth documented
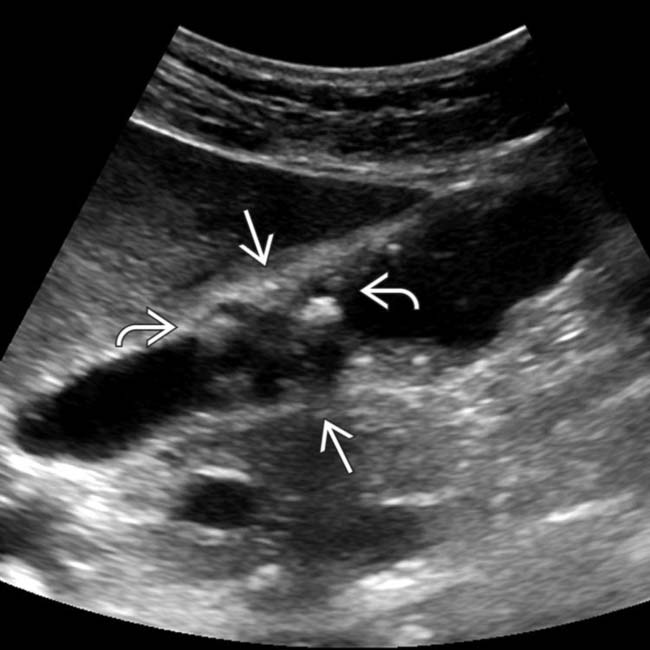
 of the mid body of the GB. Note the presence of intramural diverticula and echogenic foci
of the mid body of the GB. Note the presence of intramural diverticula and echogenic foci  in this pathologically confirmed example of segmental adenomyomatosis.
in this pathologically confirmed example of segmental adenomyomatosis.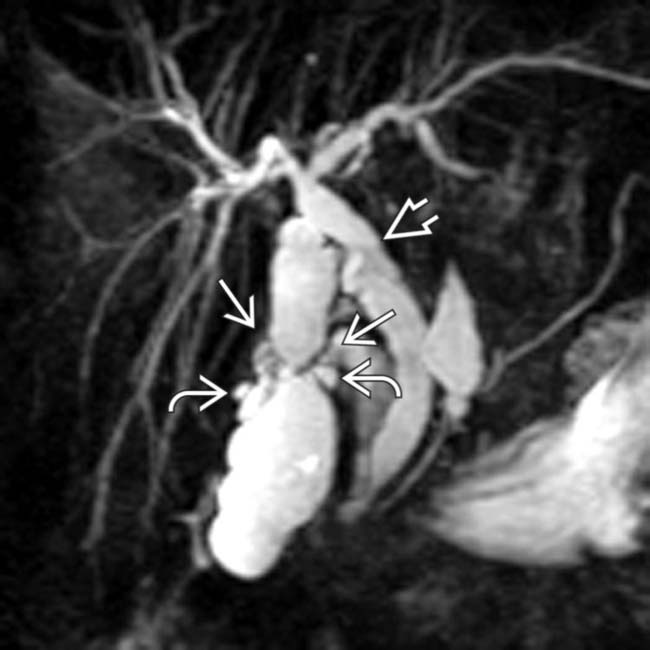
 of the GB and several adjacent intramural diverticula
of the GB and several adjacent intramural diverticula  . Common bile duct dilatation
. Common bile duct dilatation  and clinical suspicion of intermittent choledocholithiasis prompted cholecystectomy.
and clinical suspicion of intermittent choledocholithiasis prompted cholecystectomy.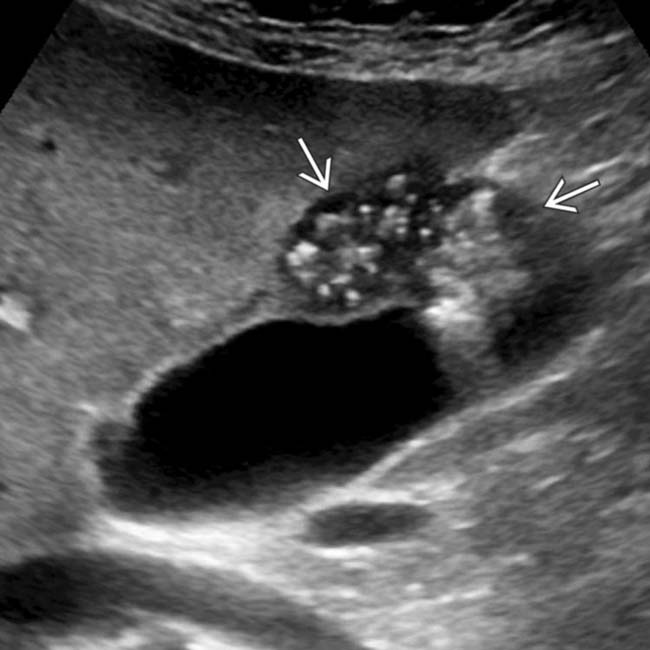
 . Echogenic foci within the lesion are associated with “comet tail” artifact, characteristic of adenomyomatosis.
. Echogenic foci within the lesion are associated with “comet tail” artifact, characteristic of adenomyomatosis.
 and several minute, echogenic GB polyps
and several minute, echogenic GB polyps  . Pathology showed cholesterolosis and hyperplastic (cholesterol) polyps.
. Pathology showed cholesterolosis and hyperplastic (cholesterol) polyps.
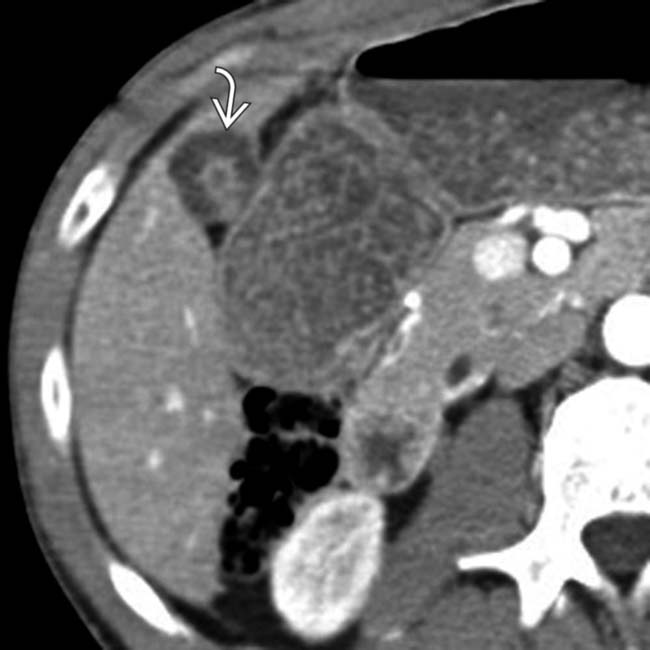
 within a thickened portion of the GB fundus.
within a thickened portion of the GB fundus.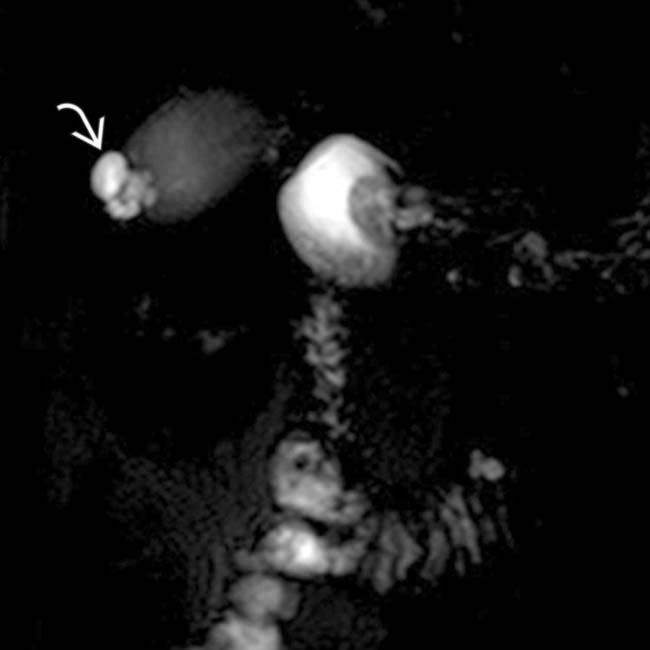
 in the GB fundus corresponding to the findings on CT. Both the CT and MR appearance is classic for adenomyomatosis, a benign finding that does not require follow-up or treatment.
in the GB fundus corresponding to the findings on CT. Both the CT and MR appearance is classic for adenomyomatosis, a benign finding that does not require follow-up or treatment.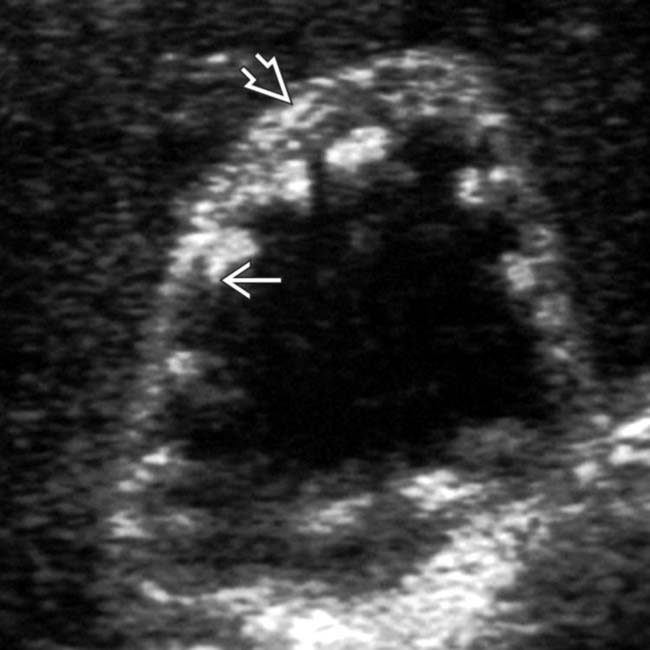
 and multiple echogenic foci with “comet tail” reverberation artifacts
and multiple echogenic foci with “comet tail” reverberation artifacts  .
.
 with multiple tiny cystic spaces, characteristic of adenomyomatosis.
with multiple tiny cystic spaces, characteristic of adenomyomatosis.
 , the so-called pearl necklace sign, characteristic of adenomyomatosis.
, the so-called pearl necklace sign, characteristic of adenomyomatosis.
 at the GB fundus, a classic appearance for focal fundal adenomyomatosis.
at the GB fundus, a classic appearance for focal fundal adenomyomatosis.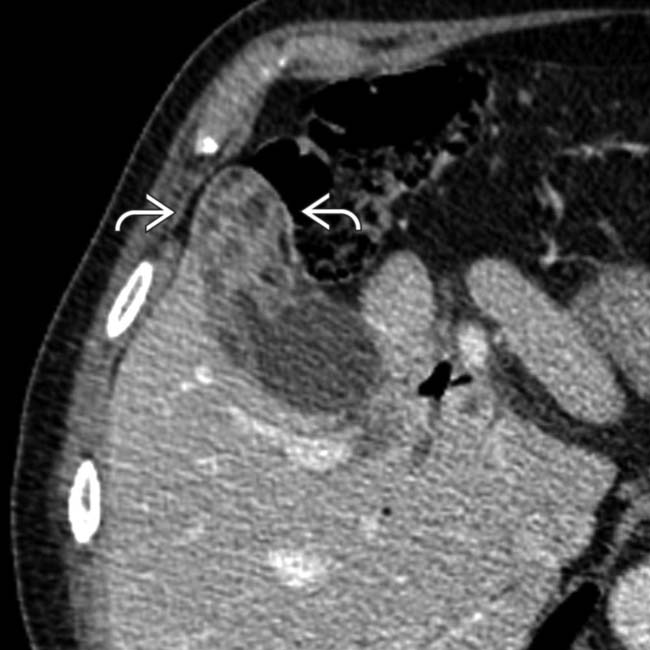
 . The cystic regions within the mass are thought to represent dilated Rokitansky-Aschoff sinuses.
. The cystic regions within the mass are thought to represent dilated Rokitansky-Aschoff sinuses.
 . Although the features are characteristic of adenomyomatosis, a cholecystectomy was performed due to suggestion of hepatic invasion at CT
. Although the features are characteristic of adenomyomatosis, a cholecystectomy was performed due to suggestion of hepatic invasion at CT  .
.
 , consistent with fundal adenomyomatosis.
, consistent with fundal adenomyomatosis.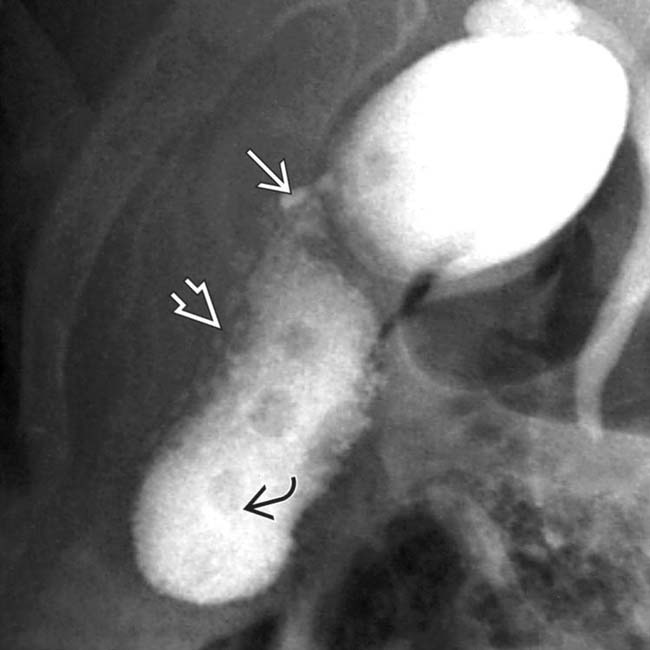
 , multiple intramural diverticula
, multiple intramural diverticula  , and gallstones
, and gallstones  .
.

























































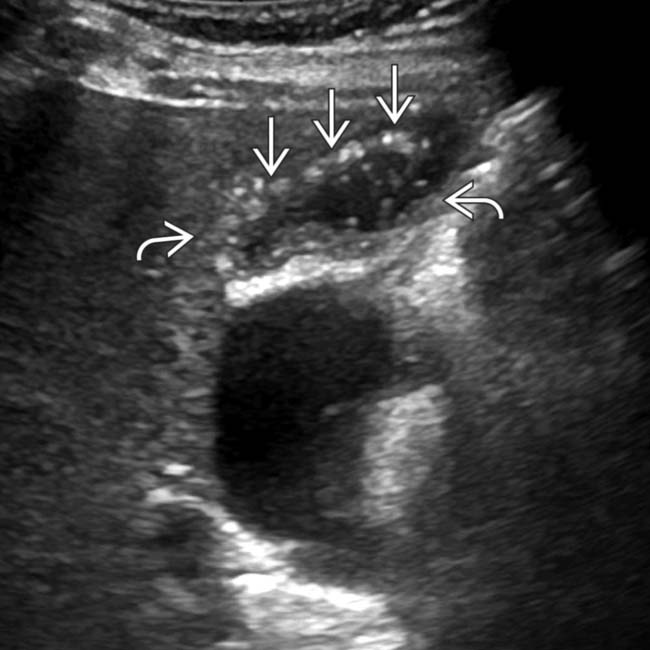
 and subtle “comet tail” artifacts within a cystic-appearing GB fundal mass
and subtle “comet tail” artifacts within a cystic-appearing GB fundal mass  . Fundal adenomyomatosis may be mistaken at ultrasound for adjacent duodenum.
. Fundal adenomyomatosis may be mistaken at ultrasound for adjacent duodenum.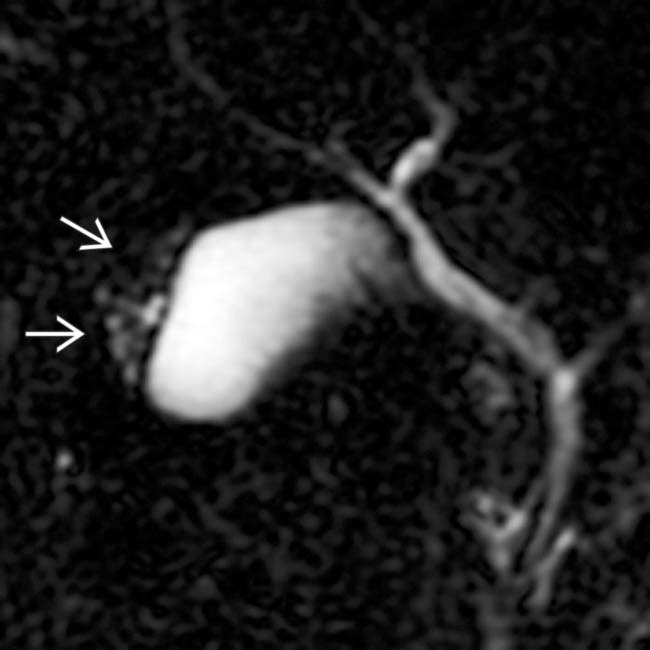
 within dilated Rokitansky-Aschoff sinuses. This MR “string of pearls” sign is characteristic of fundal adenomyomatosis.
within dilated Rokitansky-Aschoff sinuses. This MR “string of pearls” sign is characteristic of fundal adenomyomatosis.

