Chapter 18 Hyperlipidemia
With contribution from Professor Manohar Garg
Introduction
Hyperlipidemia is a heterogeneous disorder characterised by increased circulating levels of plasma cholesterol, low-density lipoprotein (LDL)-cholesterol, triglycerides and apolipoprotein-B (apoB) as well as reduced high-density lipoprotein (HDL)-cholesterol concentration.1 The primary lipid abnormality involved in the development of hyperlipidemia is an increase in circulating free (non-esterified) fatty acids originating from adipose tissue, caused by a down-regulation of signalling pathways, as well as inadequate esterification and metabolism.2 Reduced retention of fatty acids by adipose tissue results in an increased flux of non-esterified or free fatty acids (FFA) returning to the liver, stimulating hepatic triglyceride synthesis, promoting production of apoB and assembly/secretion of very low-density lipoprotein (VLDL).3 Presence of increased plasma triglyceride concentration results in the increased production of triglyceride rich HDL particles that are more likely to be catabolized resulting in reduced HDL-cholesterol. Elevated VLDL particles are lipolyses, converted into small dense (highly atherogenic) LDL particles with reduced receptor-mediated clearance, prolonged retention in circulation and an increased susceptibility to peroxidation.4 A strong independent association between elevated levels of LDL-cholesterol and increased incidence of coronary heart disease (CHD) has been established.5, 6
Prevalence and economy of burden
The World Health Organization (WHO) estimated that hyperlipidemia is associated with more than 50% of global cases of ischemic heart disease and >4 million deaths/year.7 Most (80%) lipid disorders are related to diet and lifestyle, although familial disorders (20%) are important as well. The basic categories of hyperlipidemia include: increased LDL-cholesterol, reduced HDL-cholesterol, excess lipoprotein(a) (LPa), hypertriglyceridemia, atherogenic dyslipidemia, and mixed lipid disorders.8 Most patients with CHD have mixed hyperlipidemia (e.g. elevated LDL-cholesterol and low HDL-cholesterol), which is also commonly seen in patients with diabetes mellitus.
The American Heart Association estimates that more than 98 million Americans have total cholesterol levels >5.18mmol/L (200mg/dL), which is considered a moderately high level, and more than 34 million adult Americans have levels >6.2mmol/L (240mg/dL), which is considered a high level necessitating treatment.9 A recent Australian study set out to estimate the prevalence of selected diagnosed chronic diseases among patients (n = 9156) attending general practice reported prevalence of hyperlipidemia to be 15.9%.10 Prevalence of dyslipidemia in a professional population in Beijing, China has been reported to be 52.7% for males and 42.9% for females with at least 1 abnormality in the blood lipid profile.11
Increasing evidence supports triglyceride (TG) concentration as a risk factor for cardiovascular disease,12 however, the exact role of hypertriglyceridemia in the development of CVD is not known. A recent study examined the prevalence of hyperlipidemia in 5610 adults aged 20 years or older enrolled in the National Health and Nutrition Examination Surveys (NHANES) from 1999 to 2004.13 Unadjusted prevalence rates (percentages) of TG concentration of 1.695mmol/L (150mg/dL) or higher occurred in 33.1% of participants, a concentration of 2.26mmol/L (200mg/dL) or higher occurred in 17.9% of participants, a concentration of 5.65mmol/L (500mg/dL) or higher occurred in 1.7% of participants, and a concentration of 11.3mmol/L (1000mg/dL) or higher occurred in 0.4% of participants.
The total cost associated with cardiovascular diseases and stroke in the United States, many of which are related to dyslipidemia, was estimated to exceed $400 billion in 2006.14 Total costs include medical services (direct costs) as well as lost wages (indirect costs). While the health care system is only associated with the direct costs, these are nearly two-thirds of total costs. Costs of cardiovascular disease and stroke vary widely around the world, but in every instance, costs are substantial.15 Closely related to dyslipidemia is diabetes mellitus. Persons with diabetes mellitus have average LDL-cholesterol levels in excess of 140mg/dL, and most require drug therapy.16
The National Heart Foundation (NHF) of Australia recommends lifestyle advice supplemented by pharmacological measures for the appropriate management of hyperlipidemia.17 Management should be based on both the individual’s measured serum cholesterol levels and estimated absolute cardiovascular risk. The management aims to lower the plasma lipid levels as part of the absolute risk profile of the individual, which is particularly relevant in high-risk groups such as diabetics, people with familial hypercholesterolemia, vascular disease, chronic kidney disease and those with a family history of coronary heart disease.17
Table 18.1 summarises the NHF recommendation of lifestyle factors for reducing cholesterol levels and risk of developing cardiovascular disease.
| Dietary advice |
|---|
Table 18.2 summarises the NHF recommendations for drug and nutrient therapy in patients with hyperlipidemia.
Table 18.2 NHF recommendations of drug/nutrient therapy17
| Statins (HMG-CoA Reductase Inhibitors) | Reduces the level of LDL-C; modest triglyceride-lowering; HDL-C-raising effects |
| Fibrates | |
| Fish oils | |
| Bile acid binding resins in selected patients |
The NHF goals and targets for therapy, especially in people with existing coronary heart disease or other high-risk groups, are summarised as:17
Lipid management recommendations, if adopted, have immense potential for significant health gain; however conventional lipid-modifying treatments such as statins and fibrates are underused, due to both under-prescription and non-adherence to treatment in Australia and overseas.18, 19 The Adult Treatment Panel III (ATP III) guidelines of the US National Cholesterol Education Program (NCEP) emphasise the importance on lowering cholesterol but also place greater emphasis on lowering triglyceride levels.20 Therefore statin monotherapy may not be sufficient to achieve the recommended non-LDL goals, especially given their modest effects on triglyceride concentration.
Pharmacological therapies including bile acid sequestrant resins, statins, fibrates, niacin and cholesterol absorption inhibitors are common treatment options for hyperlipidemia, however the use of alternative therapies is also becoming increasingly popular. Controlled trials using a range of dietary supplements, herbal extracts and functional foods (e.g. policosanols, flaxseed, red yeast rice, guggulipid, garlic, viscous fibre, tree nuts and soy proteins) have been examined as potential complementary treatments in the management of hyperlipidemia.21 A recent survey found that as many as 50% of respondents with elevated cholesterol levels would prefer non-prescription drugs such as garlic, yeast, or soy products as an alternative to pharmaceutical drugs.22
Risk factors for hyperlipidemia
Risk factors for hyperlipidemia include:
Familial hypercholesterolemia
Familial hypercholesterolemia (FH) is caused by a defect on the short arm of chromosome 19 via an autosomal dominant gene.23 FH is a result of mutations that influence the binding of LDL particles to the cell-surface receptor (LDL-receptor). Five classes of mutations in the LDL-receptor have been identified with each class having multiple alleles.24 Class 1 mutations are null mutations as these result in a complete failure to express any LDL-receptor protein. Most common are the class 2 mutations resulting in intracellular transport defects so that the LDL-receptor does not move between the intracellular membranes (endoplasmic reticulum and the golgi membranes). Class 3 mutations involve LDL-receptors that are expressed and transported to the cell surface but fail to bind with LDL particles. Class 4 mutations are the rarest that result in failure of the LDL-receptor/LDL particle complexes be internalised. Class 5 mutations cause failure of the LDL-receptor recycling back to the cell surface. Regardless of the class of mutation, the body’s ability to remove LDL-cholesterol from the bloodstream is impaired and that results in raised blood levels of LDL-cholesterol, contributing to increased risk of atherosclerosis, cardiovascular and coronary heart disease.
Pharmaceutical treatment of hyperlipidemia: key factors to consider
Compliance
Despite all of the positive research and trial data about statins and other pharmacologic interventions for treating elevated cholesterol, many patients do not take these drugs. Drug companies have reported that over 30% of patients initiated on statins do not continue their prescriptions. These reasons warrant a review of the efficacy of dietary and non-pharmacologic measures to lower cholesterol compared with pharmacologic therapy.25
Efficacy of treatment
Several treatment or preventive strategies may significantly reduce lipid levels; however, the reduction may not be large enough to be of clinical significance. Strategies that demonstrate sustainable efficacy over a long period of time would be of greater value than the ones to which the body develops resistance/adaptation over time. Most non-pharmaceutical treatments reduce total and LDL-cholesterol with no or little effects on triglyceride or HDL-cholesterol levels. Modalities that have multiple effects for optimising the circulating lipid profile are preferred over those that only modify 1 of the lipid risk factors.
Cost of treatment
In Australia, a Pharmaceutical Benefits Scheme (PBS) non-concessional prescription for statins, which would lower LDL-cholesterol by 30–40%, costs about $1 per day (the cost to the PBS is about $1.50–$3.00 per day). In comparison, a daily serving of phytosterol enriched spread sufficient to lower LDL-cholesterol by 10% costs the Australian consumer about 17 cents per day.26 Cost of the treatment must be taken into consideration when looking at long-term management of hyperlipidemia.
Adverse health effects
Although statins are generally well tolerated, many clinicians believe that, in practice, statin-related side-effects occur more commonly than reported in randomised trials. Recently, researchers identified a common variant of a gene on chromosome 12 that predisposes patients to statin myopathy.27 Another point of controversy is whether statins cause cognitive problems in some people. Yet another concern about statins and cognition was raised in a recently published Canadian study in which the researchers used a national database to conduct a retrospective analysis of nearly 300 000 patients who had undergone elective surgery. Patients who had been prescribed statins during the previous 90 days had a significantly higher risk for developing post-operative delirium than did statin non-users. Intriguingly, no other class of cardiovascular drugs was associated with postoperative delirium. The authors speculated that altered cerebral blood flow, resulting from the effects of statins on vascular smooth muscle, could be 1 mechanism for statin-induced post-operative delirium. The beneficial effects of statins in high-risk patient populations are indisputable. However, these drugs increasingly are being prescribed to asymptomatic people on the basis of somewhat arbitrary serum lipid thresholds, without regard to overall cardiovascular risk.
Lifestyle factors
Stress management
A number of studies have demonstrated the possible link between stress and hyperlipidaemia. With prolonged stress, the pituitary-adrenal cortical system is activated to secrete cortisol. This is lipogenic and the plasma cholesterol levels can rise up to 60% above baseline.28, 29 An American study including a survey of 187 394 respondents from the Behavioural Risk Factor Surveillance System (BRFSS), aged 35 years or older from 37 states and territories, confirmed the linear relationship between psychological distress and blood cholesterol.30 However, whether stress is the cause or consequence of increased blood cholesterol or whether it is a casual relationship remains unclear. A recent study, in which participants were asked to increase dietary fibre intake to >30g/day; reduce saturated fat intake to <16g/day; trained to reach 70-85% of their maximum heart rate; perform strength training for 3 days/week and engage in 10-20 minutes of stress management activities daily, demonstrated a reduction in the ratio of total to HDL-cholesterol by 8.9% and plasma cholesterol lowering by 7.3%.31
Yoga
Yoga has become increasingly popular in Western cultures as a means of exercise and training fitness. It has been used clinically as a therapeutic intervention and its practice includes muscle stretching, breathing exercises, behavioural modification, and dietary control through mental discipline. An Indian RCT examined the effects of yoga and meditation on biochemical parameters of metabolic syndrome.32 In this study, 101 participants were randomised to receive either the usual care (n = 46) or yogic intervention in addition to usual care for 3 months (n = 55). At the end of the intervention period, plasma triglyceride levels decreased from 210 to 152mg/dL and HDL-cholesterol increased from 33.4 to 44.5mg/dL in the group receiving yogic intervention.
Physical activity and exercise
A 5-year follow-up study of more than 7000 men with average age of 66, demonstrated that physical activity was associated with positive changes to lipid profile.33 Cross-sectional and longitudinal exercise training studies indicate that 15 to 20 miles/week of brisk walking or jogging, which elicit between 5000 to 9000 kilojoules of energy expenditure per week, is associated with triglyceride lowering from 5 up to 38mg/dL and HDL-cholesterol increases of 2 to 8mg/dL. Halverstadt et al.34 showed that endurance exercise training induced favourable changes in plasma lipoprotein and lipid profiles independent of diet and baseline or change in body fat. Another small study involving 12 healthy unfit men and women, subjected to 6 weeks of exercise, demonstrated that endurance training results in a decrease of LDL-cholesterol by 21%, apoB levels by 19% and an increase in HDL-cholesterol by 10%.35 Exercise training rarely alters serum cholesterol or LDL-cholesterol unless dietary fat intake is reduced and body weight loss is associated with the exercise training program, or both. The decrease in plasma triglyceride concentrations is related to baseline concentrations36, 37, 38 with greater reductions in people, previously inactive and higher baseline concentrations.37, 39, 40, 41 Resistance training, however, appears to have no effects on blood lipids, even when initial blood lipid levels are elevated.42–46 A recent Portuguese study compared the effects of 2 exercise programs of 8 months duration on lipid profiles in older women.47 Women (n = 77) aged 60-79 years were randomly assigned to either a multi-component exercise program or resistance exercise program. Significant decreases in plasma triglyceride (−5.1%), and significant increases in HDL-cholesterol (9.3%) were observed in the multi-component exercise group while no significant changes in lipid profile were observed in the resistance exercise group.47
Only a small number of studies have investigated the effects of physical activity on blood lipids and lipoproteins in a race- and sex-specific manner. African American and white participants of the Atherosclerosis Risk in Communities (ARIC) study were investigated for the longitudinal effects of physical activity on plasma lipids and lipoproteins.48 Nine years of follow up data on 8764 individuals aged 45-64 years at baseline demonstrated that increases in the level of activity were associated with increases in HDL and decreases in triglycerides among white participants. Physical activity was associated with reduced LDL in all women, while the association with total cholesterol was limited to African American women.
Nutritional influences
Diet
Diet plays the most important role in the management of hyperlipidemia.
Low (saturated) fat — epidemiological studies
A wealth of epidemiological and interventional studies over the last 60 years has established a link between saturated fat intake and serum cholesterol levels. Perhaps the most quoted of these is the Seven Countries Study,49 in which the dietary habits of 12 763 middle-aged men comprising 16 cohorts from 7 countries were studied, and the relationship to serum cholesterol and coronary disease mortality analysed over subsequent years. This study was carried out between 1958 and 1964, with the information on dietary intake collected by the dietary record method. It allowed inter-cohort comparisons to be made, but analysis on an individual level was not possible. Large variations were seen in the average intake of different saturated fats, and correlations were found between the intake of lauric and myrisitic acids and serum cholesterol increases. In the Western Electric Study,50 1900 middle-aged men randomly chosen from the Western Electric Company’s Hawthorne Works in the Chicago area were analysed for their dietary intake, and serum cholesterol concentrations were measured. The information was collected through interviews and questionnaires by nutritionists. Again, a positive correlation was apparent between serum cholesterol and saturated fat intake. In Belgium, an epidemiological analysis was performed on the differences between the dietary intakes of Belgians living in the north and south of the country.51 Food intake was gathered through 3 independent sources: an investigation of 451 families in the north and 752 in the south, a survey by the Ministry of Agriculture, and through the Ministry of Economic Affairs by way of the National Institute of Statistics. This information revealed a much higher intake of saturated fat in the south compared to the north, and also a lower intake of total polyunsaturated fats in the south. Evidence gathered over 10 years revealed decreasing average serum cholesterol in the north of the country, and a higher serum cholesterol in the south, allowing the authors to conclude a positive relationship between saturated fat intake and serum cholesterol. Kato et al.52 undertook a large scale study of men of Japanese ancestry living in 3 different environments, which was a useful approach as it limited the effects of genetic influences on serum cholesterol changes. Information was collected by 24-hour recall dietary interviews. Dietary intake patterns varied markedly between the men in Japan, Hawaii and California, with serum cholesterol levels showing an apparent positive regression with saturated fat intake.
Low (saturated) fat — interventional studies
Along with epidemiological evidence, there have been a number of interventional studies attempting to establish the link between saturated fat intake and serum cholesterol. Keys et al.53 in 1957 used 66 middle-aged schizophrenic men for a dietary experiment to establish a link between fat intake and serum cholesterol. On a fixed calorie diet, the type of fat fed to the subjects was varied, with 2–9 weeks spent on each experimental diet. The fats used were butter fat, hydrogenated coconut oil, olive oil, cotton-seed oil, corn oil, sunflower-seed oil, safflower oil and fish oil. The percentage of the caloric intake from saturated, monoethenoid and polyethenoid fats were estimated, and serum cholesterol was measured in duplicate at the end of each dietary period. The authors came to the conclusion from their results that saturated fatty acids (especially fats containing 10 or more carbons) such as butter fat and coconut oil have about twice the effect in raising total serum cholesterol as the cholesterol depressing effect of equal amounts of polyethenoid fats. Another major study often used as apparent evidence is that of Hegsted et al.54 Two groups of 10 normocholesterolaemic male subjects were tested whilst being fed diets with fixed fat (38% caloric intake) and protein proportions, with carbohydrates varied to make caloric intake appropriate for each subject. Each test period lasted for 4 weeks, with the type of fat varied (coconut, olive, safflower). Samples taken were measured for total serum cholesterol, beta-lipoprotein cholesterol, total fatty acids, and lipid phosphorus. It was concluded that myristic acid is most hypercholesterolemic. Another highly referenced article on the saturated fat theory is that of Ahrens et al.,55 who examined 40 patients who were either hyperlipidaemic, hypercholesterolaemic or normocholesterolaemic with arteriosclerotic heart disease. The subjects were observed for 4–6 months under controlled dietary conditions, with fixed calories, total fat (40% of total calories), carbohydrates and proteins. The type of fat fed to the subjects varied between corn oil and coconut oil. Serum cholesterol levels were found to be higher on the coconut oil diet (high in saturated fat) and lower on the corn oil diet (high in polyunsaturated fat). Shepherd et al.56 studied the effect of dietary fatty acids on low density lipoprotein (LDL) in 8 young normocholesterolaemic adult males. During study 1, the subjects received a diet rich in saturated fat, derived mainly from dairy products. In study 2, the fat intake from the dairy products was replaced by safflower oil, lower in saturated fat and higher in polyunsaturated fats. Both diets were controlled for total caloric intake and dietary cholesterol. Serum samples were measured for triglyceride, plasma cholesterol, and lipoprotein cholesterol concentrations. It was concluded that compared to the saturated fat diet, the polyunsaturated diet lowered both plasma cholesterol and triglyceride, with 67% of the cholesterol reduction due to a fall in LDL-cholesterol. Similar results were seen by Turner et al.,57 where 15 subjects (7 normal and 8 with type II hyperlipoproteinaemia) were fed diets with 40% calories as either safflower oil or lard. The diets were chosen to maximise the difference in the degree of saturation of the dietary fat whilst maintaining constant cholesterol and total fat intake.
A strict, very low saturated fat, low cholesterol American Heart Association Step 2 diet only minimally lowers serum cholesterol. A 5% reduction in LDL-cholesterol in patients following this program was reported and, discouragingly, an equivalent 6% fall in HDL-cholesterol, so that ratios were unchanged.58 Low-fat diets as commonly prescribed rarely produce significant LDL declines. Studies performed on controlled metabolic units where intakes are rigidly enforced can demonstrate cholesterol reductions of 15% with diet alone; however, in the real world, people can rarely replicate these results.59 One exception to this, however, is the Dean Ornish-style diet, which was studied in the Lifestyle Heart Trial.60 This vegetarian diet consists of fruits, vegetables, soybean products, non-fat milk, and yoghurt with no oils or animal fats. Roughly 7% of calories are from fat, 15% to 20% from protein, and the remainder from complex carbohydrates. Only 12mg of cholesterol per day is allowed. On average, Ornish’s patients had a 37% reduction in LDL-cholesterol levels (HDL-cholesterol levels were unchanged).
What is most provocative about this diet/lifestyle program is that there was a 91% reduction in angina frequency and a significant degree of angiographically measured coronary stenosis regression. It is unclear to what degree other lifestyle modifications, such as exercise and stress reduction, which are integral parts of the Ornish program, play in these results. The problem with the Ornish diet is that it is so stringent that most Americans find adhering to it nearly impossible. In addition, critics of this study note that it had only 48 subjects; thus, the outcome should be viewed sceptically until larger trials are completed. The greatest scientific objection to the Ornish-style diet is that it is now known that high-carbohydrate, low-fat diets raise triglyceride levels, lower HDL levels, and may convert LDL lipoproteins into smaller, denser, and more atherogenic particles.61 Nevertheless, the Ornish diet provides the greatest absolute LDL reduction available by diet alone and is of a magnitude similar to that of high-dose statin therapy, which can reduce cholesterol by 25% to 60% depending upon the drug dose.62 A recent meta-analysis of 60 controlled trials revealed that as the chain length of the saturated fatty acids increase, their cholesterol-raising effects tapers off. Accordingly, lauric acid (C12:0) is most hypercholesterolemic and the longer chain stearic acid (C18:0) in fact is cholesterol neutral or even slightly hypocholesterolemic.63 Based on the above evidence, most international dietary guidelines recommend that total fat intake should be limited to 30% of daily energy intake with saturated fat contributing no more than 10% of daily energy intake to control blood lipid levels. Families with high cardiovascular risk factors such as familial hypercholesterolemia may also warrant for children to be on a diet low in saturated fats and cholesterol. Researchers demonstrated a diet low in saturated fats (30–35% of daily energy) and cholesterol (less than 200mg/day) in early children, aged 7 months to 5 years, reduced cholesterol levels by 3–5% compared with controls without affecting development which may reduce the risk of cardiovascular disease in adulthood.64 The authors warned against over-restricting dietary fat intake in young children.
Monounsaturated fats
A large majority of the published literature suggests that consumption of monounsaturated fatty acids (MUFA), primarily oleic acid rich sources including olive oil, high oleic safflower oil, canola oil, sunola (genetically modified sunflower) oil, macadamia oil and avocado oil, are cholesterol neutral; that is, they do not significantly affect plasma cholesterol. Therefore, not surprisingly, MUFA consumption is not factored in any of the equations used to predict the change in blood cholesterol levels such as those put forward by Hegsted et al.54 and Keys.65 Intervention studies involving 24–28% of daily energy in the form of MUFA conducted in the 1980s reported reduction in LDL-cholesterol to the same extent to that of a low fat, high-carbohydrate diet.66
Monounsaturated fats and the Mediterranean diet
More widely studied and perhaps more practical for the treatment of patients with coronary artery disease is the Mediterranean diet rich in MUFA. In the 1950s, Ancel Keys began studying the dietary habits of 1770 inhabitants of various countries and correlating them with subsequent mortality.67 His landmark study found that the mortality rates from heart disease were 2–3 times lower in the countries bordering the Mediterranean Sea compared with Northern Europe and the USA. Notably, studies conducted in North America, where MUFA source was not olive oil but other plant or animal oils, failed to demonstrate benefits of MUFA-rich diets, raising possibilities of benefits of Mediterranean diet components other than MUFA. Another potential mechanism is that a diet rich in fruits and legumes provides folic acid, which may reduce cardiac risk by lowering plasma homocysteine.68 Also, moderate alcohol consumption is associated with decreased cardiovascular risk, in part by increasing HDL levels,69 and both red wine and some Mediterranean plant foods contain large amounts of flavonoids, which are natural antioxidants and antithrombotic substances.70 But the most provocative explanation is that the Mediterranean diet contains α-linolenic acid which is an omega-3 fatty acid and has been shown to possess antithrombotic properties and may also be antiarrhythmic.71, 72 This α-linolenic acid is a precursor of other omega-3 fatty acids found in fish and fish oil, such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which may have independent beneficial effects that are discussed later in this review.
Polyunsaturated fats
Most polyunsaturated fatty acids in the diet belong to the omega-6 (mainly linoleic acid) family, present in large amounts in seed oils such as corn, sunflower, soybean and cottonseed. Consumption of these has been shown to lower serum cholesterol, LDL-cholesterol and, in clinical trials, the risk of heart disease. Every 1 gram increase in linoleic acid consumption resulted in plasma cholesterol lowering by 1mg/dL.73 Increased consumption of linoleic acid may induce increased expression of hepatic LDL-receptors, thereby enhancing increased LDL uptake in the liver for further metabolism.74
Controversy surrounds omega-6 polyunsaturated fatty acids, because even though they lower LDL-cholesterol levels, excessive intakes do not appear to be correlated with cardiovascular benefit.75 Recently, Jakobsen et al.76 pooled data on diet and the incidence of heart disease in 340 000 people from the United States, Scandinavia, and Israel. Metabolic trials of diet and blood lipids show that replacing 5% of energy from saturated fatty acids with polyunsaturated fatty acids reduces the serum total/HDL-cholesterol ratio by 0.17.77 In prospective observational studies, such a reduction in the total-to-HDL-cholesterol ratio is associated with a reduction in heart disease risk of 9%.78 The effect of omega-6 fatty acids on blood lipids, combined with prospective data on blood lipids and heart disease, predicts a 9% risk reduction. The randomised clinical trials predict an 8% reduction, and the observational studies pooled by Jakobsen et al.76 predicted a 13% reduction for people who eat 5% of calories as polyunsaturated instead of saturated fatty acids.
Tree nuts
Nuts are energy-rich foods and are an excellent source of unsaturated fatty acids. The favourable fatty acid profile perhaps contributes to the health benefits of nuts observed in epidemiologic studies and cholesterol-lowering potential in feeding trials.79, 80 Besides, the nuts contain many bioactive compounds such as vegetable protein, fibre, minerals, vitamin E, and polyphenols.81 RCTs involving dietary supplementation with peanuts, walnuts, pistachio nuts, almonds, hazelnuts and macadamia nuts have demonstrated a reduction in serum total cholesterol and LDL-cholesterol.
A systematic review of studies investigating independent effects of nuts show reduction in total cholesterol between 2–16% and LDL-cholesterol between 2–19% in subjects consuming almonds or walnuts or pecan nuts or peanuts or macadamia nuts compared with those consuming control diets.79 Another review of clinical studies concluded that tree nuts lower LDL-cholesterol by 3–19% compared with Western and lower-fat diets.80 In summary, nuts as part of a healthy diet can play an important role in maintenance of blood cholesterol levels. Of all the nuts, walnut is the most extensively studied tree nut and appears to possess hypocholesterolemic properties. A recent crossover randomised control trial in which 25 normal or mildly hypercholesterolemic subjects were supplemented with 42.5g of walnuts daily for 4 weeks, confirmed serum cholesterol reduction of 9.5% and LDL-cholesterol reduction of 5.2%.82
High-protein diets
One of the initial concerns with the high-protein diets for weight loss, such as the Atkins diet, was that it allows unrestricted fat consumption, including saturated fats known to increase total and LDL-cholesterol. When the Atkins diet was studied by Samaha83 in comparison to a low-fat diet (16% fat) in severely obese subjects, they found that the high-protein diet significantly lowered triacylglycerol (TGL) by 20% versus 4% in the low-fat group (p = 0.001). The Atkins diet was also tested in a study by Foster,84 where at 3 months a significant reduction in LDL-cholesterol and triglyceride and a significant increase in HDL-cholesterol were found, compared to a low-fat diet group. Changes in LDL-cholesterol were not maintained at 1 year, therefore significant differences between the groups was lost. In view of the fact that adherence to the diet was very poor, the relevance of this is not yet clear.
Other studies85, 86 demonstrated significant reductions in triglyceride and oxidised LDL-cholesterol, with high-protein diets. By contrast, Parkers study87 in 54 type-2 diabetics on a high-protein diet (30% protein) compared to a high-carbohydrate group (15% protein), did not find any significant changes in triglyceride. Findings in regards to both LDL-cholesterol and HDL-cholesterol are even more varied. In a systematic review on low-carbohydrate diets, Bravata88 found that no change was detected overall in any serum lipids. They note that the studies were few in number and there was a wide variety in the design. However, from limited evidence, it does appear that higher protein diets do not have any adverse effects on total and LDL-cholesterol, though their effect on HDL-cholesterol is less clear. While more research is needed in these areas, it appears that moderately high-protein diets are not harmful to cardiovascular health and may indeed be beneficial.
Low carbohydrate, high vegetable protein and vegetable oil diet (‘Eco-Atkins’)
A 4-week trial of 47 overweight hyperlipidemic men and women randomised to consume either a low-carbohydrate (26% of total calories), high vegetable protein (31% from gluten, soy, nuts, fruit, vegetables, and cereals), and vegetable oil (43%) plant-based diet — termed the ‘Eco-Atkin diet’ — was compared to a high-carbohydrate lacto-ovo vegetarian diet (58% carbohydrate, 16% protein, and 25% fat), with both diets providing 60% of calorie requirements.89
A dietary portfolio for hyperlipidemia
Efforts to lower cholesterol through dietary manipulations have had only modest effects. In an attempt to increase the efficacy of diet in the prevention of cardiovascular disease, the Adult Treatment Panel of the National Cholesterol Education Program has recommended adding plant sterols and viscous fibres to the diet.20 Soy proteins and tree nuts may have additional health benefits. Jenkins and colleagues examined the cholesterol-lowering potential of a diet low in saturated-fat that included these ingredients.90 Forty-six hyperlipidemic, otherwise healthy subjects completed the 4-week study. After 4 weeks of following their own diet that was low in saturated fat, participants were randomised into 1 of the following groups: a very-low-saturated-fat diet without a statin control group; the same diet with a statin; or a similar diet with added viscous fibres, plant sterols, soy foods, and almonds (portfolio diet).
After 4 weeks, the control group lowered their LDL-cholesterol by 8% and increased the LDL-cholesterol to HDL-cholesterol ratio by 3%. The group receiving a statin lowered their LDL-cholesterol by 30.9% and decreased the LDL-cholesterol to HDL-cholesterol ratio by 28.4%. The portfolio diet group lowered their LDL-cholesterol by 28.6% and decreased the LDL-cholesterol to HDL-cholesterol ratio by 23.5%. Clearly the reductions in blood lipid levels in the statin and portfolio diet groups were considerably greater than the changes in the control group; however, no significant differences were apparent in the statin versus the portfolio diet groups. The authors concluded that diet alone, if selecting for foods with a combination of cholesterol-lowering properties, can lower cholesterol to the same extent as statins.90 Compliance in all the 3 groups was reported to be 93%. These results were subsequently confirmed by another similar study.91 The long-term sustainability of clinically meaningful reduction in LDL-cholesterol of >20% by dietary means in motivated individuals has also been reported.92
Additional benefits of a portfolio diet include weight loss,92, 93 reduced blood pressure,93 and reduced inflammation as indicated by a reduction in CRP levels.90, 94 It has also been shown that the reduction in serum cholesterol following the consumption of the portfolio diet is attributable to decrease in the level of the highly atherogenic, smallest subclass of LDL.95 More importantly, these health benefits can be achieved without side-effects. Notably the portfolio diet had no effect on the HDL-cholesterol or triglyceride levels. Long-chain omega-3 fatty acids, particularly docosahexanoic acid (DHA), is known to decrease triglyceride and increase HDL-cholesterol levels, therefore, addition of DHA may enhance the lipid-lowering potential of the portfolio diet.
Alcohol
Moderate alcohol consumption is associated with decreased cardiovascular risk in part by increasing HDL levels.69 Red wine, rich in flavonoids, a natural antioxidant with antithrombotic properties, is particularly more beneficial.70
Grapefruit juice
Israeli grapefruit juice, with a high level of bioactive compounds, has been shown to possess cholesterol-lowering properties. An RCT of 72 hypercholesterolemic patients were divided into either a control group or experimental groups supplemented daily with 100 or 200 mL of fresh grapefruit juice for 30 days.96 Following the intervention period, total cholesterol decreased by 9.5%, and 16.1%; LDL-cholesterol by 11.6% and 21.0%; and triglycerides by 11.5%, and 24.7% in the groups supplemented with 100mL and 200 mL of grapefruit juice respectively. In a follow-up study by the same authors,97 the lipid-lowering potential of red versus blonde grapefruit was compared. Fifty-seven hypercholesterolemic patients, after coronary bypass surgery, were divided into either a control group or experimental groups supplemented daily with 1 equal weight of red or blond grapefruit. Following the 30-day intervention period, total cholesterol decreased by 15.5%, and 7.6%; LDL-cholesterol by 20.3% and 10.7%; and triglycerides by 17.2%, and 5.6% in the red and blond grapefruit fed groups respectively.97 It is conceivable that addition of grapefruit (especially red variety) juice may be beneficial for hypercholesterolemic individuals in a dose-dependent manner. The magnitude of the lipid-lowering following red grapefruit consumption should prompt further interest in this food as part of a healthy diet.
However, care is required as grapefruit juice is known to interact and augment the drug bioavailability with many pharmaceutical drugs. (See chapter on Herb-drug interactions). The mechanism for this interaction is via the inhibition of cytochrome P-450 3A4 in the small intestine, reducing the metabolism of the drug, and also the inhibition of P-glycoprotein resulting in further increases in absorption of the drug, potentially leading toxic levels.98 Drugs metabolised by the pathways that are most affected by grapefruit juice include some calcium channel antagonists (e.g. nifedipine, verapamil), blood thinning medications such as warfarin (increasing risk of bleeding), benzodiazepines (e.g. midazolam and diazepam increasing risk of sedation), HMG-CoA reductase inhibitors/statins (increasing risk of side-effects such as myopathies) and cyclosporine. Even a single glass of juice can produce a significant interaction.99
Soybean products
Soybean-derived protein has been shown to possess considerable cholesterol-lowering potential in clinical studies involving hypercholesterolemic subjects. In 1995, a meta-analysis concluded that partial or full replacement of dietary animal proteins by soy protein resulted in an average reduction of 23mg/dL in plasma total and 22mg/dL in LDL-cholesterol concentrations.100 The observed effects of soybeans on plasma lipids were not extended to triglycerides or HDL-cholesterol. Moreover, reductions in plasma cholesterol were dependent on baseline levels with greater reductions noted in subjects with established hypercholesterolemia.100 Another recent meta-analysis confirmed these effects of soy proteins.101 It has been shown that the cholesterol-lowering ability of soy proteins may be attributed to its ability to up-regulate apo-B receptor gene expression.102, 103
Another component of soybeans, isoflavones, structurally similar to oestrogen, have been examined for their cholesterol-lowering potential. Isolated soy isoflavones introduced in amounts from 28–150mg have achieved statistically insignificant reductions in LDL-cholesterol in the range of 1–6.5%.104 These minor declines in non-HDL/LDL-cholesterol concentrations would be of little clinical significance in terms of a reduction in the risk of developing coronary artery disease, but when combined with dietary changes may have an additive beneficial effect.
Based on the published scientific evidence, the United States Food & Drug Administration issued a health claim that 25g/day of soy protein, when supplemented in the diet may significantly reduce the risk of cardiovascular disease via an average fall of up to 10% in plasma cholesterol levels, depending on initial values.105
Nutritional supplements
Phytosterols
Phytosterols, also referred to as plant sterols are structurally similar to cholesterol, with the same basic functions in plants as cholesterol in animals; that is, to regulate membrane fluidity and other physiological functions associated with plant biology.106 The only difference between phytostanols and phytosterols is the saturation of the double bond, consequently the former are less abundant in nature.107
Phytosterols are effective in reducing the absorption of both dietary and biliary cholesterol from the gastrointestinal tract, by displacing cholesterol from micelles.107–110 The inhibition of cholesterol absorption by this mechanism produces a state of relative cholesterol deficiency, which is followed by an up-regulation of cholesterol biosynthesis and LDL-receptor activity.110 Chronic phytosterol feeding studies, show whole body cholesterol biosynthesis increases by 38–53%, LDL-receptor expression increases by 25–45%, VLDL-cholesterol production by the liver was reduced by 20% and plasma concentration of dense LDL-cholesterol was reduced by 22%.111, 112 Cholesterol-lowering potential of phytosterols were first documented more than 50 years ago,113 however a fortified functional food (fat spread) was developed in 1995 and since then a number of studies have investigated the safety/efficacy of the spread to modify blood lipids.114, 115 Research has demonstrated that plant sterol and stanol ester-enriched margarine spreads lower LDL-cholesterol by 9–14%.116 Maximal LDL reduction is achieved at plant sterol or stanol ester doses of 1.6–2.0g/day.117, 118 Plant sterols also provide additional LDL-lowering when used in conjunction with statins.117, 119 It should be noted that neither phytosterols nor statin drugs have any significant effect on plasma triglycerides. Recent studies have shown that combined plant sterols and long-chain omega-3 fatty acid supplementation have complementary and synergistic lipid-lowering effects.120, 121 Therefore, for optimisation of blood lipid profile in order to maximise cardio-protection, it may be advisable to develop functional foods with the 2 supplements together.
In the 21st century, plant sterols have been added to other food matrices, including juices, non-fat beverages, milk and yoghurt, cheese, croissants, muffins, cereal bars and chocolates.122 Plant sterol-enriched fermented milk can significantly reduce LDL-Cholesterol and also triglyceride levels in moderately hypercholesterolemic patients. A multi-centre, randomised, double-blind, placebo-controlled, parallel clinical trial of 83 hypercholesterolemic patients who received a 100 ml serving of either plain (control) low-fat or phytosterol enriched (1.6g of free sterol equivalents) drinkable yoghurt per day along with their main meal for 42 days123 demonstrated a significant reduction in LDL-cholesterol without affecting the HDL-cholesterol.
Efficacy of phytosterols in low-fat or non-fat products may be a concern, however, fortified low-fat dairy products have been shown to be as effective as fortified fat spreads for lipid-lowering.115, 122 The beneficial physiologic effects of plant sterols could be further enhanced by combining them with other beneficial foods and substances, such as olive and fish oils, fibres, and soy proteins, enhanced by the additive effects of exercise. In 2006 Food Standards Australia New Zealand (FSANZ) granted permission to market plant sterols in low-fat milks, yoghurts and breakfast cereals. A meta-analysis of 6 randomised controlled intervention trials investigated the effects of phytosterols/stanols on lipid concentrations in familial hypercholesterolemic subjects that used fat spreads (dosages ranging from 1.6–2.8g/day) over a 4–12 week period, and found fat spreads enriched with 2.3 +/– 0.5 gram phytosterols/stanols per day significantly reduced total cholesterol by 7–11% and LDL-cholesterol from 10–15% compared with control. There were no changes in triglyceride and HDL-cholesterol concentrations.124
Vitamin B3 — niacin or nicotinic acid
Niacin or nicotinic acid appears to lower LDL-cholesterol and increase HDL-cholesterol. Vitamin B3 includes niacin (nicotinic acid) and niacinamide (nicotinamide), although niacinamide has no effect on lipid levels in patients with hyperlipidemia. Well-designed studies have found that niacin/nicotinic acid lowers LDL-cholesterol by approximately 10%, lowers triglycerides by 25%, and raises ‘good’ HDL-cholesterol by 15% to 30%. When compared with statins, niacin can raise HDL levels up to 5 times although statins are more effective in lowering total and LDL-cholesterol.125–128 In a randomised open-label controlled (n = 30) study of 6 months duration, extended release niacin (1000mg/day) significantly reduced LDL-cholesterol by 24% and triglycerides by 12% in patients with impaired glucose tolerance.129
Combined extended release niacin and statin therapy
Niacin combined with statins may provide additional benefit for achieving LDL-cholesterol, non-HDL-cholesterol, HDL-cholesterol and triglyceride target goals for cardiovascular prevention. A number of trials demonstrated that combined niacin and statins have significant additional benefits of lowering total cholesterol, LDL-cholesterol, triglyceride and raising HDL-cholesterol levels compared with statins alone, and for prevention of coronary artery disease.130–134 Extended-release niacin (1000mg/day) combined with simvastatin (20mg) reduced LDL-cholesterol by 6%, non-HDL-cholesterol by 7% and triglycerides by 13%, and raised HDL-cholesterol by 11% compared to simvastatin alone, over a 52-week period. The higher niacin dose of 2000mg combined with simvastatin 20–40mg reduced LDL-cholesterol by up to 24%, non-HDL-cholesterol by up to 28%, and triglycerides by up to 34%, and increased HDL-cholesterol by up to 22% compared to similar dose simvastatin monotherapy.135 A randomised study of 520 patients with mixed dyslipidemia over a 52-week period compared niacin extended release combined with simvastatin therapy (dosage of 2000/40mg/day) to simvastatin monotherapy136 and examined their safety and efficacy.136 Combined niacin/simvastatin therapy was well tolerated with about 70% of patients experiencing mostly mild–moderate flushing that subsided over time and 20% of participants withdrew from the treatment group due to side-effects (7% due to flushing). Overall, when compared with simvastatin monotherapy, combined niacin/simvastatin therapy significantly reduced non-HDL-cholesterol and LDL-cholesterol levels, increased HDL-cholesterol and reduced triglyceride levels.
Niacin may also play a role in metabolic syndrome. A recent study compared the effects of aerobic exercise and extended-release niacin on post-prandial triglyceride levels in 15 men with the metabolic syndrome over a 16-week period.137 This study reported that aerobic exercise lowers the postprandial triglyceride response to a high-fat meal, whereas niacin lowered fasting but not postprandial triglycerides. When the 2 were combined, niacin attenuated the triglyceride-lowering effect of exercise and decreased postprandial insulin concentrations after niacin administration.137
Mechanism of action
There are several possible mechanisms of action for niacin. These include inhibiting free fatty acid release from adipose tissue, inhibiting hepatic diacylglycerol acyltransferase (DGAT), resulting in inhibition of triglyceride synthesis and reducing apolipoprotein B-containing lipoproteins and reducing the rate of synthesis of LDL-cholesterol and VLDL-cholesterol.138, 139, 140
Viscous (soluble) fibre
Soluble fibre appears to reduce LDL-cholesterol by reducing cholesterol absorption in the intestines. Soluble fibre binds with cholesterol so that it is excreted. Soluble fibre can be found as a dietary supplement, such as psyllium powder, or in foods such as oats, barley, rye, legumes (peas, beans), some fruits such as apples, prunes, and berries and some vegetables, such as carrots, brussel sprouts, broccoli, and yams. Five to 10g a day of soluble fibre has been found to decrease LDL-cholesterol by approximately 5%. Well-controlled intervention studies have now shown that 4 major water-soluble fibre types — β-glucan, psyllium, pectin and guar gum — effectively lower serum LDL-cholesterol concentrations, without affecting HDL-cholesterol or triglyceride concentrations. It is estimated that for each additional gram of water-soluble fibre in the diet, serum total and LDL-cholesterol concentrations decrease by -0.028mmol/L and -0.029mmol/L, respectively.141
Oats and barley
Several studies have been carried out on the cholesterol-lowering effects of oats, which were later found to be due to their β-glucan content.142 Results of several uncontrolled metabolic ward trials have been summarised by Anderson et al. and reductions in serum total cholesterol (mainly LDL-cholesterol) from 13% to 26% were reported,143 however a few studies demonstrated virtually no benefit.144, 145, 146 Although a few individual studies showed virtually no effects, a number of meta-analyses concluded that water-soluble fibre from oat products effectively lowered serum total and LDL-cholesterol concentrations.147, 148, 149 Brown et al. estimated that 1g of water-soluble fibre from oats lowered total and LDL-cholesterol concentrations with −0.037mmol/L and −0.032mmol/L, respectively.149 Obviously, more research is needed to confirm the cholesterol-lowering effects of this source of β-glucan and its potential beneficial effects on HDL-cholesterol concentrations. A recent systematic review of 8 RCTs (n = 391 patients) of 4–12 weeks’ duration evaluated the lipid-lowering effects of barley, another source of β-glucan.150 The use of barley significantly lowered total cholesterol (–13.38mg/dL), LDL-cholesterol (–10.02mg/dL) and triglycerides (–11.83mg/dL) but did not appear to significantly alter HDL-cholesterol.
Psyllium
Psyllium has been shown to reduce total cholesterol and LDL-cholesterol levels in animals and humans. One study demonstrated a 3.5% reduction in total cholesterol and a 5.1% reduction in LDL-cholesterol levels after consuming 5.1g of psyllium husk twice daily for 8 weeks.151
Another study began with individuals on the American Heart Association Step-1 diet, then with the addition of 8 weeks of psyllium supplements, resulted in decreased total cholesterol (4.8%) and LDL (8.8%).152 An analysis of all double-blind studies concluded that psyllium-enriched cereals lowered cholesterol levels by 5% and LDL by 9%.153 In a study examining age and gender differences in the effect of psyllium on blood lipids, men and pre- and post-menopausal women were given psyllium or placebo. Psyllium lowered plasma LDL-cholesterol levels by 7–9% in all groups. Triglyceride levels were lowered by 17% in men, but increased by 16% in post-menopausal women. Pre-menopausal women displayed no significant shift in triglycerides.154
Pectin
Keys et al.155 published the first human study involving 24 healthy subjects that suggested that pectin supplementation lowered serum total cholesterol concentrations. Consumption of biscuits with pectin (15g/day) reduced total cholesterol by 5%. Since then, many studies have confirmed that pectin lowers serum cholesterol levels in hypercholesterolemic as well as normocholesterolemic subjects. All sources of pectin, including guava fruit, prunes, grapefruit gelatin capsules, and citrus pectin desserts were all effective. Despite some controversy,156, 157 meta-analysis by Brown et al.149 concluded that pectin effectively lowered total and LDL-cholesterol concentrations. The range of effects on total cholesterol varied from –16% to –5%. On average, each gram of pectin decreased total and LDL-cholesterol concentrations by –0.070mmol/L and –0.055mmol/L respectively. Pectin did not significantly alter serum HDL-cholesterol and triglyceride levels.
Guar gum (Cyamopsis tetragonoloba)
Guar gum, a bulk laxative, is not only used to relieve constipation but also to decrease serum cholesterol concentrations. Fahrenbach et al. were the first to report that guar gum effectively reduced serum cholesterol levels in normocholesterolemic subjects.158 Since then, this serum lipid-lowering effect of guar gum has been investigated in a large number of human trials. The results of these studies were consistent in that total and LDL-cholesterol were effectively decreased by guar gum supplementation, whereas HDL-cholesterol and triglyceride remained unchanged. From their meta-analysis, Brown et al. estimated that 1g of water-soluble fibre from guar gum lowered serum total and LDL-cholesterol by –0.026mmol/L and –0.033mmol/L respectively.149 Guar gum lowered total cholesterol concentrations in healthy and hyperlipidemia subjects, and in subjects with diabetes mellitus. Guar gum exhibited additional cholesterol-lowering effects in subjects already receiving lipid-lowering drugs.
Glucomannan
Glucomannan, another soluble fibre derived from Amorphophallus konjac, available in numerous over-the-counter products, such as Lipozene®, has been the subject of several intervention trials evaluating its influence on blood lipids.159–162 A meta-analysis of 14 RCTs, including patients receiving glucomannan, had statistically significantly lower total cholesterol, LDL-cholesterol, and triglycerides; however, the use of glucomannan did not appear to alter HDL-cholesterol.163
Fish oil
Omega-3 fatty acids are pleiotropic molecules with the potential to play a key role in the management of hyperlipidemia for the prevention of coronary heart disease. Supplementation with omega-3 fatty acids favourably modifies serum lipids; the most consistent finding being a drastic reduction in fasting and postprandial triglycerides levels.164 This has been observed with EPA and DHA alone165 and with their combination in fish oil.
Grimsgaard et al.166 reported on the effects of supplementation with highly purified eicosapentanoic acid (EPA) (3.8 g/d) or docasahexanoic acid (DHA) (3.6 g/d) for 7 weeks in healthy, non-smoking male volunteers. They found a reduction in plasma triglycerides that was at least as marked in the DHA group (26%) as in the EPA group (21%). In addition, HDL-cholesterol increased only in the DHA group.166 These results provide convincing evidence that EPA and DHA are equally effective at reducing serum triglycerides, but that DHA may raise HDL-cholesterol as well as LDL particle size (i.e. both anti atherogenic outcomes). Omega-3 fatty acids have contrasting effects on LDL-cholesterol, with a general tendency toward slightly increased LDL-cholesterol concentrations, however the size of the LDL molecule is also increased, which is thought to be less atherogenic.167
A recent meta-analysis quantitatively evaluated RCTs of fish oils in hyperlipidemic subjects.168 The final analysis comprising of 47 trials showed that consuming fish oils (average intake of 3.25g/day of EPA/DHA) produced a clinically significant reduction of triglyceride (–0.34mmol/L), no change in serum cholesterol (–0.01mmol/L) and slight increase in HDL (0.01mmol/L) and LDL-cholesterol (0.06mmol/L). The reduction in triglyceride concentration correlated with both EPA/DHA intake and initial triglyceride levels. A recent trial supports the observations that dietary supplementation with a DHA rich oil, reduces plasma triglyceride by 22.3% and increases HDL-cholesterol by 7.1% with no significant change in total or LDL-cholesterol.120
A systematic review comparing the effects of lipid-lowering interventions for the prevention and treatment of hyperlipidemias concluded that statins and omega-3 fatty acids are by far the most favourite agents to reduce the risk of cardiovascular disease.169 Another recent study demonstrated that fish oil supplements may work slightly better than a popular cholesterol-reducing drug to help patients with chronic heart failure.170 Indeed, combined therapy with cholesterol-lowering agents (statin drugs or phytosterols) and omega-3 fatty acid may offer complementary or even synergistic effects on blood lipid levels.120, 121, 171 Monotherapy with statins or phytosterols may not be sufficient to treat target goals for hyperlipidemia, especially given their modest effects on triglyceride concentration, and co-supplementation with omega-3 fatty acids may optimise plasma lipid profile in people with mixed hyperlipidemia.
Herbal therapies
Guggulipid
One trial studying the effects of guggul reported that serum cholesterol dropped by 17.5%.172 In another report comparing guggul to the drug clofibrate, average fall in serum cholesterol was slightly greater in the guggul group; moreover, HDL-cholesterol rose in 60% of people responding to guggul, while clofibrate did not elevate HDL.173 In another Indian placebo-controlled study from 1994, guggulipid lowered the average level of total cholesterol by 11.7%, LDL-cholesterol by 12.5%, triglycerides by 12% and total cholesterol/HDL ratio by 11.1%.174 In the first clinical trial of guggul extract outside of India, neither the commonly used dose, nor a high dose of standardised guggul improved any of the measured levels of lipoproteins in a sample of 103 healthy patients with hypercholesterolemia (moderate) and eating a Western diet.175 Guggul also appeared to cause a dermatologic hypersensitivity reaction in some patients
A recent Norwegian double-blind, randomised, placebo-controlled trial including 43 women and men, age 27–70 years, with moderately increased cholesterol, randomised to use 2160mg guggul daily, or a placebo for 12 weeks, showed a significant decrease in serum cholesterol and HDL-cholesterol with no change in LDL-cholesterol, triglycerides, and total cholesterol/HDL-C ratio between the 2 groups.176 Further larger studies are needed to establish effects and safety of guggul-based formulations in the treatment for hypercholesterolemia.
Artichoke leaf extract
Artichoke (Cynara scolymus) leaf extract (ALE) is a herbal remedy marketed as an aid to lowering cholesterol. ALE may work by limiting the synthesis of cholesterol in the body. Artichokes also contain a compound called cynarin, believed to increase bile production in the liver and speed the flow of bile from the gallbladder, both of which may increase cholesterol excretion. A review of 11 clinical studies conducted between 1936–1994 on the lipid-lowering effects of ALE showed an average decrease in either total cholesterol or triglycerides of between 5% and 45%,177 although the robustness of some of the trial designs is unclear.
In a recent UK study, 75 hypercholesterolemic volunteers were randomised to examine the effects of feeding 1280mg of a standardised ALE, or a matched placebo, daily for 12 weeks.178 Plasma total cholesterol decreased in the treatment group by an average of 4.2%. No significant differences between groups were observed for LDL-cholesterol, HDL-cholesterol or triglyceride levels. An Indian study including 30 volunteers with type II diabetes reported that 6g of globe artichoke powder per day for 90 days significantly lowered total cholesterol by 11mg/dL, LDL-cholesterol by 17mg/dL (9%), triglyceride by 18mg/dL (9.5%) and surprisingly increased HDL-cholesterol by a massive 38% or 9mg/dL, compared to the baseline values.179 A meta-analysis looked at RCTs for artichoke extract for high cholesterol.180 Two trials involving a total of 167 people met the quality criteria. One trial found artichoke significantly reduced total cholesterol after 42 days of treatment.181 The other study found artichoke significantly reduced total cholesterol in a subgroup of patients with total cholesterol levels of more than 230mg/dl.182 Adverse events were mild, transient and infrequent. Larger clinical trials over longer periods are needed.
Garlic extract
There have been numerous studies with conflicting results regarding garlic’s ability to lower lipids. Positive findings in 3 trials exhibited a lowering of cholesterol from 6.1 to 11.5%, primarily due to the lowering of LDL levels over a 1–4 month period.183, 184, 185 More recent studies have yielded conflicting results.186, 187 A 12-week study using garlic powder in ambulatory patients resulted in a 14% reduction of serum cholesterol. An earlier meta-analysis of the controlled trials of garlic to reduce hypercholesterolemia suggested a significant reduction in total cholesterol levels.188 The best available evidence suggests that garlic, in an amount approximating one-half to 1 clove per day, decreased total serum cholesterol levels by about 9% in the groups of patients studied. It should be noted that only 5 of 28 studies were selected for review while the rest did not meet the criteria for homogeneity with respect to study design, patient characteristics, interventions, duration of therapy, and cholesterol measurements. Another meta-analysis of randomised double-blind, placebo-controlled clinical trials published in 2001 suggested that garlic is superior to placebo in reducing serum cholesterol levels, however, the effect size is modest, and the robustness of the effect is debatable, raising doubts about the treatment of hypercholesterolemia by garlic use.189 A recent systematic review evaluated the effects of garlic on cholesterol levels in both healthy and hypercholesterolaemic subjects. RCTs with garlic ranging from 11–24 weeks in duration concluded that garlic therapy did not produce any statistically significant reduction in serum total cholesterol levels.190 As moderate to high heterogeneity exists among pooled studies, the available evidence from RCTs does not demonstrate beneficial effects of garlic on serum cholesterol.
Other supplements
Policosanols
Policosanol is a natural product derived from sugar cane wax, which may inhibit cholesterol synthesis although studies have demonstrated conflicting results. A single daily dose of 5–10mg policosanol reduced cholesterol by 8–18% and LDL-cholesterol by 11–28% (equivalent to low dose statin) within 2 months of therapy. It also increased HDL-cholesterol from 10–29%.191–194 More than 80 placebo-controlled or comparative trials suggest that policosanol at doses of 5–40mg/d has lipoprotein-lowering effects comparable with statins.
Hypocholesterolemic effects of policosanol have been compared with lipid-lowering drugs, bezafibrate195 and statins.196 A multi-centre controlled double-blind randomised trial in 113 hypercholesterolemic subjects demonstrated that a daily dose of 10mg of policosanol possessed superior lipid-lowering effects compared to 400mg/day dose of bezafibrate.195 Another double-blind randomised study conducted in Chile showed greater lipid-lowering effects of policosanol compared with statins.197 In this trial, Frencini-Presenti et al.197 failed to demonstrate cholesterol-lowering potential of policosanol at a dose of 20mg/day for 8 weeks. Another randomised, double-blind, placebo-controlled, parallel-group trial conducted in Germany using a daily dose of up to 80mg of policosanol for 12 weeks showed no significant effects on blood lipids.198 Yet another randomised, parallel, double-blind, double-dummy, placebo-controlled trial199 with policosanol with or without statin therapy failed to show cholesterol-lowering effects and the authors suggested that policosanol should be added to the list of nutritional supplements lacking scientific validity to support their use. A recent study demonstrated that dietary supplementation with 30mg/day of octacosanol (policosanol) for 4 weeks did not alter blood lipid profile; however, neutral sterol and bile excretion in the faeces decreased following the intervention suggesting a systemic effect of policosanol on cholesterol metabolism.200 A meta-analysis of 4596 patients from 52 eligible studies that compared the benefits of policosanol and plant sterols and stanols with placebo, found that policosanol affected total cholesterol, HDL-cholesterol, triglyceride levels more favourably than plant sterols and stanols.201 Both groups had favourable safety profile. The net reduction of LDL-cholesterol were –24% for policosanol versus –10% for plant sterols (p<0.0001) after accounting for the placebo groups, and a clinically significant decrease in the LDL:HDL ratio with the policosanol group.
However, a number of recent RCTs for policosanol suggest it has no benefit for the treatment of hypercholesterolemia demonstrating no significant change in LDL-cholesterol levels or reduced LDL oxidation compared to control in hypercholesterolaemic individuals.202–205 Therefore, the overall weight of current evidence at present suggests policosanol may not play a role in the treatment of hypercholesterolemia.
Chinese red yeast rice extract (RYRE) (Monascus purpureus)
The benefit of Chinese RYRE, a fungus, has been known for over a decade to have cholesterol-lowering effects.206–211 It contains a natural source of lovastatin, possessing statin properties, and many other substances such as flavonoids, polyunsaturated fats, pyrrolinic compounds.212 Like statin cholesterol-lowering agents, Chinese RYRE is an inhibitor of HMG-CoA reductase and can potentially have similar side-effects such as liver impairment and hepatitis with elevation of alanine-amino transferase (ALT) and aspartate-amino transferase (AST), and myopathy or rhabdomyolysis with elevation of creatinine kinase (CK).213, 214, 215 The biosynthesis of ubiquinone (CoQ10) is well recognised to be affected by the inhibition of HMG-CoA reductase with significant reduction in plasma levels with statin treatment. CoQ10 is essential for the production of energy, has antioxidative properties and reduced levels are thought to be responsible for membrane alteration and consequent cellular damage leading to myopathy. Anaphylaxis to the yeast extract is also reported in a case report.216
A number of short-term, placebo-controlled trials of Monascus purpureus Went rice (dosage 600mg daily for 8 weeks), demonstrated significant reduction in LDL-cholesterol levels, total cholesterol/HDL-lipoprotein cholesterol ratio, LDL-cholesterol/HDL-cholesterol ratio and apolipoprotein B/apolipoprotein A-I ratios in hypercholesterolemic patients (aged 23–65 years) when compared with placebo.217, 218 Monascus purpureus Went rice therapy was able to reduce LDL-cholesterol by up to 27.7%, total cholesterol by 21.5%, triglycerides by 15.8% and apolipoprotein B by 26.0% with 8 weeks therapy.218 There was a non-significant rise in HDL-cholesterol and apolipoprotein A-I levels by 0.9% and 3.4% respectively.
A longer trial of Monascus purpureus Went rice (600mg twice daily 1st month, then daily) for a total of 6–12 months in subjects with secondary nephrotic hyperlipidemia demonstrated it was equally as effective as fluvastatin (20mgs/day) in reducing cholesterol levels and well-tolerated with no significant side-effects, including myopathy.219 A recent meta-analysis of trials of Chinese RYRE for primary hyperlipidemia identified 93 randomised trials (9625 participants) of namely 3 RYRE preparations (Cholestin, Xuezhikang and Zhibituo), and found from the combined results significant reduction of serum total cholesterol levels, triglycerides levels and LDL-cholesterol levels, and increase of HDL-cholesterol levels compared with placebo and on par to statins such as pravastatin, simvastatin, lovastatin, atorvastatin, or fluvastatin.220 Another recent RCT involving 62 patients with dyslipidemia and history of discontinuation of statin therapy due to myalgias have demonstrated that those receiving 1800mg/day of RYRE for 24 weeks had a significant reduction in LDL-cholesterol of 0.9mmol/L without adverse effects on HDL-cholesterol, triglyceride, liver enzyme, CPK, weight loss, and pain severity scores.221 More long-term research is warranted.
Conclusion
Taken together, for maximum defence against the risk of developing cardiovascular disease the following targets have been set:17, 20
In summary, non-pharmaceutical management of hyperlipidemia should include a combination of lifestyle changes such as diet, exercise, stress management and consideration for co-supplementation such as with phytosterols, niacin, Chinese RYRE, and omega-3 fatty acids to optimise plasma lipid profile, particularly in people with mixed hyperlipidemia. Where stronger therapy is necessary, pharmaceutical medication may be warranted.
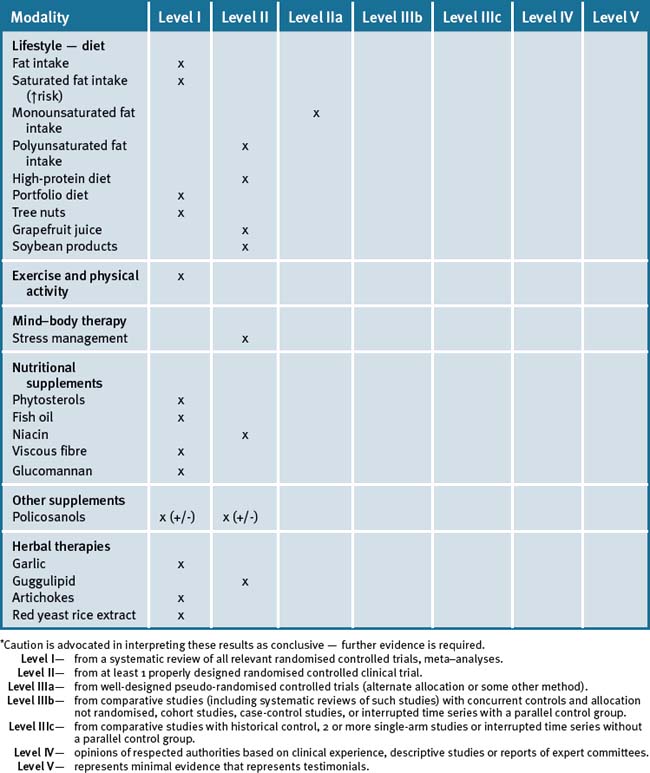
Table 18.3 summarises the level of scientific evidence for the treatment of hyperlipidemia for lifestyle factors and CAM (complementary and alternative medicine) therapies.
Clinical tips handout for patients — hyperlipidemia
1 Lifestyle advice
Sunshine
2 Physical activity/exercise
3 Mind–body medicine
5 Dietary changes
6 Supplements
Fish oils (EPA/DHA)
Vitamin B3 — niacin (nicotinic acid)
Guar gum
Glucomannan
Glucomannan is high in fibre, derived from Amorphophallus konjac.
Soybean products
Herbs
Artichoke (Cynara scolymus) leaf extract (ALE)
1 Kolovou G.D., Anagnostopoulou K.K., Cokkinos D.V. Pathophysiology of dyslipidaemia in the metabolic syndrome. Postgrad Med J. 2005;81:358-366.
2 Bernard J. Free fatty acid receptor family: novel targets for the treatment of diabetes and dyslipidemia. Curr Opin Investig Drugs. 2008;9:1078-1083.
3 Funatsu T., Suzuki K., Goto M., et al. Prolonged inhibition of cholesterol synthesis by atorvastatin inhibits apo B-100 and triglyceride secretion from HepG2 cells. Atherosclerosis. 2001;157:107-115.
4 Holvoet P., Jenny N.S., Schreiner P.J., et al. The relationship between oxidised LDL and other cardiovascular risk factors and subclinical CVD in different ethnic groups: The Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis. 2007;194:245-252.
5 Gordon T., Kannel W.B. Premature mortality from coronary heart disease. The Framingham study. JAMA. 1971;215:1617-1625.
6 Iso H., Jacobs D.R.J., Wentworth D., et al. Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the multiple risk factor intervention trial. N Engl J Med. 1989;320:904-910.
7 World Health Organization. Quantifying selected major risks to health. In: The World Health Report 2002-Reducing Risks, Promoting Healthy Life. Chapter 4. Geneva: World Health Organization; 2002. 47–97
8 Eaton C.B. Hyperlipidemia. Prim Care Clin Office Pract. 2005;32:1027-1055.
9 American Heart Association. High Blood Cholesterol and Other Lipids – Statistics (2009 Update). Available at: http://www.americanheart.org/downloadable/heart/1236205246237CHOL.pdf (accessed 18 June 2009).
10 Knox S.A., Harrison C.M., Britt H.C., et al. Estimating prevalence of common chronic morbidities in Australia. Medical Journal of Australia. 2008;189:66-70.
11 Li Z., Yang R., Xu G., et al. Serum lipid concentrations and prevalence of dyslipidemia in a large professional population in Beijing. Clinical Chemistry. 2005;51:144-150.
12 Rana JS, Visser ME, Arsenault BJ, et al. Metabolic dyslipidemia and risk of future coronary heart disease in apparently healthy men and women: The EPIC-Norfolk prospective population study. Int J Cardiol Epub ahead of print, doi:10.1016/j.ijcard.2009.03.123.
13 Ford E.S., Li C., Zhao G., Pearson W.S., et al. Hypertriglyceridemia and its pharmacologic treatment among US adults. Arch Intern Med. 2009;169:572-578.
14 Thom T., Haase N., Rosamond W., et al. Heart disease and stroke statistics – 2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85-e151.
15 Palmer A.J., Valentine W.J., Roze S., et al. Overview of costs of stroke from published, incidence-based studies spanning 16 industrialised countries. Curr Med Res Opin. 2005;21:19-26.
16 Erdman D.M., Cook C.B., Greenlund K.J., et al. The impact of outpatient diabetes management on serum lipids in urban African-Americans with type 2 diabetes. Diabetes Care. 2002;25:9-15.
17 National Heart Foundation of Australia and The Cardiac Society of Australia & New Zealand. Position Statement on Lipid Management – 2005. Heart and Lung Circulation. 2005;14:275-291. Online. Available: http://www.heartfoundation.org.au/SiteCollectionDocuments/Lipids%20HLC%20Pos%20Statement.pdf (accessed 18 June 2009)
18 Euroaspire. A European Society of Cardiology survey of secondary prevention of coronary heart disease. Euroaspire Study Group. European action on secondary prevention through intervention to reduce events. Principal results. Eur Heart J. 1997;18:1569-1582.
19 Simons L.A., Levis G., Simons J. Apparent discontinuation rates in patients prescribed lipid-lowering drugs. Med J Aust. 1996;164:208-211.
20 NCEP. Executive summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486-2497.
21 Nies L.K., Cymbala A.A., Kasten S.L., et al. Complementary and alternative therapies for the management of dyslipidemia. Ann Pharmacother. 2006;40:1984-1992.
22 Caron M.F., White C.M. Evaluation of the anti-hyperlipidemic properties of dietary supplements. Pharmacotherapy. 2001;21:451-457.
23 Beekman M., Heijmans B.T., Martin Nicholas G., et al. Evidence for a QTL on chromosome 19 influencing LDL-cholesterol levels in the general population. European Journal of Human Genetics. 2003;11:845-850.
24 Jensen H.K. The molecular genetic basis and diagnosis of familial hypercholesterolemia in Denmark. Dan Med Bull. 2002;49:318-345.
25 Rosenthal R.L. Effectiveness of altering serum cholesterol levels without drugs. BUMC Proceedings. 2000;13:351-355.
26 Clifton P. Lowering cholesterol: A review on the role of plant sterols. Australian Family Physician. 2009;38:218-221.
27 Collaborative Group S.E.A.R.C.H., Link E., Parish S., et al. SLCO1B1 variants and statin-induced myopathy – A genomewide study. N Engl J Med. 2008;359:789-799.
28 Dimsdale J.E., Herd J.A. Variability of plasma lipids in response to emotional arousal. Psychosomatic Medicine. 1982;44:413-430.
29 Brindley D.N., Rolland Y. Possible connections between stress, diabetes, hypertension and altered lipoprotein metabolism that mey result in athersclerosis. Clinical Science. 1989;77:453-461.
30 Fan A.Z., Strine T.W., Muppidi S.R., et al. Psychological distress associated with self-reported high blood pressure and high blood cholesterol in U.S. adults, 2007. Int J Public Health. 2009 April 14. Epub ahead of print
31 Masley S.C., Weaver W., Peri G., et al. Efficacy of lifestyle changes in modifying practical markers of wellness and ageing. Altern Ther Health Med. 2008;14:24-29.
32 Khatri D., Mathur K.C., Gahlot S., et al. Effects of yoga and meditation on clinical and biochemical parameters of metabolic syndrome. Diabetes Research and Clinical Practice, Epub ahead of print. 2008. doi:10.1016/j.diabres.2007.05.002
33 Lee I.M., Sesso H.D., Paffenbarger R.S.Jr. Physical activity and coronary heart disease risk in men: does the duration of exercise episodes predict risk? Circulation. 2000;102:981-986.
34 Halverstadt A., Phares D.A., Wilund K.R., et al. Endurance exercise training raises high-density lipoprotein cholesterol and lowers small low-density lipoprotein and very low-density lipoprotein independent of body fat phenotypes in older men and women. Metabolism Clinical and Experimental. 2007;56:444-450.
35 Vislocky L.M., Pikosky M.A., Rubin K.H., et al. Habitual consumption of eggs does not alter the beneficial effects of endurance training on plasma lipids and lipoprotein metabolism in untrained men and women. Journal of Nutritional Biochemistry. 2009;20:26-34.
36 Grandjean P.W., Crouse S.F., O’Brian B.C., et al. The effects of menopausal status and exercise training on serum lipids and the activities of intravascular enzymes related to lipid transport. Metabolism. 1998;47:377-383.
37 Kokkinos P.F., Holland J.C., Narayan P., et al. Miles run per week and high-density lipoprotein cholesterol levels in healthy, middleaged men. Arch Intern Med. 1995;155:415-420.
38 Kokkinos P.F., Narayan P., Colleran J. Effects of moderate intensity exercise on serum lipids in African-American men with sever systemic hypertension. Am J Cardiol. 1998;81:732-735.
39 Seip R.L., Moulin P., Cocke T., et al. Exercise training decreases plasma cholesteryl ester transfer protein. Arterioscler Thromb. 1993;13:1359-1367.
40 Thompson P.D., Yurgalevitch S.M., Flynn M.M., et al. Effect of prolonged exercise training without weight loss on high-density lipoprotein metabolism in overweight men. Metabolism. 1997;46:217-223.
41 Wilson P.W., D’Agostino R.B., Levy D., et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837-1847.
42 Ullrich I.H., Reid C.M., Yeater R.A., et al. Increased HDL-cholesterol levels with a weight lifting program. South Med J. 1987;80:328-331.
43 Boyden T.W., Pamenter R.W., Going S.B., et al. Resistance exercise training is associated with decreases in serum low-density lipoprotein cholesterol levels in premenopausal women. Arch Intern Med. 1993;153:97-100.
44 Kokkinos P.F., Hurley B.F., Smutok M.A., et al. Strength training does not improve lipoprotein-lipid profiles in men at risk for CHD. Med Sci Sports Exerc. 1993;32:1134-1139.
45 Smutok M.A., Reece C., Kokkinos P.F., et al. Aerobic versus strength training for risk factor intervention in middle-aged men at high risk for coronary artery disease. Metabolism. 1993;42:177-184.
46 Durstine J.L., Grandjean P.W., Cox C.A., et al. Lipids, Lipoproteins, and Exercise. Journal of Cardiopulmonary Rehabilitation. 2002;22:385-398.
47 Marques E, Carvalho J, Soares JMC, et al. Effects of resistance and multi-component exercise on lipid profiles of older women. Maturitas Epub ahead of print, doi:10.1016/j.maturitas.2009.03.003.
48 Monda K.L., Ballantyne C.M., North K.E. Longitudinal impact of physical activity on lipid profiles in middle-aged adults: the Atherosclerosis Risk in Communities (ARIC) Study. J Lipid Res. 2009. Epub ahead of print, doi:10.1194/jlr.P900029-JLR200
49 Keys A. Coronary heart disease in seven countries. Circulation. 1970;41(Suppl. 1):1-211.
50 Skekelle R.B., Shryock A.M., Paul O., et al. Diet, serum cholesterol, and death from coronary heart disease: the Western Electric study. New England Journal of Medicine. 1981;304:65-70.
51 Joossens J.V., Vuylsteek K., Brems-Heyns E., et al. The pattern of food and mortality in Belgium. Lancet. 1977;1:1069-1072.
52 Kato H., Tillotson J., Nichaman M.Z., et al. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: serum lipids and diet. American Journal of Epidemiology. 1993;97:372-385.
53 Keys A., Anderson J.T., Grande F. Prediction of serum-cholesterol responses of man to changes in fats in the diet. Lancet. 1957;2:959-966.
54 Hegsted D.M., McGandy R.B., Myers M.L., et al. Quantitative effects of dietary fat on serum cholesterol in man. American Journal of Clinical Nutrition. 1965;17:281-295.
55 Ahrens E.H., Insull W., Blomstrand R., et al. The influence of dietary fats on serum-lipid levels in man. Lancet. 1957;1:943-953.
56 Shepherd J., Packard C.J., Grundy S.M., et al. Effects of saturated and polyunsaturated fat diets on the chemical composition and metabolism of low density lipoproteins in man. Journal of Lipid Research. 1980;21:91-99.
57 Turner J.D., Le N.A., Brown W.V. Effect of changing dietary fat saturation on low density lipoprotein metabolism in man. American Journal of Physiology. 1981;241:E57-E63.
58 Hunninghake D.B., Stein E.A., Dujovne C.A., et al. The efficacy of intensive dietary therapy alone or combined with lovastatin in outpatients with hypercholesterolemia. N Engl J Med. 1993;328:1213-1219.
59 Schaefer E.J., Brosseau M.E. Diet, lipoproteins, and coronary heart disease. Endocrinol Metab Clin North Am. 1998;27:711-727.
60 Ornish D., Brown S.E., Scherwitz L.W., et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet. 1990;336:129-133.
61 Grundy S.M. What is the desirable ratio of saturated, polyunsaturated, and monounsaturated fatty acids in the diet? Am J Clin Nutr. 1997;66(Suppl):988S-990S.
62 Knopp R.H. Drug treatment of lipid disorders. N Engl J Med. 1999;341:498-511.
63 Mensink R.P., Zock P.L., Kester A.D.M., et al. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL-cholesterol and on serum lipids and lipoproteins: a meta-analysis of 60 controlled trials. Amer J Clin Nutr. 2003;77:1146-1155.
64 Rask-Nissilä L., Jokinen E., Terho P., et al. Neurological development of 5-year-old children receiving a low-saturated fat, low-cholesterol diet since infancy: A randomised controlled trial. Journal of the American Medical Association. 2000;284:993-1000.
65 Keys A. Serum cholesterol response to dietary cholesterol. Amer J Clin Nutr. 1984;40:351-359.
66 Grundy S.M., Florentin L., Nixand D., et al. Comparison of monounsaturated fatty acids and carbohydrates for reducing raised levels of plasma cholesterol in man. Am J Clin Nutr. 1988;47:965-969.
67 Keys A., Anderson J.T., Grande F. Serum cholesterol response to changes in the diet, IV: particular saturated fatty acids in the diet. Metabolism. 1965;14:776-787.
68 Nygard O., Nordrehaug J.E., Refsum H., et al. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 1997;337:230-236.
69 Gaziano J.M., Buring J.E., Breslow J.L., et al. Moderate alcohol intake, increased levels of high density lipoprotein and its subfractions, and decreased risk of myocardial infarction. N Engl J Med. 1993;329:1829-1834.
70 Trichopoulou A., Vasilopoulou E., Liagiou A. Mediterranean diet and coronary heart disease: are antioxidants critical? Nutr Rev. 1999;57:253-255.
71 de Lorgeril M., Renaud S., Mamelle N., et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343:1454-1459.
72 de Lorgeril M., Salen P., Martin J.-L., et al. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99:779-785.
73 Denke M.A. Dietary fats, fatty acids, and their effects on lipoproteins. Curr Atheroscler Rep. 2006;8:466-471.
74 Fernandez M.L., West K.L. Mechanisms by which dietary fatty acids modulate plasma lipids. J Nutr. 2005;135:2075-2078.
75 Lecerf J.M. Fatty acids and cardiovascular disease. Nutr Rev. 2009;67:273-283.
76 Jakobsen M.U., O’Reilly E.J., Heitmann B.L., et al. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr. 2009;89:1425-1432.
77 Mensink R.P., Zock P.L., Kester A.D.M., et al. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL-cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146-1155.
78 Stampfer M.J., Sacks F.M., Salvini S., et al. A prospective study of cholesterol, apolipoproteins, and the risk of myocardial infarction. N Engl J Med. 1991;325:373-381.
79 Mukuddem-Petersen J., Oosthuisen W., Jerling J. A systematic review of the effects of nuts on blood lipid profiles in humans. J Nutr. 2005;135:2082-2089.
80 Griel A.E., Kris-Etherton P.M. Tree nuts and the lipid profile: a review of clinical studies. Br J Nutr. 2006;96(Suppl 2):S68-S78.
81 Ros E. Nuts and novel biomarkers of cardiovascular disease. Am J Clin Nutr. 2009;89(suppl):1649S-1656S.
82 Rajaram S., Haddad E.H., Mejia A., et al. Walnuts and fatty fish influence different serum lipid fractions in normal to mildly hyperlipidemic individuals: a randomised controlled study. Am J Clin Nutr. 2009;89(suppl):1657S-1663S.
83 Samaha F.F., Iqbal N., Seshadri P., et al. A low-carbohydrate as compared with a low-fat diet in severe obesity. N Engl J Med. 2003;348:2074-2081.
84 Foster G.D., Wyatt H.R., Hill J.O., et al. A randomised trial of a low-carbohydrate diet for obesity. N Engl J Med. 2003;348:2082-2090.
85 Skov A.R., Toubro S., Rønn B., et al. Randomised trial on protein vs carbohydrate in ad libitum fat reduced diet for the treatment of obesity. Int J Obes Relat Metab Disord. 2003;23:528-536.
86 Jenkins D.J., Kendall C.W.C., Vidgen E., et al. High-protein diets in hyperlipidemia: effect of wheat gluten on serum lipids, uric acid, and renal function. Am J Clin Nutr. 2001;74:57-63.
87 Parker B., Noakes M., Luscombe N., et al. Effect of a high-protein, high-monounsaturated fat weight loss diet on glycemic control and lipid levels in type 2 diabetes. Diabetes Care. 2002;25:425-430.
88 Bravata D.M., Sanders L., Huang J., et al. Efficacy and safety of low-carbohydrate diets: a systematic review. JAMA. 2003;289:1837-1850.
89 Jenkins D.J.A., Julia M.W., Wong R.D., et al. The Effect of a Plant-Based Low-Carbohydrate (‘Eco-Atkins’) Diet on Body Weight and Blood Lipid Concentrations in Hyperlipidemic Subjects. Arch Intern Med. 2009;169(11):1046-1054.
90 Jenkins D.J., Kendall C.W.C., Marchie A., et al. Effects of a dietary portfolio of cholesterol-lowering foods vs lovastatin on serum lipids and C-reactive protein. JAMA. 2003;290:502-510.
91 Jenkins D.J.A., Kendall C.W.C., Faulkner D.A., et al. The Effect of Combining Plant Sterols, Soy Protein, Viscous Fibres, and Almonds in Treating Hypercholesterolemia. Metabolism. 2003;52:1478-1483.
92 Jenkins D.J., Kendall C.W., Faulkner D.A., et al. Assessment of the longer-term effects of a dietary portfolio of cholesterol-lowering foods in hypercholesterolemia. Am J Clin Nutr. 2006;83:582-591.
93 Jenkins D.J.A., Kendall C.W.C., Faulkner D.A., et al. Long-term effects of a plant-based dietary portfolio of cholesterol-lowering foods on blood pressure. European Journal of Clinical Nutrition. 2008;62:781-788.
94 Jenkins D.J., Kendall C.W., Marchie A., et al. Direct comparison of dietary portfolio vs statin on C-reactive protein. European Journal of Clinical Nutrition. 2005;59:851-860.
95 Gigleux I., Jenkins D.J.A., Kendall C.W.C., et al. Comparison of a dietary portfolio diet of cholesterol-lowering foods and a statin on LDL particle size phenotype in hypercholesterolaemic participants. British Journal of Nutrition. 2007;98:1229-1236.
96 Gorinstein S., Caspi A., Libman I., et al. Fresh israeli jaffa sweetie juice consumption improves lipid metabolism and increases antioxidant capacity in hypercholesterolemic patients suffering from coronary artery disease: studies in vitro and in humans and positive changes in albumin and fibrinogen fractions. J Agric Food Chem. 2004;52:5215-5222.
97 Gorinstein S., Caspi A., Libman I., et al. Red grapefruit positively influences serum triglyceride level in patients suffering from coronary atherosclerosis: studies in vitro and in humans. J Agric Food Chem. 2006;54:1887-1892.
98 Dahan A., Altman H. Food-drug interaction: grapefruit juice augments drug bioavailability–mechanism, extent and relevance. Eur J Clin Nutr. 2004;58:1-9.
99 Gateway I.M., Braun L. Drug-Food Supplement Interactions. Journal of Complementary Medicine. 2004;3:80-84.
100 Anderson J.W., Johnstone B.M., Cook-Newell M.E. Meta-analysis of the effects of soy protein intake on serum lipids. New Engl J Med. 1995;333:276-282.
101 Sirtori C.R., Eberini I., Arnoldi A. Hypocholesterolaemic effects of soya proteins: results of recent studies are predictable from the Anderson meta-analysis data. Br J Nutr. 2007;97:816-822.
102 Descovich G.C., Ceredi C., Gaddi A., et al. Multicentre study of soybean protein diet for outpatient hyper-cholesterolaemic patients. Lancet. 1980;ii:709-712.
103 Zhan S., Ho S.C. Meta-analysis of the effects of soy protein containing isoflavones on the lipid profile. Am J Clin Nutr. 2005;81:397-408.
104 Dewell A., Hollenbeck P.L.W., Hollenbeck C.B. A critical evaluation of the role of soy protein and isoflavone supplementation in the control of plasma cholesterol concentrations. Journal of Clinical Endocrinology & Metabolism. 2006;91:772-780.
105 Science Advisory A.H.A. Soy protein and cardiovascular disease: a statement for health care professionals from the Nutrition Committee of the AHA. Circulation. 2000;102:2555-2559.
106 Brufau G., Canela M.A., Rafecas M. Phytosterols: physiologic and metabolic aspects related to cholesterol-lowering properties. Nutr Res. 2008;28:217-225.
107 Tikkanen M.J. Plant sterols and stanols. Handb Exp Pharmacol. 2005;170:215-230.
108 Ikeda I., Tanabe Y., Sugano M. Effects of sitosterol and sitostanol on micellar solubility of cholesterol. J Nutr Sci Vitaminol. 1989;35:361-369.
109 Subbiah M.T., Kottke B.A., Carlo I.A. Uptake of campesterol in pigeon intestine. Biochim Biophys Acta. 1971;249:643-646.
110 Ling W.H., Jones P.J. Dietary phytosterols: a review of metabolism, benefits and side-effects. Life Sci. 1995;57:195-206.
111 Plat J., Mensink R.P. Increased intestinal ABCA1 expression contributes to the decrease in cholesterol absorption after plant stanol consumption. FASEB J. 2002;16:1248-1253.
112 Gylling H., Miettinen T.A. Effects of inhibiting cholesterol absorption and synthesis on cholesterol and lipoprotein metabolism in hypercholesterolemic non-insulin dependent diabetic men. J Lipid Res. 1996;37:1776-1785.
113 Lesesne J.M., Castor C.W., Hoobler S.W. Prolonged reduction in human blood cholesterol levels induced by plant sterols. Med Bull. 1955;21:13-17.
114 Ostlund R.E.Jr. Phytosterols in human nutrition. Annu Rev Nutr. 2002;22:533-549.
115 Clifton P. Lowering cholesterol: A review on the role of plant sterols. Australian Family Physician. 2009;38:218-221.
116 Law M. Plant sterol and stanol margarines and health. BMJ. 2000;320:861-864.
117 Neil H.A.W., Huxley R.R.. Efficacy and therapeutic potential of plant sterols. Atheroscler. 2002;Suppl 3:11-15..
118 Lichtenstein A.H. Plant sterols and blood lipid levels. Curr Opin Clin Nutr Metab Care. 2002;5:147-152.
119 Simons L.A. Additive effect of plant sterol-ester margarine and cerivastatin in lowering low-density lipoprotein cholesterol in primary hypercholesterolemia. Am J Cardiol. 2002;90:737-740.
120 Micallef M.A., Garg M.L. The Lipid-Lowering Effects of Phytosterols and (n-3) Polyunsaturated Fatty Acids Are Synergistic and Complementary in Hyperlipidemic Men and Women. J Nutr. 2008;138:1086-1090.
121 Khandelwal S., Demonty S., Jeemon P. Independent and interactive effects of plant sterols and fish oil n-3 long-chain polyunsaturated fatty acids on the plasma lipid profile of mildly hyperlipidaemic Indian adults. British Journal of Nutrition. 2009. EPub ahead of print doi:10.1017/S0007114509297170
122 AbuMweis S.S., Jones P.J. Cholesterol-lowering effect of plant sterols. Curr Atheroscler Rep. 2008;10:467-472.
123 Plana N., Nicolle C., Ferre R., et al. Plant sterol-enriched fermented milk enhances the attainment of LDL-cholesterol goal in hypercholesterolemic subjects. Eur J Nutr. 2008;47:32-39.
124 Moruisi K.G., Oosthuisen W., Opperman A.M. Phytosterols/stanols lower cholesterol concentrations in familial hypercholesterolemic subjects: a systematic review with meta-analysis. J Am Coll Nutr. 2006;25:41-48.
125 O’Connor P.J., Quiter E.S., Rush W.A., et al. Relative effectiveness of niacin and lovastatin for treatment of dyslipidemias in a health maintenance organisation. J Family Pract. 1997;44:462-467.
126 Illingworth D., Stein E.A., Mitchel Y.B., et al. Comparative effects of lovastatin and niacin in primary hypercholesterolemia: a prospective trial. Arch Intern Med. 1994;154:1586-1595.
127 Vega G., Grundy S. Lipoprotein responses to treatment with lovastatin, gemfibrozil and nicotinic acid in normolipidemic patients with hypoalphalipoprotein. Arch Intern Med. 1994;154:73-82.
128 Guyton J.R., Blazing M.A., Hagar J., et al. Extended-release niacin vs gemfibrozil for the treatment of low levels of high-density lipoprotein cholesterol. Niaspan-Gemfibrozil Study Group. Arch Intern Med. 2000;160:1177-1184.
129 Linke A., Sonnabend M., Fasshauer M., et al. Effects of extended-release niacin on lipid profile and adipocyte biology in patients with impaired glucose tolerance. Atherosclerosis. 2009. Epub prior to print, doi:10.1016/j.atherosclerosis.2008.11.026
130 Wolfe M.L., Vartanian S.F., Ross J.L., et al. Safety and effectiveness of Niaspan when added sequentially to a statin for treatment of dyslipidemia. Am J Cardiol. 2001;87:476-479.
131 Wink J., Giacoppe G., King J. Effect of very-low-dose naicin on high-density lipoprotein in patients undergoing long-term statin therapy. Am Heart J. 2002;143:514-518.
132 Brown B.G., Zhao X.Q., Chait A. Simvastatin and niacin, antioxidant vitamins, or the combination for the prevention of coronary disease. N Engl J Med. 2001;345:1583-1593.
133 Kamanna V.S., Kashyap M.L. Nicotinic acid (niacin) receptor agonists: will they be useful therapeutic agents? Am J Cardiol. 2007;100:S53-S61.
134 Digby J.E., Lee J.M., Choudhury R.P. Nicotinic acid and the prevention of coronary artery disease. Curr Opin Lipidol. 2009. Epub ahead of print doi: 10.1097/MOL.0b013e32832d3b9d
135 Robinson J.G. Management of complex lipid abnormalities with a fixed dose combination of simvastatin and extended release niacin. Vasc Health Risk Manag. 2009;5:31-43.
136 Karas R.H., Kashyap M.L., Knopp R.H. Long-term safety and efficacy of a combination of niacin extended release and simvastatin in patients with dyslipidemia: the OCEANS study. Am J Cardiovasc Drugs. 2008;8:69-81.
137 Plaisance E.P., Mestek L., Mahurin A.J., et al. Postprandial triglyceride responses to aerobic exercise and extended-release niacin. American Journal of Clinical Nutrition. 2008;88:30-37.
138 Kamanna V.S., Ganji S.H., Kashyap M.L. Niacin: an old drug rejuvenated. Curr Atheroscler Rep. 2009;11:45-51.
139 Kamanna V.S., Vo A., Kashyap M.L. Nicotinic acid: recent developments. Curr Opin Cardiol. 2008;23:393-398.
140 Kamanna V.S., Kashyap M.L. Nicotinic acid (niacin) receptor agonists: will they be useful therapeutic agents? Am J Cardiol. 2007;100:S53-S61.
141 Theuwissen E., Mensink R.P. Water-soluble dietary fibres and cardiovascular disease. Physiology & Behavior. 2008;94:285-292.
142 Braaten J.T., Wood P.J., Scott F.W., et al. Oat beta-glucan reduces blood cholesterol concentration in hypercholesterolemic subjects. Eur J Clin Nutr. 1994;48:465-474.
143 Anderson J.W. Dietary fibre, complex carbohydrate and coronary artery disease. Can J Cardiol. 1995;11(Suppl G):55G-62G.
144 Swain J., Rouse I., Curley C., et al. Comparison of the effects of oat bran and low-fibre wheat on serum lipoprotein levels and blood pressure. N Engl J Med. 1990;322:147-152.
145 Leadbetter J., Ball M.J., Mann J.I. Effects of increasing quantities of oat bran in hypercholesterolemic people. Am J Clin Nutr. 1991;54:841-845.
146 Lovegrove J.A., Clohessy A., Milon H., et al. Modest doses of betaglucan do not reduce concentrations of potentially atherogenic lipoproteins. Am J Clin Nutr. 2000;72:49-55.
147 Ripsin C.M., Keenan J.M., Jacobs D.R., et al. Oat products and llipid-lowering. A meta-analysis. JAMA. 1992;267:3317-3325.
148 Glore S.R., Van Treeck D., Knehans A.W., et al. Soluble fibre and serum lipids: a literature review. J Am Diet Assoc. 1994;94:425-436.
149 Brown L., Rosner B., Willett W.W., et al. Cholesterol-lowering effects of dietary fibre: a meta-analysis. Am J Clin Nutr. 1999;69:30-42.
150 Talati R., Baker W.L., Pabilonia M.S., et al. The Effects of Barley-Derived Soluble Fibre on Serum Lipids. Ann Fam Med. 2009;7:157-163.
151 Sprecher D.L., Harris B.V., Goldberg A.C., et al. Efficacy of psyllium in reducing serum cholesterol levels in hypercholesterolemic patients on high- or low-fat diets. Ann Intern Med. 1993;199:545-554.
152 Anderson J.W., Zettwoch N., Feldman T., et al. Cholesterol-lowering effects of psyllium hydrophilic mucciloid for hypercholesterolemic men. Arch Intern Med. 1988;148:292-296.
153 Olson B.H., Anderson S.M., Becker M.P., et al. Psyllium-enriched cereals lower blood total cholesterol & LDL-cholesterol, but not HDL-cholesterol in hypercholesterolemic adults: results of a metanalysis. J Nutr. 1992;127:1973-1980.
154 Anderson J.W., Riddell-Mason S., Gustafson N.J., et al. Cholesterol-lowering effects of psyllium enriched cereal as an adjunct to a prudent diet in the treatment of mild to moderate hypercholesterolemia. Am J Clin Nutr. 1992;56:93-95.
155 Keys A., Grande F., Anderson J.T. Fibre and pectin in the diet and serum cholesterol concentration in man. Proc Soc Exp Biol Med. 1961;106:555-558.
156 Schwab U., Louheranta A., Torronen A., et al. Impact of sugar beet pectin and polydextrose on fasting and postprandial glycemia and fasting concentrations of serum total and lipoprotein lipids in middle-aged subjects with abnormal glucose metabolism. Eur J Clin Nutr. 2006;60:1073-1080.
157 Mahalko J.R., Sandstead H.H., Johnson L.K., et al. Effect of consuming fibre from corn bran, soy hulls, or apple powder on glucose tolerance and plasma lipids in type II diabetes. Am J Clin Nutr. 1984;39:25-34.
158 Fahrenbach M.J., Riccardi B.A., Saunders J.C., et al. Comparative effetcs of guar gum and pectin on human serum cholesterol levels. Circulation. 1965;55:767-772.
159 Martino F., Martino E., Morrone F., et al. Effect of dietary supplementation with glucomannan on plasma total cholesterol and low density lipoprotein cholesterol in hypercholesterolemic children. Nutr Metab Cardiovasc Dis. 2005;15:174-180.
160 Arvill A., Bodin L. Effect of short-term ingestion of konjac glucomannan on serum cholesterol in healthy men. Am J Clin Nutr. 1995;61:585-589.
161 Zhang M.O., Huang C.Y., Wang X., et al. The effect of foods containing refined konjac meal on human lipid metabolism. Biomed Environ Sci. 1990;3:99-105.
162 Chen H.L., Huey-Herng Sheu W., Tai T.S., et al. Konjac supplement alleviated hypercholesterolemia and hyperglycemia in type 2 diabetic subjects—a randomised double-blind trial. J Am Coll Nutr. 2003;22:36-42.
163 Sood N., Baker W.L., Coleman C.I.. Effect of glucomannan on plasma lipid and glucose concentrations, body weight, and blood pressure: systematic review and meta-analysis. Am J Clin Nutr. 2008;88:1167-1175..
164 Weintraub M.S., Zechner R., Brown A., et al. Dietary polyunsaturated fats of the w-6 and w-3 series reduce postprandial lipoprotein levels: chronic and acute effects of fat saturation on postprandial lipoprotein metabolism. J Clin Invest. 1988;82:1884-1893.
165 Woodman R.J., Mori T.A., Burke V., et al. Effects of purified eicosapentaenoic and docosahexaenoic acids on glycemic control, blood pressure, and serum lipids in type 2 diabetic patients with treated hypertension. Am J Clin Nutr. 2002;76:1007-1015.
166 Grimsgaard S., Bonaa K.H., Hansen J.B., et al. Highly purified eicosapentaenoic acid and docosahexaenoic acid in humans have similar triacylglycerol-lowering effects but divergent effects on serum fatty acids. Am J Clin Nutr. 1997;66:649-659.
167 Connor W.E. Dietary sterols: their relationship to atherosclerosis. J Am Diet Assoc. 1968;52:202-208.
168 Eslick G.D., Howe P.R.C., Smith C., et al. Benefits of fish oil supplementation in hyperlipidemia: a systematic review and meta-analysis. Int J Cardiol. 2009. doi:10.1016/j.ijcard.2008.03.092
169 Studer M., Briel M., Leimenstoll B., et al. Effects of different antilipidemic agents and diet on mortality. Arch Intern Med. 2005;165:725-730.
170 GISSI-HF investigators. Effect of n-3 polyunsaturated fatty acids in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372:1223-1230.
171 Nambi V., Ballantyne C.M. Combination therapy with statins and omega-3 fatty acids. Amer J Cardiol. 98, 2006. 43i–38i
172 Agarwal R.C., Singh S.P., Saran R.K., et al. Clinical trial of Guggulipid new hypolipidemic agent of plant prigin in primary Hyperlipidemia. Indian J Med Res. 1986;84:626-634.
173 Nityanand S., Srivastava J.S., Asthana O.P. Clinical trials with Guggulipid – A new hyperlipidemic agent. J Assoc Phys India. 1989;37:323-328.
174 Singh R.B., Niaz M.A., Ghosh S. Hypolipidemic and antioxidant effects of Commiphora mukul as an adjunct to dietary therapy in patients with hypercholesterolemia. Cardiovasc Drug Ther. 1994;8:659-664.
175 Szapary P.O., Wolfe M.L., Bloedon L.T., et al. Guggulipid for the treatment of Hypercholesterolemia: A randomised controlled trial. JAMA. 2003;290:765-772.
176 Nohr L.A., Rasmussen L.B., Straand J. Resin from the mukul myrrh tree, guggul, can it be used for treating hypercholesterolemia? A randomised, controlled study. Complement Ther Med. 2009;17:16-22.
177 Kraft K. Artichoke leaf extract: recent findings reflecting effects on lipid metabolism, liver and gastrointestinal tracts. Phytomedicine. 1997;4:369-378.
178 Bundy R., Walker R.F., Middleton R.W., et al. Artichoke leaf extract (Cynara scolymus) reduces plasma cholesterol in otherwise healthy hypercholesterolemic adults: A randomised, double-blind placebo-controlled trial. Phytomedicine. 2008;15:668-675.
179 Nazni P., Vijayakumar T.P., Alagianambi P., et al. Hypoglycemic and hypolipidemic effect of cynara scolymus among selected type 2 diabetic individuals. Pakistan J Nutrition. 2006;5:147-151.
180 Pittler M.H., Ernst E. Artichoke leaf extract for treating hypercholesterolaemia. Cochrane Database of Systematic Reviews. 2002. Art. No.: CD003335. doi: 10.1002/14651858.CD003335
181 Englisch W., Beckers C., Unkauf M., et al. Efficacy of artichoke dry extract in patients with hyperlipoproteinemia. Arzneim.-Forsch./Drug Res. 2000;50:260-265.
182 Petrowicz O., Gebhardt R., Donner M., et al. Effects of artichoke leaf extract (ALE) on lipoprotein metabolism in vitro and in vivo. Atherosclerosis. 1997;129:147.
183 Jain A., Vargas R., Gotzkowsky S., et al. Can garlic reduce the levels of serum lipids? A controlled clinical study. Am J Med. 1993;94:632-635.
184 Alder A.J., Holub B.J. Effect of garlic and oil supplementation on serum lipid and lipoprotein concentrations in hypercholesterolemic men. Am J Cli Nutr. 1997;65:445-450.
185 Steiner M., Khan A.H., Holbert D., et al. A double-blind crossover study in moderately hypercholesterolemic men that compared the effect of aged garlic extract and placebo administration on blood lipids. Am J Clin Nutr. 1996;64:866-870.
186 Byrne D.J., Neil H.A., Vallance D.T., et al. A pilot study of garlic consumption shows no significant effect on markers of oxidation or sub-fraction composition of low-density lipoprotein including lipoprotein (a) after allowance for non-compliance and the placebo effect. Clin Chim Acta. 1999;285:21-33.
187 Berthold H.K., Sudhop T., Von Bergman K. Effect of garlic oil preparation on serum lipoproteins and cholesterol metabolism: A randomised controlled trial. JAMA. 1998;279:1900-1902.
188 Warshafsky S., Kamer R.S., Sivak S.L. Effect of garlic on total serum cholesterol. A meta-analysis. Ann Intern Med. 1993;119:599-605.
189 Stevinson C., Pittler M.H., Ernst E. Garlic for treating hypercholesterolemia. A meta-analysis of randomised clinical trials. Ann Intern Med. 2001;135:65-66.
190 Khoo Y.S.K., Azis Z. Garlic supplementation and serum cholesterol: a meta-analysis. J Clin Pharm Ther. 2009;34:133-145.
191 Castano G., Mas R., Arruzazabala M.L., et al. Effects of Policosanol and Pravastatin on lipid profile, platelet aggregation and endothelaemia in older hypercholesterolemic patients. Int. J. Clin. Pharm. Res. 1999;XIX(4):105-116.
192 Castano G., Cannetti M., Moreira M., et al. Efficacy and tolerability of policosanol compared with lovastatin in patients with type II hypercholesterolemia and concomitant coronary risk factors. Current Therapeutic Research. 2000;61:137-146.
193 Fernandez J.C., Mas R., Castano G., et al. Comparison of the efficacy, safety and tolerability of policosanol versus fluvastatin in elderly hypercholesterolaemic women. Clinical Drug Invest. 2001;21:103-113.
194 Marcello S., Gladstein J., Tesone P., et al. Effects of bezafibrate plus policosanol or placebo in patients with combined dyslipidaemia: a pilot study. Current Therapeutic Research. 2000;61:346-357.
195 Nikitin I., Slepchenko N.V., Gratsianski N.A., et al. Results of the multicentre controlled study of the hypolipidemic drug polycosanol in Russia. Ter Arkh. 2000;72:7-10.
196 Prat H., Roman O., Pino E. Comparative effects of polycosanol and two HMG-CoA reductase inhibitors on type II hypercholesterolemia. Rev Med Chil. 1999;127:286-294.
197 Francini-Pesenti F., Beltramolli D., Dall’acqua S., et al. Effect of sugar cane policosanol on lipid profile in primary hypercholesterolemia. Phytother Res. 2008;22:318-322.
198 Berthold H.K., Unverdorben S., Degenhardt R., et al. Effect of policosanol on lipid levels among patients with hypercholesterolemia or combined hyperlipidemia: a randomised controlled trial. JAMA. 2006;295:2262-2269.
199 Cubeddu L.X., Cubeddu R.J., Heimowitz T., et al. Comparative lipid-lowering effects of policosanol and atorvastatin: a randomised, parallel, double-blind, placebo-controlled trial. Am Heart J. 2006;152:982-985.
200 Keller S., Gimmler F., Jahreis G. Octacosanol administration to humans decreases neutral sterol and bile acid concentration in feces. Lipids. 2008;43:109-115.
201 Chen J.T., Wesley R., Shamburek R.D., et al. Meta-analysis of natural therapies for hyperlipidemia: plant sterols and stanols versus policosanol. Pharmacotherapy. 2005;25:171-183.
202 Kassis A.N., Jones P.J. Changes in cholesterol kinetics following sugar cane policosanol supplementation: a randomised control trial. Lipids Health Dis. 2008;7:17.
203 Kassis A.N., Jones P.J. Lack of cholesterol-lowering efficacy of Cuban sugar cane policosanols in hypercholesterolemic persons. Am J Clin Nutr. 2006;84:1003-1008.
204 Kassis A.N., Kubow S., Jones P.J. Sugar cane policosanols do not reduce LDL oxidation in hypercholesterolemic individuals. Lipids. 2009;44:391-396.
205 Greyling A., De Witt C., Oosthuisen W., et al. Effects of a policosanol supplement on serum lipid concentrations in hypercholesterolaemic and heterozygous familial hypercholesterolaemic subjects. Br J Nutr. 2006;95:968-975.
206 Heber D., Yip I., Ashley J.M., et al. Cholesterol-lowering effects of a proprietary Chinese red-yeast-rice dietary supplement. Am J Clin Nutr. 1999;69:231-236.
207 Wang J., Lu A., Chi J. Multicenter clinical trial of the serum lipid-lowering effects of a monascus purpureus (red yeast) rice preparation from traditional Chinese medicine. Cur Ther Res. 1997;58:964-978.
208 Kou W., Lu Z., Guo J. Effect of xuezhikang on the treatment of primary hyperlipidemia. [Article in Chinese]. Chung Hua Nei Ko Tsa Chih. 1997;36:529-531.
209 Blisnakov E.G. More on the Chinese red-yeast-rice supplement and its cholesterol-lowering effect. Am J Clin Nutr. 2000;71:152-157.
210 Heber D., Lembertas A., Lu Q.Y., et al. An analysis of nine proprietary Chinese red yeast rice dietary supplements: implications of variability in chemical profile and contents. J Altern Complement Med. 2001;7:133-139.
211 Keithley J.K., Swanson B., Sha B.E., et al. A pilot study of the safety and efficacy of cholestin in treating HIV-related dyslipidemia. Nutrition. 2002;18:201-204.
212 Bianchi A. Extracts of Monascusus purpureus beyond statins–profile of efficacy and safety of the use of extracts of Monascus purpureus. Chin J Integr Med. 2005;11:309-313.
213 Prasad G.V., Wong T., Meliton G., et al. Rhabdomyolysis due to red yeast rice (Monascus purpureus) in a renal transplant recipient. Transplantation. 2002;74:1200-1201.
214 Mueller P.S. Symptomatic myopathy due to red yeast rice. Ann Intern Med. 2006;145:474-475.
215 Roselle H., Ekatan A., Tzeng J., et al. Symptomatic hepatitis associated with the use of herbal red yeast rice. Ann Intern Med. 2008;149:516-517.
216 Wigger-Alberti W., Bauer A., Hipler U.C., et al. Anaphylaxis due to Monascus purpureus-fermented rice (red yeast rice). Allergy. 1999;54:1330-1331.
217 Huang C.F., Li T.C., Lin C.C., et al. Efficacy of Monascus purpureus Went rice on lowering lipid ratios in hypercholesterolemic patients. Eur J Cardiovasc Prev Rehabil. 2007;14:438-440.
218 Lin C.C., Li T.C., Lai M.M. Efficacy and safety of Monascus purpureus Went rice in subjects with hyperlipidemia. Eur J Endocrinol. 2005;153:679-686.
219 Gheith O., Sheashaa H., Abdelsalam M., et al. Efficacy and safety of Monascus purpureus Went rice in subjects with secondary hyperlipidemia. Clin Exp Nephrol. 2008;12:189-194.
220 Liu J., Zhang J., Shi Y., et al. Chinese red yeast rice (Monascus purpureus) for primary hyperlipidemia: a meta-analysis of randomised controlled trials. Chin Med. 2006;1:4.
221 Becker D.J., Gordon R.Y., Halbert S.C., et al. Red yeast rice for dyslipidemia in statin-intolerant patients: a randomised trial. Annals of Internal Medicine. 2009;150:830-839.