Hyperkalaemia
Serum potassium and potassium balance
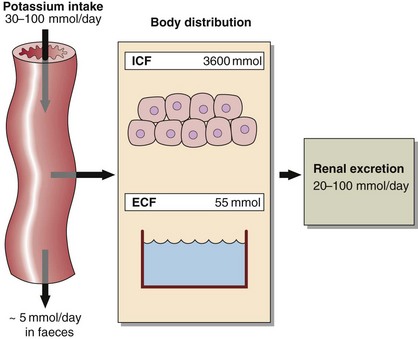
Serum potassium concentration is normally kept within a tight range (3.5–5.3 mmol/L). Potassium intake is variable (30–100 mmol/day in the UK) and potassium losses (through the kidneys) usually mirror intake. The two most important factors that determine potassium excretion are the glomerular filtration rate and the plasma potassium concentration. A small amount (~5 mmol/day) is lost in the gut. Potassium balance can be disturbed if any of these fluxes is altered (Fig 11.1). An additional factor often implicated in hyperkalaemia and hypokalaemia is redistribution of potassium. Nearly all of the total body potassium (98%) is inside cells. If, for example, there is significant tissue damage, the contents of cells, including potassium, leak out into the extracellular compartment, causing potentially dangerous increases in serum potassium (see below).
Hyperkalaemia
Hyperkalaemia is one of the commonest electrolyte emergencies encountered in clinical practice. If severe (>7.0 mmol/L), it is immediately life-threatening and must be dealt with as an absolute priority; cardiac arrest may be the first manifestation. ECG changes seen in hyperkalaemia (Fig 11.2) include the classic tall ‘tented’ T-waves and widening of the QRS complex, reflecting altered myocardial contractility. Other symptoms include muscle weakness and paraesthesiae, again reflecting involvement of nerves and muscles.
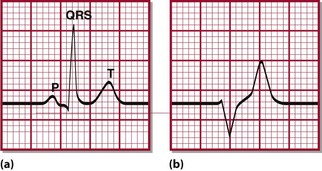
Fig 11.2 Typical ECG changes associated with hyperkalaemia. (a) Normal ECG (lead II). (b) Patient with hyperkalaemia: note peaked T-wave and widening of the QRS complex.
Hyperkalaemia can be categorized as due to increased intake, redistribution or decreased excretion.
Decreased excretion
In practice, virtually all patients with hyperkalaemia will have a reduced GFR.
 Renal failure. The kidneys may not be able to excrete a potassium load when the glomerular filtration rate is very low, and hyperkalaemia is a central feature of reduced glomerular function. It is exacerbated by the associated metabolic acidosis, due to the accumulation of organic ions that would normally be excreted.
Renal failure. The kidneys may not be able to excrete a potassium load when the glomerular filtration rate is very low, and hyperkalaemia is a central feature of reduced glomerular function. It is exacerbated by the associated metabolic acidosis, due to the accumulation of organic ions that would normally be excreted.
 Hypoaldosteronism. Aldosterone stimulates sodium reabsorption in the renal tubules at the expense of potassium and hydrogen (see p. 15). This mineralocorticoid activity is shared by many steroid molecules. Deficiency, antagonism or resistance results in loss of sodium, causing a decreased GFR with associated retention of potassium and hydrogen ions. In clinical practice, hyperkalaemia due to hypoaldosteronism is most often seen with the use of angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) to treat hypertension; spironolactone and other potassium-sparing diuretics also antagonize the effect of aldosterone. Less frequently, adrenal insufficiency is responsible (see pp. 96–97).
Hypoaldosteronism. Aldosterone stimulates sodium reabsorption in the renal tubules at the expense of potassium and hydrogen (see p. 15). This mineralocorticoid activity is shared by many steroid molecules. Deficiency, antagonism or resistance results in loss of sodium, causing a decreased GFR with associated retention of potassium and hydrogen ions. In clinical practice, hyperkalaemia due to hypoaldosteronism is most often seen with the use of angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) to treat hypertension; spironolactone and other potassium-sparing diuretics also antagonize the effect of aldosterone. Less frequently, adrenal insufficiency is responsible (see pp. 96–97).
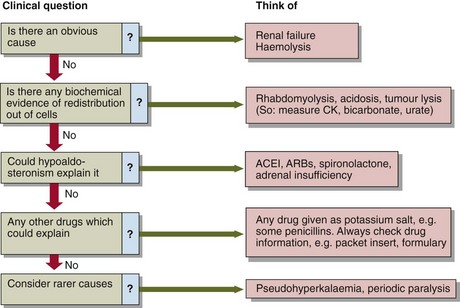
Figure 11.4 describes an approach to the evaluation of hyperkalaemia.
Redistribution out of cells
 Potassium release from damaged cells. The potassium concentration inside cells (~140 mmol/L) means that cell damage can give rise to marked hyperkalaemia. This occurs in rhabdomyolysis (where skeletal muscle is broken down), extensive trauma, or rarely tumour lysis syndrome, where malignant cells break down.
Potassium release from damaged cells. The potassium concentration inside cells (~140 mmol/L) means that cell damage can give rise to marked hyperkalaemia. This occurs in rhabdomyolysis (where skeletal muscle is broken down), extensive trauma, or rarely tumour lysis syndrome, where malignant cells break down.
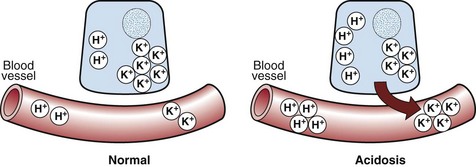
 Metabolic acidosis. There is a reciprocal relationship between potassium and hydrogen ions. As the concentration of hydrogen ions increases with the development of metabolic acidosis, so potassium ions inside cells are displaced from the cell by hydrogen ions in order to maintain electrochemical neutrality (Fig 11. 3). These hydrogen ion changes cause marked alterations in serum potassium.
Metabolic acidosis. There is a reciprocal relationship between potassium and hydrogen ions. As the concentration of hydrogen ions increases with the development of metabolic acidosis, so potassium ions inside cells are displaced from the cell by hydrogen ions in order to maintain electrochemical neutrality (Fig 11. 3). These hydrogen ion changes cause marked alterations in serum potassium.
 Insulin deficiency. Insulin stimulates cellular uptake of potassium, and plays a central role in treatment of severe hyperkalaemia. Where there is insulin deficiency or severe resistance to the actions of insulin, as in diabetic ketoacidosis (see pp. 66–67), hyperkalaemia is an associated feature.
Insulin deficiency. Insulin stimulates cellular uptake of potassium, and plays a central role in treatment of severe hyperkalaemia. Where there is insulin deficiency or severe resistance to the actions of insulin, as in diabetic ketoacidosis (see pp. 66–67), hyperkalaemia is an associated feature.
 Pseudohyperkalaemia. This should be considered when the cause of hyperkalaemia is not readily apparent. Indeed, it is important largely because it can lead to diagnostic dilemmas. It is dealt with in detail below.
Pseudohyperkalaemia. This should be considered when the cause of hyperkalaemia is not readily apparent. Indeed, it is important largely because it can lead to diagnostic dilemmas. It is dealt with in detail below.
 Hyperkalaemic periodic paralysis. This is a rare familial disorder with autosomal dominant inheritance. It presents typically as recurrent attacks of muscle weakness or paralysis, often precipitated by rest after exercise.
Hyperkalaemic periodic paralysis. This is a rare familial disorder with autosomal dominant inheritance. It presents typically as recurrent attacks of muscle weakness or paralysis, often precipitated by rest after exercise.
Treatment
 Calcium – usually in the form of calcium gluconate or calcium chloride should be given to counteract the effects of hyperkalaemia on the resting membrane potential of cells.
Calcium – usually in the form of calcium gluconate or calcium chloride should be given to counteract the effects of hyperkalaemia on the resting membrane potential of cells.
 Insulin and glucose should be given to promote the uptake of potassium by muscule tissues.
Insulin and glucose should be given to promote the uptake of potassium by muscule tissues.
 The underlying cause of the reduction in GFR should be sought and corrected when possible. If the GFR cannot be restored the patient will need to be dialysed. Units treating acutely ill patients will have a written local protocol that should be followed.
The underlying cause of the reduction in GFR should be sought and corrected when possible. If the GFR cannot be restored the patient will need to be dialysed. Units treating acutely ill patients will have a written local protocol that should be followed.
Cation exchange resins are not suitable for the treatment of severe hyperkalaemia. They are only useful in the treatment of modest slow increases in potassium.