Chapter 41
Hypercholesterolemia
1. Who should be screened for hypercholesterolemia?
2. True or false: Coronary atherosclerosis is common in persons in their 20s and 30s.
3. What are the ATP III classifications of LDL cholesterol, total cholesterol, HDL cholesterol, and triglyceride levels based on measured values?
The values, as denoted in ATP III, are given in Table 41-1. Note that since publication of this classification in 2001, a goal of LDL less than 70 mg/dL has emerged as desirable in some very high-risk populations and thus an LDL of significantly less than 100 mg/dL would now be considered optimal in such patients. To convert the values in the table to mmol/L, divide by 88.6.
TABLE 41-1
NCEP-ATP III CLASSIFICATION OF LDL, TOTAL CHOLESTEROL, HDL CHOLESTEROL, AND TRIGLYCERIDE LEVELS∗
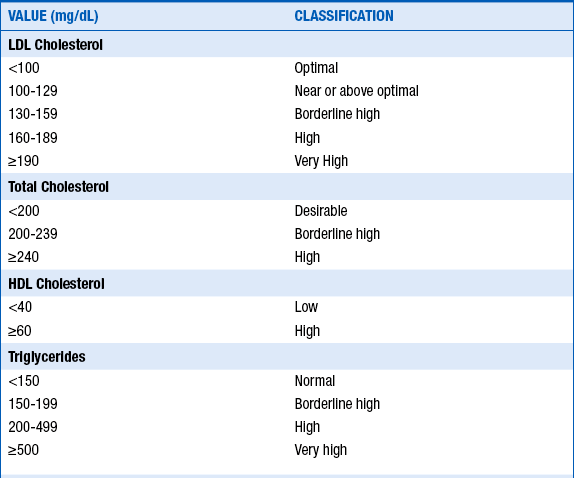
To convert mg/dL to mmol/L, divide by 88.6.
∗Note that since publication of this classification, a goal of LDL less than 70 mg/dL has emerged as desirable in some very-high risk populations.
Modified from Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults: Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 285:2486-2497, 2001.
4. What are important secondary causes of hypercholesterolemia?
 Chronic renal failure or nephrotic syndrome
Chronic renal failure or nephrotic syndrome
 Drugs (e.g., progestins, anabolic steroids, or corticosteroids)
Drugs (e.g., progestins, anabolic steroids, or corticosteroids)
A lipoprotein is the particle that transports cholesterol and triglycerides. Lipoproteins are composed of proteins (called apolipoproteins), phospholipids, triglycerides, and cholesterol (Fig. 41-1).
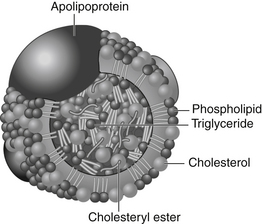
Figure 41-1 A lipoprotein particle. The polar surface coat is composed of apoproteins, phospholipids, and free cholesterol. The nonpolar lipid core is composed of cholesterol esters and triglycerides. (From Genest J, Libby P: Lipoprotein disorders and cardiovascular disease. In Libby P, Bonow RO, Mann DL, Zipes DP, editors: Braunwald’s heart disease: a textbook of cardiovascular medicine, ed 8, Philadelphia, 2008, Saunders.)
7. What is the minimal LDL goal for secondary prevention?
The minimal LDL goal for secondary prevention in patients with established coronary artery disease (CAD) is an LDL less than 100 mg/dL. This is also now the goal in patients with coronary heart disease risk equivalents (see Question 8). In an update to ATP III, it was emphasized that an LDL less than 100 mg/dL is a minimal goal of therapy. In light of more recent studies (Pravastatin or Atorvastatin Evaluation and Infection Therapy [PROVE-IT], Heart Protection Study [HPS], and Treating to New Targets [TNT]), a goal of LDL less than 70 mg/dL should be considered in patients with coronary heart disease at very high risk. Patients with coronary heart disease classified as very high risk include those with the following:
 Multiple major coronary risk factors (especially diabetes)
Multiple major coronary risk factors (especially diabetes)
 Severe and poorly controlled risk factors (especially continued cigarette smoking)
Severe and poorly controlled risk factors (especially continued cigarette smoking)
 Multiple risk factors of metabolic syndrome (see Question 9)
Multiple risk factors of metabolic syndrome (see Question 9)
8. What is a coronary heart disease risk equivalent?
 Other clinical forms of atherosclerosis (e.g., peripheral arterial disease, abdominal aortic aneurysm, and symptomatic carotid artery disease)
Other clinical forms of atherosclerosis (e.g., peripheral arterial disease, abdominal aortic aneurysm, and symptomatic carotid artery disease)
 Multiple cardiac risk factors that confer a 10-year risk for CAD greater than 20% (based on the Framingham risk table)
Multiple cardiac risk factors that confer a 10-year risk for CAD greater than 20% (based on the Framingham risk table)
9. What factors make up metabolic syndrome?
 Abdominal obesity (waist circumference in men more than 40 inches [102 cm] or in women more than 35 inches [88 cm])
Abdominal obesity (waist circumference in men more than 40 inches [102 cm] or in women more than 35 inches [88 cm])
 Triglycerides 150 mg/dL or more
Triglycerides 150 mg/dL or more
 Low HDL cholesterol (less than 40 mg/dL in men or less than 50 mg/dL in women)
Low HDL cholesterol (less than 40 mg/dL in men or less than 50 mg/dL in women)
10. What medications should be used to lower LDL levels?
Statins are the first-line agents to lower LDL levels. If adequate LDL lowering is not achieved, a more potent statin can be considered. If adequate LDL is still not achieved, either a bile acid sequestrant, fibrate, or nicotinic acid should be added. Note that patients may need to be followed more carefully for side effects, such as liver function test (LFT) elevation and myopathy, with certain combination therapies. At the time of this writing, and likely until the results of the Improved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT) are presented, ezetimibe should only be used as a secondary agent if the agents listed here are not tolerated or do not lead to adequate LDL reduction. Table 41-2 summarizes the drugs used to treat hypercholesterolemia, their effects, and their side effects.
TABLE 41-2
DRUGS USED IN THE TREATMENT OF HYPERCHOLESTEROLEMIA
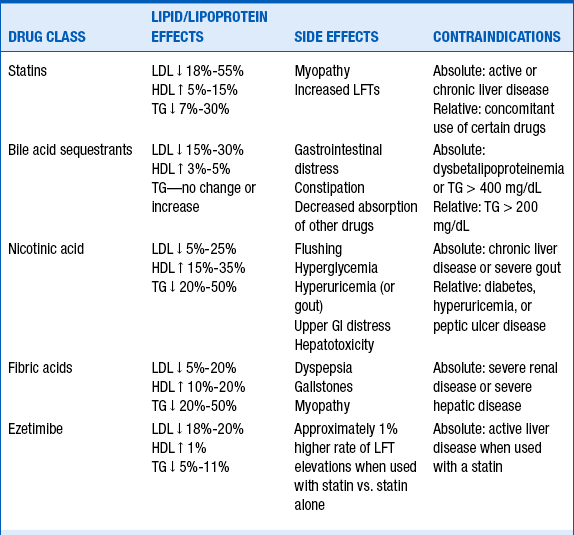
Modified from Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults: Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 285:2486-2497, 2001.
11. Is there an age cutoff for secondary prevention therapy with statins?
No. Older secondary prevention trials with statins included many patients in their 60s and 70s and demonstrated benefit in older and younger patients. Thus, for secondary prevention, according to ATP III, “no hard-and-fast age restrictions appear necessary when selecting persons with established coronary heart disease for LDL-lowering therapy.” Since publication of ATP III, the Prospective Study of Pravastatin in the Elderly at Risk (PROSPER), and several other trials were published. In PROSPER, subjects age 70 to 82 with a history of vascular disease or risk factors were randomized to treatment with pravastatin or placebo. After an average of 3.2 years of follow-up, the composite ischemic endpoint was reduced by 15%. The results of PROSPER, HPS, and Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) reinforce that statin therapy should be used in elderly patients for secondary prevention and should be seriously considered in elderly patients for primary prevention.
12. What is non-HDL cholesterol?
The non-HDL cholesterol level is the total cholesterol level minus HDL cholesterol level. It is an approximation of very-low-density lipoprotein (VLDL) plus LDL levels. VLDL cholesterol is felt in clinical practice to be the most readily available measure of atherogenic remnant lipoproteins. Reduction of non-HDL cholesterol is considered a secondary target of therapy in persons with high triglycerides (200 mg/dL or more). The goals for non-HDL cholesterol are generally 30 mg/dL higher than those for LDL cholesterol (Box 41-1). For example, in patients with coronary heart disease and coronary heart disease risk equivalents, the LDL goal is less than 100 mg/dL and the non-HDL goal is less than 130 mg/dL.
13. What factors and conditions are believed to be associated with or cause low HDL cholesterol?
 Very high carbohydrate intakes (more than 60% of energy intake)
Very high carbohydrate intakes (more than 60% of energy intake)
 Certain drugs (e.g., beta-adrenergic blocking agents [β-blockers], anabolic steroids, and progestational agents)
Certain drugs (e.g., beta-adrenergic blocking agents [β-blockers], anabolic steroids, and progestational agents)
14. What is the difference between myopathy, myalgia, myositis, and rhabdomyolysis?
 Myopathy: general term referring to any disease of muscles
Myopathy: general term referring to any disease of muscles
 Myalgia: muscle ache or weakness without creatine kinase (CK) elevation
Myalgia: muscle ache or weakness without creatine kinase (CK) elevation
 Myositis: muscle symptoms with increased CK levels
Myositis: muscle symptoms with increased CK levels
 Rhabdomyolysis: muscle symptoms with marked CK elevation (more than 10 times the upper limit of normal [ULN])
Rhabdomyolysis: muscle symptoms with marked CK elevation (more than 10 times the upper limit of normal [ULN])
15. What is the incidence of nonspecific muscle aches or joint pains in patients treated with statins?
Bibliography, Suggested Readings, and Websites
1. Baylor College of Medicine. Lipids Online website. Available at http://www.lipidsonline.org. Accessed February 27, 2013
2. Brunzell, J.D., Davidson, M., Furberg, C.D., et al. Lipoprotein management in patients with cardiometabolic risk. J Am Coll Cardiol. 2008;51:1512–1524.
3. Genest, J., Libby, P. Lipoprotein disorders and cardiovascular disease. In Libby P., Bonow R.O., Mann D.L., Zipes D.P., eds.: Braunwald’s heart disease: a textbook of cardiovascular medicine, ed 8, Philadelphia: Saunders, 2008.
4. Grundy, S.M., Cleeman, J.I., Merz, C.N., et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. J Am Coll Cardiol. 2004;44:720–732.
5. Pasternak, R.C., Smith, S.C., Jr., Bairey-Merz, C.N., et al. ACC/AHA/NHLBI clinical advisory on the use and safety of statins. Circulation. 2002;106:1024–1028.
6. Rosenson, R.S. Overview of Treatment of Hypercholesterolemia. Available at: http://www.utdol.com.
7. Rosenson, R.S. Screening Guidelines for Dyslipidemia. In Basow, DS, editor: UpToDate, Waltham, MA, 2013, UpToDate. Available at: http://www.uptodate.com/contents/screening-guidelines-for-dyslipidemia. Accessed March 26, 2013
8. Smith, S.C., Jr., Allen, J., Blair, S.N., et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113:2363–2372.
9. Smith, S.C., Jr., Benjamin, E.J., Bonow, R.O., Braun, L.T., et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58:2432–2446.

















