Hypercalcaemia
Diagnosis
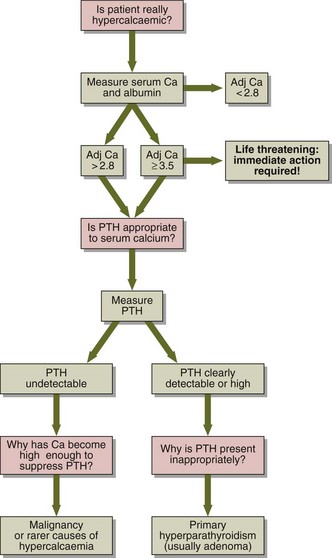
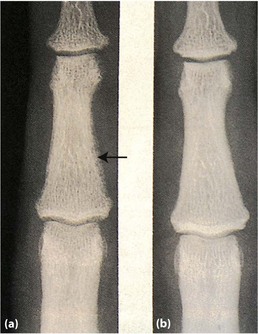
A diagnostic decision chart is shown in Figure 36.1. Primary hyperparathyroidism is most often due to a single parathyroid adenoma, which secretes PTH independently of feedback control by plasma calcium. Hypercalcaemia associated with malignancy is the commonest cause of a high calcium in a hospital population. Some tumours secrete a protein called PTHrP (parathyroid hormone-related protein), which has PTH-like properties.
Rarer causes of hypercalcaemia include:
 Inappropriate dosage of vitamin D or metabolites, e.g. in the treatment of hypoparathyroidism or renal disease or due to self-medication.
Inappropriate dosage of vitamin D or metabolites, e.g. in the treatment of hypoparathyroidism or renal disease or due to self-medication.
 Granulomatous diseases (such as sarcoidosis or tuberculosis) or certain tumours (such as lymphomas) synthesize 1,25-dihydroxycholecalciferol.
Granulomatous diseases (such as sarcoidosis or tuberculosis) or certain tumours (such as lymphomas) synthesize 1,25-dihydroxycholecalciferol.
 Thyrotoxicosis very occasionally leads to increased bone turnover and hypercalcaemia.
Thyrotoxicosis very occasionally leads to increased bone turnover and hypercalcaemia.
 Thiazide therapy: the hypercalcaemia is usually mild.
Thiazide therapy: the hypercalcaemia is usually mild.
 Immobilization: especially in young people and patients with Paget’s disease.
Immobilization: especially in young people and patients with Paget’s disease.
 Renal disease. Long-standing secondary hyperparathyoidism may lead to PTH secretion becoming independent of calcium feedback. This is termed tertiary hyperparathyroidism.
Renal disease. Long-standing secondary hyperparathyoidism may lead to PTH secretion becoming independent of calcium feedback. This is termed tertiary hyperparathyroidism.
 Calcium therapy. Patients are routinely given calcium-containing solutions during cardiac surgery, and may have transient hypercalcaemia afterwards.
Calcium therapy. Patients are routinely given calcium-containing solutions during cardiac surgery, and may have transient hypercalcaemia afterwards.
 Diuretic phase of acute renal failure or in the recovery from severe rhabdomyolysis.
Diuretic phase of acute renal failure or in the recovery from severe rhabdomyolysis.
 Milk alkali syndrome: the combination of an increased calcium intake together with bicarbonate, as in a patient self-medicating with proprietary antacid, may cause severe hypercalcaemia, but the condition is very rare.
Milk alkali syndrome: the combination of an increased calcium intake together with bicarbonate, as in a patient self-medicating with proprietary antacid, may cause severe hypercalcaemia, but the condition is very rare.
Treatment
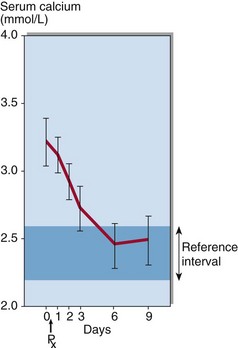
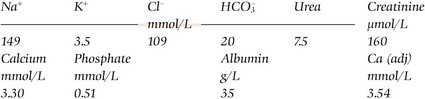
Treatment is urgent if the adjusted serum calcium is greater than 3.5 mmol/L; the priority is to reduce it to a safe level. Intravenous saline is administered first to restore the glomerular filtration rate and promote a diuresis. Although steroids, mithramycin, calcitonin and intravenous phosphate have been used, compounds known as the bisphosphonates have been found to have the best calcium-lowering effects. Bisphosphonates such as pamidronate have become the treatment of choice in patients with hypercalcaemia of malignancy (Fig 36.2). It acts by inhibiting bone resorption.