Humerus and Elbow
Perspective
Anatomy
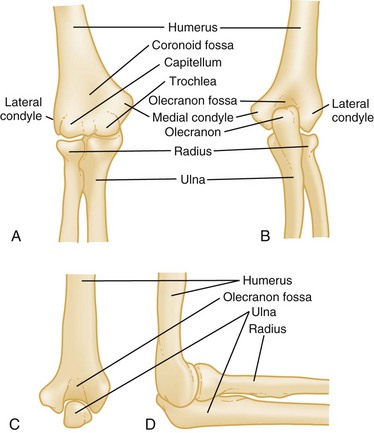
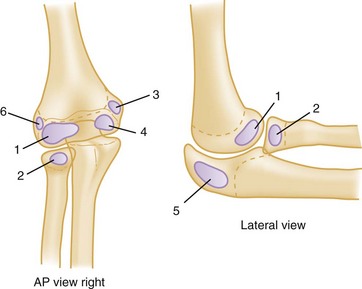
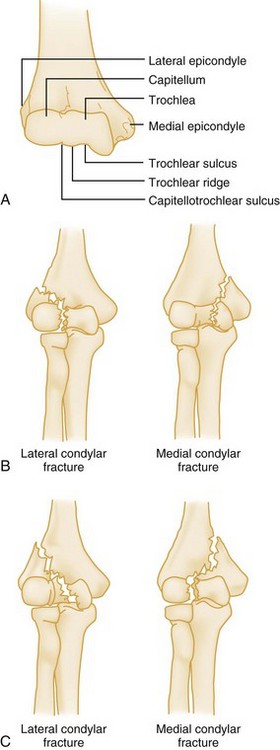
The bony anatomy of the distal humerus and elbow is diagrammed in Figure 52-1. The distal end of the humerus tapers into two columns of bone, the medial and lateral condyles. Between the condyles, the bone thins, and the recess created is the coronoid fossa. The more proximal nonarticular portions of the condyles are the epicondyles. Just proximal to the epicondyles, the supracondylar ridges run up each side of the humerus. Collectively, these areas serve as points of origin for the muscles of the forearm. The wrist flexors originate from the medial epicondyle, and the wrist extensors originate from the lateral epicondyle. Fractures of the distal humerus often result in fragment displacement because of the pull of these strong forearm muscles on attachment sites.
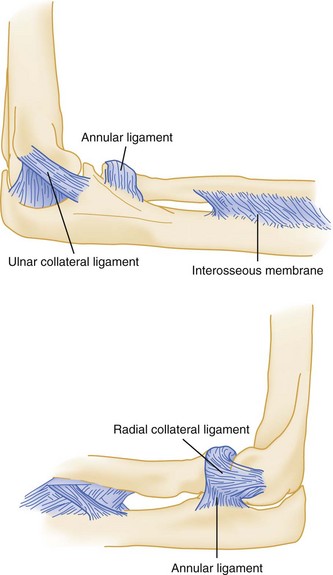
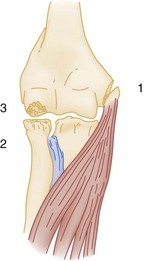
Four ligamentous structures are important in evaluating elbow injuries (Fig. 52-2). The radial head is held in place by the annular ligament and the adjacent radial collateral ligament. Rotation of the radial head within the confines of the fibrous annular ligament permits pronation and supination. In addition, the ulnar collateral ligament and anterior capsule add stability to the joint. Fracture or dislocation of the joint may severely damage the ligamentous structures.
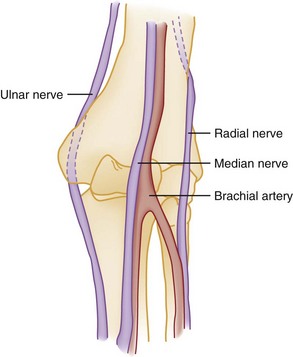
The neurovascular structures of this area are shown in Figure 52-3. The brachial artery, which is the continuation of the axillary artery, travels with the median nerve in the anterior compartment of the upper arm. It enters the antecubital fossa and bifurcates into the radial and ulnar arteries.
One important anatomic variation is the presence of a supracondylar process (in approximately 2.5% of cases) just proximal to the medial epicondyle (Fig. 52-4). When the supracondylar process is present, the median nerve and brachial artery must traverse behind this process, then forward between a fibrous band connecting the process to the epicondyle. Median nerve symptoms may develop if this process is fractured or if an injury causes swelling in the vicinity of the supracondylar process.
Clinical Features
Physical Examination
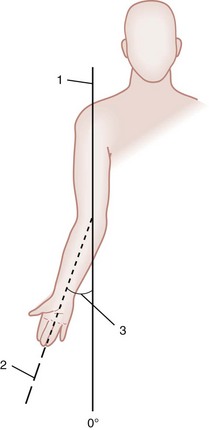
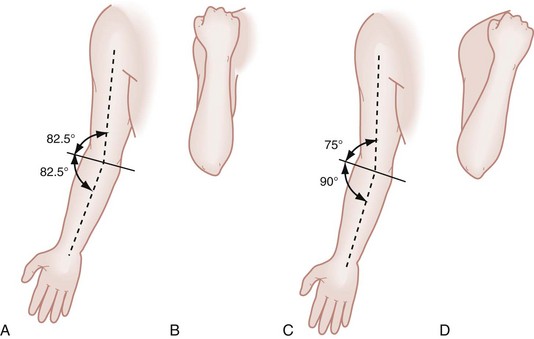
One special aspect of the elbow examination is the determination of the carrying angle, the normal outward angulation of the extended forearm at the elbow. This angle allows the long axes of the humerus and forearm to become superimposed when the elbow is flexed (Fig. 52-5). This angle varies from 5 to 20 degrees in adults, with men having less angulation than women. Measurement of the carrying angle is helpful in assessing subtle supracondylar fractures in children. As shown in Figure 52-6, lines drawn parallel to the shafts of the humerus and ulna intersect to form an angle with a mean measurement in children of 13 degrees, although this angle varies widely.1 A difference in carrying angles of greater than 12 degrees (from one side to the other for a particular individual) is associated with fractures. However, the carrying angle is used primarily for assessing the adequacy of reduction or the results of fracture healing rather than for acute diagnosis, because it is difficult for children to fully extend the arm during the initial evaluation for this measurement to be obtained.
Radiographic Findings
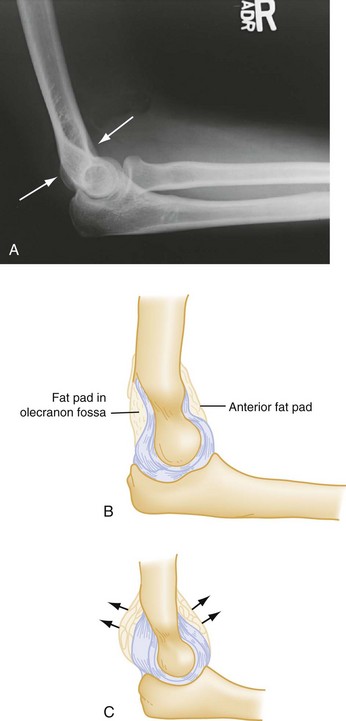
Many fractures in the elbow region are obvious on plain film, with cortical disruption, angulation, or displacement of fragments. Minor fractures can be subtle and may be missed. Special attention to the contour of the radial head and the fat pads reduces the risk of missing fractures. The normal cortex of the radius is smooth and has a gentle continuous concave sweep. If consistent with history and physical findings, any disruption of this smooth arc is considered evidence of fracture. Abnormalities within the soft tissues on elbow films are particularly important and may be the only radiographic sign of a fracture. Normally, fat surrounding the proximal elbow joint is hidden in the concavity of the olecranon and coronoid fossae. The normal elbow has only a narrow strip of lucency anteriorly (the anterior fat pad), and a posterior fat pad is not visible on radiographs. Injuries that produce intra-articular hemorrhage cause distention of the synovium and displace the fat out of the fossa, making the posterior fat pad visible on lateral radiographic views. The anterior fat pad also is altered by this swelling, becoming more prominent and taking the shape of a spinnaker sail from a boat: “sail sign” (Fig. 52-7). In the setting of trauma, more than 95% of patients with the “posterior fat pad” sign have intra-articular skeletal injury. These soft tissue findings occur even with subtle fractures, and when they are present in the setting of trauma, an occult fracture is considered to be present even when not visible on radiographs. In adults, a radial head fracture is implied, whereas in children a supracondylar fracture is the more likely underlying injury. In the absence of trauma, the presence of a fat pad suggests other causes of effusion (e.g., gout, infection, bursitis). The fat pad signs may be absent in fractures where the injury is severe enough to rupture the capsule.
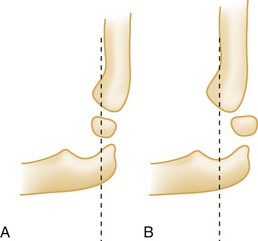
The anterior humeral line is a line drawn on a lateral radiograph along the anterior surface of the humerus through the elbow. Normally, this line transects the middle third of the capitellum (Fig. 52-8). With an extension supracondylar fracture, this line either transects the anterior third of the capitellum or passes entirely anterior to it. The abnormal relationship between the anterior-humeral line and capitellum may be the only evidence of a minimally displaced supracondylar fracture and is a presumptive finding of a fracture.
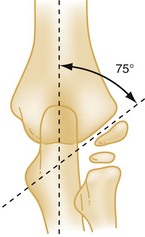
Another diagnostic aid in evaluating radiographs of possible supracondylar fractures in children is the determination of Baumann’s angle. As shown in Figure 52-9, the intersection of a line drawn on the anteroposterior film through the midshaft of the humerus and the growth plate of the capitellum defines an angle of approximately 75 degrees. In normal children, Baumann’s angle is the same in both elbows, and it has been suggested that a comparison between the injured and uninjured sides be used to assess the accuracy of reduction. An increase in Baumann’s angle indicates medial tilting of the distal fragment. Alteration in Baumann’s angle is thought to predict the final carrying angle when the fracture heals, although there is controversy regarding its reliability.2
Radiographic evaluation of the elbow in children is difficult because of the presence of multiple ossification centers (Fig. 52-10). Table 52-1 lists the typical age of first appearance and fusion of ossification centers, which gives rise to the CRITOE acronym:
Table 52-1
Ossification Centers of the Elbow: CRITOE
| OSSIFICATION CENTERS | AGE OF APPEARANCE |
| Capitellum | 1-2 |
| Radial head | 4-5 |
| Internal (medial) epicondyle | 4-5 |
| Trochlea | 8-10 |
| Olecranon | 8-9 |
| External (lateral) epicondyle | 10-11 |
Fractures
Injuries in the region of the shaft of the humerus and about the elbow fall into several categories (Box 52-1). Emergency department (ED) management varies with location and type of fracture or dislocation. Supracondylar fractures of the humerus in children are usually described according to the Gartland classification (Box 52-2).
Fractures of the Shaft of the Humerus
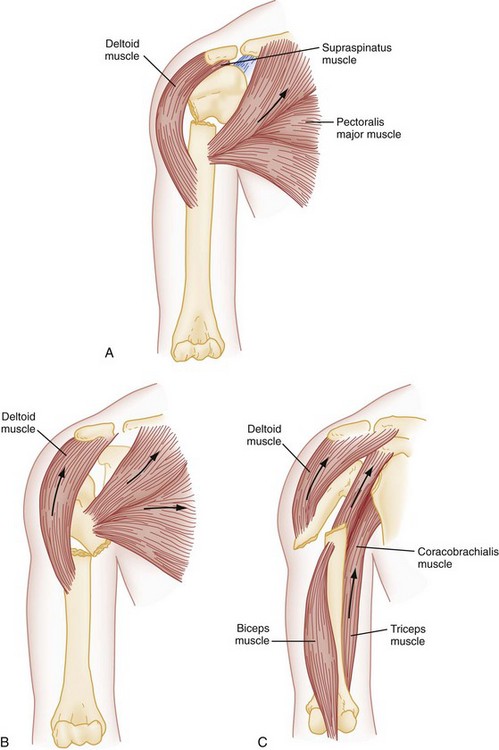
Fractures of the humeral shaft commonly result from a direct blow to the arm, such as occurs during a fall or motor vehicle collision. Severe twisting of the arm or a fall on an outstretched hand can also produce this type of fracture. Fractures produced by violent muscle contraction, such as occurs when a javelin or baseball is thrown, also are reported.3 Motion of the humerus is controlled by several muscle groups, which also influence the fracture pattern of the humeral shaft. If the fracture is located proximal to the attachment of the pectoralis major, the proximal fragment of the humerus abducts and rotates internally owing to the action of the rotator cuff, whereas the distal fragment is displaced medially by the pectoralis major (Fig. 52-11A). If the fracture occurs below the pectoralis major insertion but above the deltoid insertion, the distal fragment is displaced laterally by the deltoid muscle, and the proximal fragment is displaced medially by the pull of the pectoralis major, latissimus dorsi, and teres major muscles (Fig. 52-11B). In fractures occurring distal to the deltoid insertion, the proximal fragment is abducted by the deltoid, and the distal fragment is proximally displaced (Fig. 52-11C). The shaft of the humerus most commonly fractures in the middle third in a transverse fashion (Fig. 52-12).

Figure 52-12 Pathologic fracture of proximal humerus.
Clinical Features
Radiographic findings are confirmatory. Studies routinely should include the shoulder and elbow joints. The humerus is a common site for benign tumors, unicameral cysts, and primary bone malignancies. The humeral shaft also is a common site for metastatic disease. Thinning of the cortex and abnormal osteoblastic or osteoclastic activity are evidence of a pathologic fracture (see Fig. 52-12). These fractures do not heal without concomitant treatment of the underlying pathologic condition.
Management
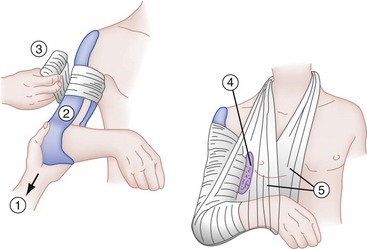
Closed fractures that are isolated injuries are treated conservatively with a high degree of success. Elaborate attempts at fracture reduction and external immobilization are unnecessary and sometimes detrimental to healing. Humeral shaft fractures remain surrounded by a richly vascularized envelope of muscle so that fracture reduction is accomplished most easily with the aid of gravity and muscle balance. Fractures that are nondisplaced or minimally displaced are immobilized by adding a coaptation, or “sugar-tong,” splint, to the sling and swathe (Fig. 52-13). This is accomplished by first padding the extremity, then carrying a long plaster splint from the lateral side of the shoulder, down the lateral aspect of the upper arm, around the elbow with the elbow flexed, and then up the inner aspect of the arm to the axilla. The sugar tong is wrapped in an elastic bandage, and a sling is used to support the arm in 90 degrees or less of flexion. The weight of the splint aided by gravity applies traction while it immobilizes the fracture. Some authorities use the coaptation splint for only the first 10 to 14 days of treatment, followed by a functional brace.
If the fracture is grossly displaced or comminuted, the hanging cast technique sometimes is used. This technique is especially effective with spiral fractures. The cast is lightweight, applied at least 1 inch proximal to the fracture site, and extends to the distal palmar crease of the hand. The elbow is flexed 90 degrees, and the wrist is placed in the neutral position. The sling is attached through a loop at the wrist. Angulation is corrected by placing the plaster loop on the dorsal aspect of the cast (to reduce lateral angulation) or on the volar side of the cast (to reduce medial angulation). Anterior or posterior angulation is corrected by altering the length of the sling apparatus (Fig. 52-14). Care is taken not to make the cast too heavy because this would distract fracture fragments. The hanging cast has the disadvantage of requiring gravity for traction and requires that the patient remain upright at all times, including during sleep, a situation that many patients find intolerable. Neurovascular examination should be repeated and documented after the application of any splint or cast, because loss of nerve function from entrapment of the nerve between fragments can occur after these interventions.
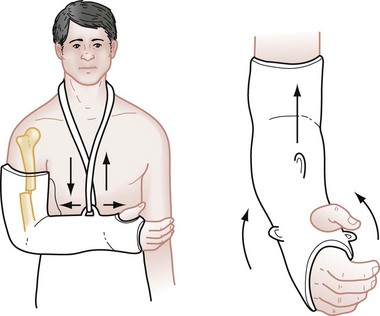
Figure 52-14 Hanging cast technique.
The use of open reduction and internal fixation (Fig. 52-15) has been more frequent recently and is necessary in certain circumstances, including open fractures, presence of multiple injuries that preclude mobilization, bilateral fractures, poor reduction, poor patient compliance, failure of closed treatment, and fractures through pathologic bone.4,5 Isolated radial nerve palsy usually is assumed to be a neurapraxia and is managed nonoperatively. Exploration and internal fixation are indicated, however, if the radial nerve palsy develops after manipulation because this is highly suggestive of nerve entrapment.4
Fractures of the Distal Humerus
Distal humerus fractures that occur proximal to the epicondyles are called supracondylar fractures. This type of fracture is almost exclusively an injury of the immature skeleton, with a peak incidence in children 5 to 10 years old6 This injury rarely occurs after age 15 and accounts for approximately one half of all elbow fractures and one third of pediatric limb fractures. In children, the tensile strength of the collateral ligaments and joint capsule of the elbow is greater than that of bone. In adults, the reverse is true, and a posterior elbow dislocation is sustained instead. Supracondylar fractures are classified as either extension or flexion fractures, depending on the mechanism of injury and the displacement of the distal fragment. Of these injuries, 98% are of the extension type.
Extension Supracondylar Fractures:
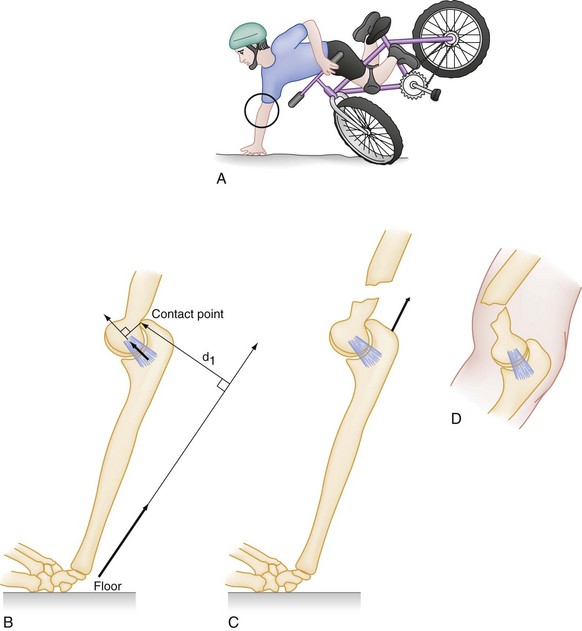
Pathophysiology.: Extension supracondylar fractures occur as a consequence of a fall on the outstretched arm when the elbow is either fully extended or hyperextended (e.g., a fall off the “monkey bars”). The elbow is likely to be in the latter position at the time of the fall because ligamentous laxity, with hyperextension of the joints, is a normal phenomenon in younger children. With the forearm acting as a lever,7 the ground reaction produces a moment of force at the elbow (Fig. 52-16). Ultimately the distal humerus fails anteriorly in the supracondylar area. The strong action of the triceps tends to pull and displace the distal fragment in a posterior and proximal direction. There may be anterior angulation of the sharp distal end of the proximal fragment into the antecubital fossa, endangering the brachial artery and median nerve (Fig. 52-17). In most cases, however, the brachialis muscle protects the anterior neurovascular structures from injury.
Clinical Features.: A child with a complete fracture comes to the ED holding the upper extremity immobile in extension to the side, with a typical S-shaped configuration and tenderness and swelling in the region of the elbow. Prominence of the olecranon attached to the posteriorly displaced distal fragment is similar to that seen with posterior dislocation of the elbow. When an incomplete supracondylar fracture exists, the diagnosis may be less obvious, with an elbow effusion as the only clinical sign. A careful neurovascular examination is essential. Although palpation is useful in determining the site of injury, the examining physician should avoid manipulation of the injury to elicit crepitus because movement can cause further neurovascular damage. Alleviating pain often facilitates the examination.
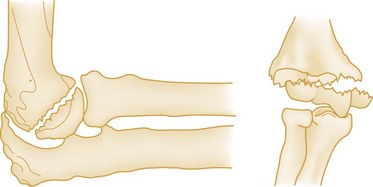
Diagnostic Strategies.: On radiographic examination, the distal fragment is often displaced on the lateral view. This displacement is most likely to occur with a complete fracture wherein the muscle activity results in proximal migration of the distal fragment. Because this fracture occurs in children, 25% of supracondylar fractures are of the greenstick variety, with the posterior cortex remaining intact. Subtle changes (e.g., the presence of a posterior fat pad or an abnormal anterior humeral line) may be the only radiographic clues to the presence of a fracture (Fig. 52-18). In displaced fractures on the anteroposterior view, the distal fragments may be displaced either medially or laterally in relationship to the humerus. Often, with minimally displaced fractures, the fracture line is transverse and not visible on the anteroposterior view. Based on radiographic findings, extension supracondylar fractures are classified into three types: type I, minimal or no displacement; type II, displaced fracture, posterior cortex intact; and type III, totally displaced fracture, anterior and posterior cortex disrupted.
Management.: Nondisplaced fractures (type I) are immobilized primarily for comfort and protection because they are inherently stable. They are treated in a splint or cast flexed to 90 degrees with the forearm in neutral rotation. Protected active range of motion is begun in approximately 3 weeks. Even without definite radiographic findings, a child with localized tenderness consistent with a supracondylar fracture should be splinted and referred for follow-up examination within 24 to 48 hours. A radiographic study performed a few weeks after the injury may reveal periosteal new bone formation in the supracondylar region.
Minimally displaced (type II) fractures that are stable after reduction can be treated with splinting or casting with the elbow flexed. Some authors recommend flexion to 110 to 120 degrees for this injury.6,8,9 This position uses the intact posterior periosteum as a tension band to hold the reduction; however, if swelling or circulatory obstruction prevents this much flexion, it cannot and should not be used. The greater the flexion at the elbow, the greater is the chance of vascular impairment. When swelling peaks at 24 to 48 hours, the risk of vascular obstruction and compartment syndrome is the greatest. Occasionally, these injuries must be pinned percutaneously to maintain stability, especially if a significant rotational component is present. Percutaneous pinning of fractures after reduction has grown in popularity in recent years.10
These general principles should be adhered to in treating these injuries: (1) achieving adequate reduction, (2) properly assessing reduction, and (3) maintaining the reduction. Closed reduction is attempted with the patient under anesthesia. If closed reduction is not possible or if the brachial artery seems to be trapped in the fracture site, open reduction may be necessary. When adequate reduction has been achieved, most authorities recommend percutaneous pin fixation to maintain the reduction.7,11,12
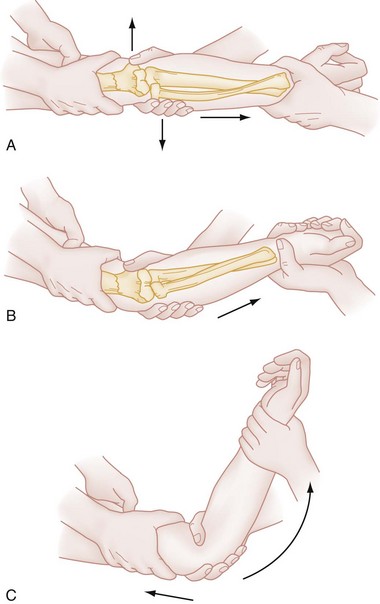
Reduction in the ED is indicated only when the displaced fracture is associated with vascular compromise that threatens the viability of the extremity. Under these conditions, closed reduction should be attempted. After appropriate procedural sedation, an assistant fixes the arm of the patient. The physician grasps the patient’s wrist and applies steady, firm traction in line with the long axis of the limb (Fig. 52-19A). The forearm is kept in the neutral, thumb-up position. While traction is maintained, correction of any medial or lateral displacement is accomplished with the other hand at the elbow (Fig. 52-19B). If the distal fragment is displaced laterally, it is pushed inward; if it is displaced medially, it is pushed outward.
After length has been restored and the angular deformity has been corrected, the thumb of the free hand is placed over the anterior surface of the proximal fragment with the fingers behind the olecranon. While traction is maintained, the elbow is gently flexed to just beyond 90 degrees (Fig. 52-19C). Angulation is corrected to a normal carrying angle.
Complications.: Ten percent of children lose the radial pulse temporarily, most often as a result of swelling and not direct brachial artery injury. Reducing the fracture, avoiding flexing the elbow more than 90 degrees, and elevating the arm help prevent secondary obstruction to arterial flow. Compartment syndrome, or Volkmann’s ischemic contracture, as a result of prolonged ischemia of the forearm is a dreaded complication but is rare in this era (reported incidence <0.5%).10
The most common complication is the loss of the carrying angle, resulting in a cubitus varus, or “gunstock,” deformity. Measurement of Baumann’s angle after reduction is predictive of the final carrying angle. Cubitus varus has been reported previously in 25 to 60% of patients, depending on the treatment method used.2,13 This incidence has decreased significantly (<10%) with the use of percutaneous pinning. The distal humerus has little capacity to remodel because only 20% of the growth of the bone derives from the distal physis. A small amount of extension or flexion deformity produces little disability, has the greatest chance of remodeling, and is not a major cosmetic concern. Valgus or varus deformities, being in the coronal plane, have little or no chance of remodeling. Although cubitus varus is not a significant functional disability, it presents a significant cosmetic problem. In most cases this complication can be corrected at a later time by an osteotomy.
Nerve injuries occurred in 7% of 4520 fractures compiled from 31 major reported series. The incidence increases to a range of 19 to 49% with increasing severity of fracture displacement.14 The interosseous nerve is the most commonly injured, followed by the radial, median, and ulnar nerves. Most deficits seen at the time of injury are neurapraxias that resolve with conservative management. Motor function returns within 7 to 12 weeks, whereas recovery of sensation may take more than 6 months.15
Flexion Supracondylar Fractures:
Pathophysiology.: Flexion-type injuries are much less common, with a reported frequency of 1 to 10%, accounting for 2% of all supracondylar fractures in a large pooled series of patients.16 The mechanism of injury is a direct blow to the flexed elbow. Energy is transferred from the posterior aspect of the proximal ulna to the distal humerus, resulting in a supracondylar fracture with anterior displacement of the distal fragment. As the fragment displaces, the periosteum is torn posteriorly.
Clinical and Radiographic Features.: The elbow is usually held in flexion rather than with the extremity in the S-shaped configuration seen in extension-type injuries. In displaced fractures, the normal olecranon process is not palpable, in contrast to the increased prominence of the olecranon seen with extension injuries.
Radiographically, these injuries can be classified into three types, similar to extension injuries:
• Type I fracture—undisplaced or minimally displaced
• Type II fracture—incomplete fracture; anterior cortex intact
• Type III fracture—completely displaced; distal fragment migrates proximally and anteriorly
Plain films may reveal a simple increase in the anterior angulation of the distal supracondylar fragment or gross displacement of the distal fragment proximal and anterior to the distal end of the proximal fragment. In the latter case, the distal end of the proximal fragment protrudes posteriorly. A line down the anterior humeral shaft intersects the capitellum either normally or posteriorly in these fractures, depending on whether there is anterior displacement.17
Management.: When the posterior periosteum is torn, the anterior periosteum functions as a tension band with the arm in extension. In type I fracture, the periosteum is minimally displaced. These injuries do not need to be immobilized in extension. The elbow can be comfortably flexed and should be immobilized in a splint as with extension injuries. Type II and III injuries should be referred to an orthopedist emergently. Type II injuries are manipulated into extension, then held either in a long arm cast or with percutaneous pins. Type III injuries often require open reduction (Fig. 52-20).
Complications.: The most common complication is injury to the ulnar nerve by posterior displacement of the proximal fragment. The radial and median nerves are rarely injured. Stiffness of the elbow also may occur, especially after open reduction. Cubitus valgus may occur but is not as cosmetically problematic as cubitus varus.
Transcondylar Fractures
Transcondylar (or dicondylar) fractures have a fracture line, either transverse or crescent shaped, that passes through both condyles within the joint capsule just proximal to the articular surface (Fig. 52-21). As with supracondylar fractures, two types have been described—extension and flexion—based on the position of the elbow when fractured. Extension types are the most common. The mechanism of injury is similar to that for supracondylar injuries. In contrast to supracondylar fractures, however, the injury is more common in elderly individuals with fragile, osteoporotic bone. These fractures generally are difficult to treat because the small distal fragment possesses little extra-articular bone, and only a small amount of bone contact is available for union.17 During healing, excessive callus may form in the olecranon or coronoid fossae with residual loss of motion. Orthopedic consultation should be immediately obtained for these injuries.
Intercondylar Fractures
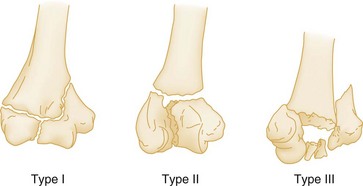
Intercondylar fractures are usually T-shaped or Y-shaped fractures with variable degrees of separation of the condyles from each other and from the proximal humerus fragment (Fig. 52-22). The distal portion of the fracture extends to the articular surface of the distal humerus. These injuries are rare and generally are seen in adults in their 50s and 60s.18 The usual mechanism of injury is direct trauma to the elbow that drives the olecranon against the humeral articular surface and splits the distal end.
Clinical and Radiographic Features.: Patients with intercondylar fractures complain of pain at the elbow, which on examination is tender to palpation. Good-quality anteroposterior and lateral radiographic views are essential in evaluating fracture displacement and comminution (Fig. 52-23). Computed tomography may be used to delineate fracture patterns further. Neurovascular complications are not common with these injuries.
Management.: Treatment of intercondylar fractures is difficult and complicated.16,19 The goal of treatment is to reestablish articular congruity and alignment and to begin active motion as soon as possible, most often through open reduction with rigid internal fixation. Closed treatment is typically restricted to elderly patients, patients with medical conditions that prohibit surgery, and certain patients with nondisplaced fractures. These injuries all should be referred to an orthopedic surgeon emergently. As with supracondylar fractures, manipulation should be avoided unless limb-threatening ischemia is present. Traction across the elbow with the arm extended is helpful in restoring blood flow to an ischemic forearm.
Complications.: Historically, loss of elbow joint function is the most common complication reported, although this now can be largely avoided with optimal surgical technique.16 Any method of treatment that requires prolonged immobilization is likely to result in fibrosis or ankylosis of the joint. Neurovascular complications are rare.
Lateral Condyle Fractures in Children
Lateral condyle fractures are the second most common fractures involving the elbow in children, after supracondylar fractures.20 The fracture has an age distribution similar to that of supracondylar fracture and occurs after a fall on the outstretched hand, with a varus stress applied to the extended arm.
Clinical and Radiographic Features.: Tenderness and swelling are noted over the lateral aspect of the elbow. In general, children exhibit less swelling than with supracondylar fractures, and neurovascular compromise is uncommon. Diagnosis is usually made on standard anteroposterior and lateral views, although an oblique view also may be helpful. These fractures are notoriously difficult to diagnose because fractures with minimal displacement are difficult to see radiographically and are often misdiagnosed as supracondylar humerus fractures.
Management.: Nondisplaced fractures are treated nonoperatively with a cast, whereas fractures with any displacement require closed or open reduction with percutaneous pin fixation for 3 to 4 weeks.20,21
Complications.: The risk of neurovascular compromise is much lower than with supracondylar humerus fractures. Fractures diagnosed and treated in a timely manner should have few complications, although historically, nonunion, cubitus varus or valgus, and fishtail deformity (avascular necrosis) have been reported.22
Medial Condyle Fractures in Children
Medial condyle fractures are rare, comprising 1 to 2% of pediatric elbow fractures.23 These fractures are type IV Salter-Harris injuries with physeal injury a possible outcome. The mechanism of injury is believed to be a valgus force on the extended elbow.
Clinical and Radiographic Features.: The patient has tenderness and swelling over the medial aspect of the elbow. Anteroposterior, lateral, and oblique films may show the fracture in older children, but because the trochlea does not ossify until about age 9, plain films in younger children do not show the fracture. Magnetic resonance imaging (MRI) may be necessary to confirm the diagnosis in these patients.
Condylar Fractures in Adults
Condylar fractures are rare in adults and typically involve the articular surface and the nonarticular portion of the distal humerus, including the epicondyle (Fig. 52-24). The status of the lateral trochlear ridge is the key to analyzing humeral condyle fractures. It may be involved with either medial or lateral condylar fractures and, when incorporated into the distal fragment, is far more likely to result in instability.
Pathophysiology.: Lateral condylar fractures are uncommon, although more common than fractures of the medial condyle. The mechanism of injury is either a direct blow to the lateral aspect of the flexed elbow or a force that results in adduction and hyperextension with avulsion of the lateral condyle. Medial condylar fractures are rare and result from either a direct blow to the apex of the flexed elbow or a fall on the outstretched arm with the elbow forced into varus.
Clinical and Radiographic Features.: The presentation of condylar fractures is similar to that of other distal humerus fractures, with swelling, tenderness, and crepitus localized over either the medial or the lateral elbow. On palpation, independent motion of the involved condyle may be appreciated. In lateral condylar fractures, findings may be accentuated with movement of the radius. On radiographic examination, lateral condylar fractures show a widening of the intercondylar distance. The distal fragment is often displaced, most commonly posteriorly and inferiorly. Because of the location of the ulnar nerve, it is imperative to test its function when this fracture is present. Medial condylar fractures are associated with tenderness over the medial condyle and pain with flexion of the wrist against resistance. On radiographic examination, displaced distal fragments tend to be anterior and inferior because of the pull of the forearm flexors.
Management.: Immediate treatment depends on radiographic findings. For undisplaced or minimally displaced condylar fractures, immobilization of the flexed elbow in a long arm posterior plaster splint is sufficient. For lateral condylar fractures, the forearm should be supinated and the wrist extended to relieve the tension on the extensor muscle attachments. For medial condylar fractures, the reverse is true (i.e., the forearm should be pronated and the wrist flexed). For fractures displaced more than 3 mm, surgical fixation is required.
Articular Surface Fractures
Pathophysiology.: Fractures of the capitellum and trochlea typically occur together, usually as a result of posterior dislocation of the elbow, with isolated fractures being rarer. Injury to the capitellum occurs when the patient falls on an outstretched hand, jamming the radial head upward, similar to the motion of a piston, shearing off the capitellum into the radial fossa. Because the capitellum has no muscular attachments, the fragment may remain nondisplaced. More often the fragment is displaced (usually anteriorly, but occasionally posteriorly). Because of this mechanism, a radial head fracture also may be present and should be clinically suspected.
Clinical and Radiographic Features.: The development of significant signs and symptoms may be delayed with capitellum fractures. Eventually, swelling within the capsule results in severe pain that manifests as well-localized tenderness on examination. Flexion of the elbow increases pain. A true lateral plain film usually shows the fragment lying anterior and proximal to the main portion of the capitellum (Fig. 52-25).

Figure 52-25 Fracture of the capitellum.
Management.: Treatment begins in the ED with a posterior splint, ice packs, elevation, compression, and analgesia. Accurate anatomic alignment, rigid internal fixation, and early mobilization are prerequisites for a good functional result.24 Fractures of the articular surfaces can be treated nonsurgically only if radiographs show perfect anatomic alignment.
Trochlea Fractures
Pathophysiology.: Isolated fractures of the trochlea are exceedingly rare because of the structure’s protected position deep within the elbow joint. The shearing force of the ulna against the trochlea is associated more commonly with posterior elbow dislocation.
Clinical Features.: The elbow is painful, with an effusion and limited range of motion because this is an intra-articular injury. On the radiograph a fragment is visible lying on the medial side of the joint, just distal to the medial epicondyle, and signs of joint effusion are visible. The fracture may extend into the distal portion of the medial epicondyle.
Management.: Nondisplaced fractures may be treated with a posterior splint for 3 weeks, followed by early range-of-motion exercises. Displaced fractures should be treated operatively; fragments that can be internally fixed are repaired, whereas small fragments are excised. Immobilization should be minimized to 10 to 14 days.25
Epicondyle Fractures
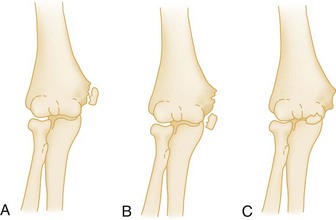
Most epicondylar fractures involve the medial epicondyle. Medial epicondyle fractures are most common in children and adolescents and often involve the apophysis, which is the last ossification center to fuse in the distal humerus, usually after age 15. Fractures through this ossification center usually occur in adolescence and constitute 11% of pediatric elbow fractures.26 These are not Salter-Harris injuries because the apophysis is involved rather than the physis. Because the lateral epicondyle is almost level with the flattened outer surface of the lateral condyle, it has only minimal exposure to a direct blow, and fracture is extremely rare.
Pathophysiology.: Medial epicondyle injuries occur from a variety of mechanisms. First, avulsion fractures are associated with posterior elbow dislocations in patients younger than 20 years in 30 to 55% of cases.27 Second, repetitive valgus stress (as with throwing a ball) results in eventual avulsion fracture of the epicondyle (Little Leaguer’s elbow). Another reported cause of fracture separation of the medial epicondyle, usually in adolescent boys, is arm wrestling.28 Violent muscular forces associated with a shifting center of gravity during this activity seem to produce an avulsion just before closure of the epiphyseal plate. Finally, a direct blow to the medial epicondyle can cause this injury.
Clinical and Radiographic Features.: The elbow is held in flexion, and any movement is resisted. Isolated fractures are associated with focal tenderness over the medial epicondyle. Use of the forearm flexors increases pain because their attachment is along the medial epicondyle. Ulnar nerve function should be evaluated. When the fracture is associated with a posterior dislocation, the examination reveals a prominent olecranon.
Simple fractures of the medial epicondyle are extra-articular injuries with limited soft tissue injury.20 They generally do not produce a fat pad sign on the lateral radiographic view of the elbow. A posterior fat pad or significant swelling of the joint should suggest concurrent injuries, such as elbow dislocation. Careful radiographic evaluation is especially important because fracture fragments may migrate into the joint space. If the fragment is overlying the joint line on radiographic examination, it should be considered intra-articular (Fig. 52-26). Radiographic detection of the intra-articular fragment is often difficult.27 Associated ulnar nerve palsy may be present with an entrapped fragment. Fragments may be difficult to see on radiographs, and a true anteroposterior view is difficult to obtain because of severe pain on extension. In an adolescent patient, there is a tendency to confuse the normal radiolucent epiphyseal growth plate with a fracture. In addition, minimally displaced fractures may be difficult to appreciate with radiographs. Comparison films of the uninjured elbow may be necessary. If dislocation is present, repeat radiographs taken after reduction should be evaluated for fragment location.
Management.: If the fracture fragment is minimally displaced (<5 mm), treatment with a posterior splint is appropriate. To minimize distraction of the fragment by the forearm flexors, the elbow and wrist are flexed with the forearm pronated.
Treatment of displaced fractures is controversial. In the past, the amount of displacement often dictated the need for surgery. Results of operative and nonoperative treatment seem to be good, however, regardless of the degree of displacement.29 Some experts advocate surgery for patients who participate in high-performance athletic activities that involve the injured extremity, but controlled studies are lacking.20 Intra-articular fragments that cannot be removed from the joint by manipulation are an indication for surgery.29 Immediate orthopedic consultation should be sought for these injuries. The rare lateral epicondylar fracture in adults was previously treated with immobilization, but more recent experience indicates that operative management is more successful.30
Little Leaguer’s Elbow
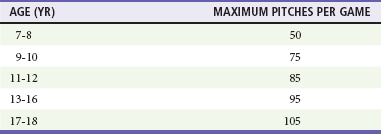
Little Leaguer’s elbow warrants special mention. An adolescent pitcher traumatizes immature epiphyses by repetitive throwing. Throwing the curve ball or breaking ball was previously implicated as a particular culprit, although the most important factor appears to be the total number of pitches per game.31 It has been shown in a group of highly competitive young baseball players that this injury is also common in catchers and fielders.32 The adolescent bone structure cannot withstand the extreme loading produced by repetitive hard throwing. Avulsion of the medial epicondyle or compression fracture of the subchondral bone of the lateral condyle or radial head may result (Fig. 52-27). This diagnosis should be sought in an athletic adolescent with medial epicondyle or radial head pain in the absence of acute injury by history. Adolescents with this condition should be forced to rest the elbow if throwing causes pain. After healing occurs, the amount of throwing and technique should be monitored carefully. The Committee on Sports Medicine and Fitness of the American Academy of Pediatrics and Little League Baseball recommend preventive measures to avoid these injuries, with guidelines for both pitch counts per game and mandated rest periods (Tables 52-2 and 52-3). The latest updates on new rules set forth by Little League Baseball can be found at www.littleleague.org.
Table 52-3
Little League Baseball Rest Requirements for Pitchers Age 16 and Older
| PITCHES | DAYS REST |
| 1-20 | 0 |
| 21-40 | 1 calendar day |
| 41-60 | 2 calendar days |
| >61 | 3 calendar days |
Olecranon Fractures
Pathophysiology.: Fractures of the olecranon may result from one of several mechanisms. Most commonly, a direct blow as a result of a fall, a motor vehicle or motorcycle crash, or an assault produces this injury. Such injuries are frequently comminuted. Less commonly, indirect force applied by forceful contraction of the triceps while the elbow is flexed during a fall can cause a transverse or oblique fracture through the olecranon. A combination of direct and indirect forces is believed also to cause some of these fractures. Olecranon fractures occur in adults and less commonly in children. The anatomic integrity of the olecranon is essential for triceps strength and normal function of the elbow, similar to the way intact patellar function is necessary for extension of the knee.
Clinical Features.: Physical findings may include tenderness and pain over the olecranon, a palpable separation at the fracture site, or the inability to extend the elbow against force. This last finding indicates complete discontinuity of the pulling mechanism and the consequent failure of triceps function. The neurovascular status should be examined, with special attention given to the ulnar nerve distribution, because this structure is most vulnerable to injury in this location. Loss of sensation over the palmar aspect of the fifth digit and hypothenar eminence or motor weakness in the interossei muscles of the hand suggests ulnar nerve injury.
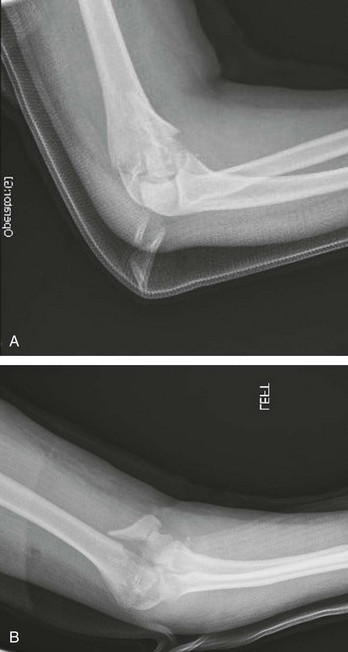
Diagnostic Strategies.: Lateral radiographic views are most helpful. In addition to the fracture, the degree of comminution, the extent of articular surface disruption, and the amount of displacement in the 90-degree flexion position should be noted. Nondisplacement in this position indicates that the triceps aponeurosis is intact, and prolonged immobilization is unnecessary. Displacement of more than 2 mm is considered an indication for surgery (Fig. 52-28A). A fracture line that increases in separation with flexion of the elbow also is considered a displaced fracture. When this fracture is associated with elbow dislocation, the plane of instability is located through the fracture site and the radiohumeral joint, resulting in posterior displacement of the proximal fragment of the ulna and anterior dislocation of the radius and ulna as a unit (Fig. 52-28B).
Management.: Undisplaced fractures can be treated conservatively on an outpatient basis with ice, compression, immobilization in 45 to 90 degrees of flexion, and analgesia. Follow-up films should be done at frequent intervals to ensure that subsequent displacement does not occur. Range-of-motion exercises can be started within 3 weeks in many cases.
Displaced fractures or fracture-dislocations require open reduction and internal fixation, and patients should be referred immediately to an orthopedic consultant. Displaced fractures in elderly patients sometimes are treated conservatively, but this should be left to the discretion of the consultant. Orthopedic referral also is necessary when ulnar nerve symptoms are present. These symptoms occur in 10% of patients, and in most cases the injury is an ulnar contusion that resolves spontaneously. The long-term outcome of treated olecranon fractures in adults is usually favorable with a low incidence of subsequent arthritis.32
Radial Head and Neck Fractures
Pathophysiology.: Radial head and neck fractures, in general, are produced by an indirect mechanism, typically a fall on an outstretched hand. The radius transmits the force upward, driving the radial head against the capitellum and resulting in fracture of the weaker radial head or neck. Although the fracture of the radial head may be the only radiographic finding, damage to the articular surface of the capitellum and injury to the collateral ligament commonly occur. Displacement of the radial head fragment suggests considerable force and significant soft tissue injury. This injury is characterized by localized tenderness over the radial head or pain with passive rotation of the forearm.
Diagnostic Strategies.: Radiographic findings range from a subtle disruption of the usual gradual sweep of the radial neck and head surface to an obvious displaced or comminuted fracture (Fig. 52-29). Undisplaced fractures are notoriously difficult to see on radiographs. Tenderness coupled with a positive fat pad sign on the radiograph indicate that the injury should be treated as a radial head fracture even in the absence of a visible fracture. Radial head fractures are classified into four types:

Figure 52-29 Radial head fracture with displacement.
Management.: Type I nondisplaced fractures are treated symptomatically with a brief period of sling support and early range-of-motion exercises (within 24-48 hours). Aspiration of the hemarthrosis and injection of 0.5% bupivacaine into the joint space may give dramatic relief of pain and improve the range of motion.35 However, a recent prospective randomized study found no benefit to bupivacaine instillation compared with simple aspiration.1 Most patients with this injury recover well in 2 to 3 months. A few do poorly, however, with long-term pain, contracture, or inflammation.
Type II injuries usually are treated similarly, with aspiration, instillation of bupivacaine, and immobilization in the ED, followed by a trial period of range-of-motion exercises. In these cases, aspiration of the joint and instillation of bupivacaine not only relieve pain but also allow testing of the range of motion to identify entrapped fragments. Radial head excision sometimes is performed later if the patient fails to improve. Early excision is advised for type II fractures when a mechanical block is present and for most type III fractures. Long-term functional results after radial head excision are acceptable in most patients, although a few have some functional disability after this procedure.34 Type IV injuries are treated for the elbow dislocation as described next and for the specific radial head lesion.
Dislocation and Subluxation
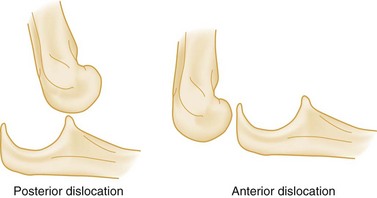
Because of its anatomic structure, the elbow is inherently subject to mechanical instability, and dislocations are common. The elbow is second only to the shoulder as the most commonly dislocated large joint. Elbow dislocation is a term usually used to describe a disruption of the relationship between the humerus and the olecranon. In general, the radius and ulna, bound together firmly by the annular ligament and interosseous membrane, displace as a unit. Most classifications refer to the abnormal position of the ulna relative to the humerus. The elbow most often dislocates posteriorly, although it may dislocate anteriorly, medially, or laterally (Fig. 52-30). A dislocation also may occur between the radius and ulna, and such dislocations rarely occur concurrently with the ulnohumeral type. The latter are termed divergent dislocations.
Posterior Elbow Dislocation
Pathophysiology.: The mechanism of injury is a fall on the outstretched hand or wrist, the elbow being either extended or hyperextended at the time of impact. A valgus stress usually also occurs. The resultant forces lever the ulna from the trochlea and produce the dislocation.
Clinical and Radiographic Features.: Patients hold the elbow in flexion at approximately 45 degrees and have marked prominence of the olecranon. Some elbow dislocations reduce before examination in the ED, presenting a confusing picture. In any case, significant diffuse tenderness and swelling are present. Neurovascular status is checked because brachial artery and median nerve injuries have been described. Neurovascular injury may occur from numerous mechanisms, including the initial traction, local swelling, and entrapment during reduction. Repeat examinations are mandatory.
A radiographic example of elbow dislocation before reduction is provided in Figure 52-31. Radiographic evaluation is crucial before manipulation to rule out fractures that can mimic dislocation on examination. Also, several fractures commonly occur in conjunction with dislocation, and these need to be identified and treated when present. These include fractures of the distal humerus, radial head, and coronoid process.
Management.: Orthopedic consultation is usually not necessary to proceed. Reduction should be attempted immediately, especially if there is neurovascular compromise. Intra-articular injection of local anesthetic may provide adequate analgesia to allow for closed reduction. Procedural sedation is very helpful and often required to facilitate reduction. Rarely is a regional block or general anesthesia needed. Posterior dislocations are reduced with an assistant immobilizing the humerus and applying countertraction while traction is applied to the distal forearm. The ideal position is for the elbow to be flexed at 30 degrees with the forearm supinated while distal traction is applied. When the capitellum slides over the coronoid process, a coupling sound occurs as the articular surfaces mesh. If reduction is unsuccessful with this technique, the physician should apply downward pressure at the proximal forearm and apply pressure behind the olecranon while maintaining in-line traction. This downward force may help “unlock” the coronoid process, which may be trapped in the olecranon fossa. The joint is gently moved through its normal range of motion to check stability. If stable, the elbow is flexed to approximately 90 degrees and immobilized with a posterior plaster mold. The neurovascular status should be rechecked. Postreduction radiographs are important to avoid missing concomitant fractures of the coronoid process or radial head or, in children, separation of the medial epicondylar apophysis.
Postreduction management includes immobilization in a posterior splint with the elbow in as much flexion as circulation allows. The arm is suspended in a sling. Circular casting should be avoided initially. Patients can be discharged with instructions to apply ice, elevate, and watch for signs of vascular impairment. Patients should not be discharged until and unless they can follow such instructions. If the elbow is stable after reduction, gentle range-of-motion exercises may be initiated in 3 to 5 days. Unstable joints may require either prolonged immobilization in the presence of ligamentous instability or internal fixation for instability associated with fracture.36
Complications.: The most serious complication of elbow dislocation is vascular compromise. Severe disruption results in injury to the brachial artery in 5 to 13% of cases.37 Vascular injury should be sought when a wide opening between the tip of the olecranon and the distal humerus is palpated or seen on a radiograph. The presence of distal pulses is not proof of an intact artery, and if a question of vascular compromise exists, emergent vascular studies or consultation is indicated. Median nerve traction injuries and entrapment also have been reported. Loss of median nerve function after reduction should prompt immediate orthopedic consultation. Recurrent dislocation of the elbow is rare.
Anterior Elbow Dislocation
Pathophysiology.: Anterior dislocations are rare and occur as a result of a blow from behind to the olecranon while the elbow is in the flexed position. Severe associated soft tissue trauma is present, including avulsion of the triceps mechanism or vascular disruption. These dislocations are frequently open.
Clinical Features.: The upper arm appears shortened and the forearm elongated. The elbow is fully extended, and the forearm is supinated. The olecranon fossa is palpable posteriorly.
Management.: Reduction of closed injuries is performed with distal traction of the wrist and a backward pressure on the forearm while the distal humerus is grasped. A click usually indicates that reduction has been achieved. These injuries have a higher incidence of vascular impairment than the more common posterior dislocation, but ulnar nerve injuries are unusual.38 Emergent orthopedic referral is advised and is mandatory for open injuries or when vascular disruption is suggested.
Radial Head Subluxation
Subluxation of the radial head is a common injury, representing more than 20% of upper extremity injuries in children. Children aged 1 to 4 years are most often affected, although cases have been reported in children 6 months to 15 years of age. Girls are affected more commonly than boys, and the left arm is more commonly affected than the right.39 This injury is called nursemaid‘s elbow because it results from a sudden longitudinal pull on the forearm while the child’s arm is in pronation. Stretching of the annular ligament allows fibers to slip between the capitellum and the head of the radius, resulting in an inability of the child to supinate the arm. By the age of 5, the annular ligament becomes thick and strong and thus is far less likely to tear or be displaced.
Clinical and Radiographic Features
The classic history, present approximately half of the time,40 is that of the forearm being pulled while in pronation with the elbow extended. Other mechanisms include direct trauma to the elbow or a twisting motion of the arm. In children younger than 6 months, the mechanism of subluxation involves rolling over in bed, which may trap the involved forearm under the body with resulting longitudinal traction on the joint. Clinically, the arm is held in passive pronation, with slight flexion at the elbow. The child is unable or unwilling to move the arm. Resistance to supination and tenderness on direct palpation over the head of the radius are present. Swelling, ecchymosis, and deformity are absent. Examination should include inspection and palpation of the entire extremity, including the clavicle.
Management
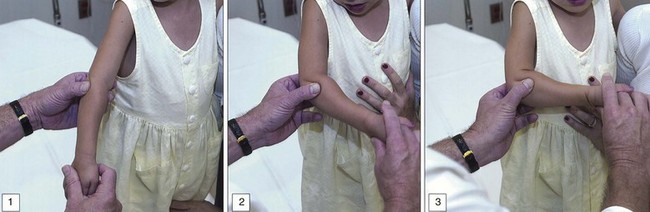
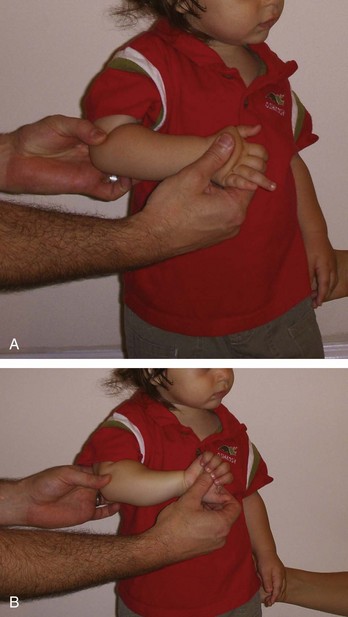
Reduction may be attempted in children with typical presentations and is safe even when the classic history is absent. Supination-flexion is the method most commonly used in the past. Reduction is achieved by supination of the forearm while slight pressure on the radial head is applied with the examiner’s thumb. In one continuous motion, the elbow is supinated and flexed with gentle traction applied. A click often, but not always, is felt as the radial head reduces (Fig. 52-32). A second technique of reduction, hyperpronation, has a significantly higher reported success rate of reduction on the first attempt.41 With the hyperpronation method, the child’s elbow is supported with moderate pressure applied to the radial head. The examiner then grips the child’s distal forearm and hyperpronates the forearm, resulting in a click felt over the radial head (Fig. 52-33).
Many patients are asymptomatic within 5 to 10 minutes; 90% of patients regain use of the arm within 30 minutes. Hearing or palpating a click is associated with success. It is a good idea for the physician to leave the room and for parents to distract the child to show return of normal function. A fearful child often does not use even the successfully reduced limb. If function does not return within 24 hours, the patient should be reevaluated. After successful reduction, no additional treatment, immobilization, or activity reduction is necessary. Parents and caregivers should be instructed to avoid excessive traction on the child’s forearm to prevent recurrent radial head subluxation. The recurrent radial head subluxation rate is approximately 20%.42 Most of these injuries are unintentional on the part of the caregiver, but inflicted injury should be considered in suggestive cases.
Soft Tissue Disorders
Pathophysiology
Tennis elbow is a term first introduced in the 1880s to describe an inflammatory process that involves the radiohumeral joint or lateral epicondyle of the humerus. It is a common exercise-related syndrome, and the mechanism is thought to be repetitive pronation and supination of the forearm. The actual pathologic nature of this syndrome is unclear. Radiohumeral bursitis or synovitis, tendinitis of the common extensor tendon, periostitis of the lateral epicondyle, and entrapment by scar tissue of the radial nerve all have been suggested as culprits in this syndrome. Histologically, the abnormality has been described as angiofibroblastic hyperplasia, a term subsequently modified to angiofibroblastic tendinosis. The cause has been theorized to be a degenerative process because of the paucity of acute inflammatory cells seen histologically.43 Medial tennis elbow and posterior tennis elbow have been reported, the former involving the pronator teres and flexor carpi radialis insertions and the latter involving the triceps tendon. The following discussion pertains to lateral tennis elbow.
Management
Traditional treatment includes protection, rest, ice, compression, elevation, and medication. Initial therapy includes avoidance of the inciting activity and immobilization with a sling. Nonsteroidal anti-inflammatory drugs are often used, but their efficacy probably is limited to their analgesic rather than their anti-inflammatory properties. Injection of a corticosteroid at the point of tenderness provides some pain relief in most patients.43,44 Because corticosteroids weaken collagen, premature resumption of heavy loading of the tendon at the lesion should be avoided, as should injection directly into the tendon. Patients with pain that persists despite treatment and a rehabilitation program should be referred for possible surgery.45 Modification of athletic technique is recommended after the symptoms subside.
Biceps Tendon Rupture
Biceps tendon rupture occurs most commonly in the proximal portion of the long head of the biceps. It is most common in middle-aged athletes or physical laborers who sustain repetitive microtrauma to the tendon. Patients experience a snapping sound and pain in the anterior shoulder during strenuous activities that produce rapid loading of the muscle. Rupture also occurs distally, usually as an avulsion from the insertion on the radial tuberosity, although ruptures at the musculotendinous junction occasionally occur. Rupture of the distal biceps tendon occurs almost exclusively in men, most commonly between the ages of 40 and 60, and most often involves the dominant arm.46–47 The inciting event is usually an unexpected extension force applied to the arm flexed at 90 degrees. The pathophysiology of tendon rupture is poorly understood, although tendon rupture generally occurs in the setting of underlying tendinosis. Biceps tendon tears are becoming more common in players in the National Football League (NFL), most commonly in offensive linemen.48 Diabetes, chronic renal failure, systemic lupus erythematosus, rheumatoid arthritis, and steroid or fluoroquinolone therapy all may result in tendinosis. Smoking has been shown to be strongly associated with distal biceps tendon rupture.49
References
1. Paraskevas, G, et al. Study of the carrying angle of the human elbow joint in full extension: A morphometric analysis. Surg Radiol Anat. 2004;26:19.
2. Silva, M, et al. Inter- and intra-observer reliability of the Baumann angle of the humerus in children with supracondylar humeral fractures. Int Orthop. 2010;34:553–557.
3. Chen, FS, Diaz, VA, Loebenberg, M, Rosen, JE. Shoulder and elbow injuries in the skeletally immature athlete. J Am Acad Orthop Surg. 2005;13:172.
4. Shao, YC, Harwood, P, Grotz, MR, Limb, D, Giannoudis, PV. Radial nerve palsy associated with fractures of the shaft of the humerus: A systematic review. J Bone Joint Surg Br. 2005;87:1647–1652.
5. Hobgood, ER, Khan, SO, Field, LD. Acute dislocations of the elbow. Hand Clin. 2008;24:10.
6. Beaty, JA, Kasser, JR. The elbow region: General concepts in the pediatric patient. In: Beaty JA, Kasser JR, eds. Rockwood and Wilkins’ Fractures in Children. 5th ed. Philadelphia: Lippincott, Williams and Wilkins; 2005:563–576.
7. Ilyas, AM, Jupiter, JB. Treatment of distal humerus fractures. Acta Chir Orthop Traumatol Cech. 2008;75:6.
8. Gadgil, A, Hayhurst, C, Maffulli, N, Dwyer, JS. Elevated-straight arm traction for supracondylar fractures of the humerus in children. J Bone Joint Surg Br. 2005;87:82.
9. Pollock, JW, Faber, KJ, Athwal, GS. Distal humerus fractures. Orthop Clin North Am. 2008;39:187.
10. Omid, R, Choi, PD, Skaggs, DL. Supracondylar humeral fractures in children. J Bone Joint Sur Am. 2008;90:1121.
11. Slongo, T, Schmid, T, Wilkins, K, Joeris, A. Lateral external fixation—a new surgical technique for displaced unreducible supracondylar humeral fractures in children. J Bone Joint Surg Am. 2008;90:1690.
12. Skaggs, DL, et al. Operative treatment of supracondylar fractures of the humerus in children: The consequences of pin placement. J Bone Joint Surg Am. 2001;83:735.
13. Weiland, AJ, Meyer, S, Tolo, VT, Berg, HL, Mueller, J. Surgical treatment of displaced supracondylar fractures of the humerus in children. Analysis of fifty-two cases followed for five to fifteen years. J Bone Joint Surg Am. 1978;60:657.
14. Hodge, D, 3rd., Gregg, J, Christofersen, M, Wong, J. Trauma to elbows, knees, and ankles. Pediatr Emerg Care. 1991;7:188.
15. Ramachandran, M, Birch, R, Eastwood, DM. Clinical outcome of nerve injuries associated with supracondylar fractures of the humerus in children. J Bone Joint Surg Br. 2006;88:90.
16. Wong, AS, Baratz, ME. Elbow fractures: Distal humerus. J Hand Surg Am. 2009;34:176–190.
17. Gupta, R, Khanchandrani, P. Intercondylar fractures of the distal humerus in adults: A critical review of 55 cases. Injury. 2002;33:511.
18. Robinson, CM, Hill, RM, Jacobs, N, Dall, G, Court-Brown, CM. Adult distal humeral metaphyseal fractures: Epidemiology and results of treatment. J Orthop Trauma. 2003;17:38–47.
19. Ring, D. Elbow fractures and dislocations. In Bucholz RW, et al, eds.: Rockwood and Greene’s Fractures in Adults, 7th ed, Philadelphia: Lippincott, Williams, and Wilkins, 2010.
20. Kramer, DE. Elbow pain and injury in young athletes. J Pediatr Orthop. 2010;30:S7.
21. Shrader, MW. Pediatric supracondylar fractures and pediatric physeal elbow fractures. Orthop Clin North Am. 2008;39:163.
22. Weiss, JM, et al. A new classification system predictive of complications in surgically-treated pediatric humeral lateral condyle fractures. J Pediatr Orthop. 2009;29:602–605.
23. Leet, AI, Young, C, Hoffer, M. Medial condyle fractures of the humerus in children. J Pediatr Orthop. 2002;22:2.
24. Dubberley, JH, Faber, KJ, Macdermid, JC, Patterson, SD, King, GJ. Outcome after open reduction and internal fixation of capitellar and trochlear fractures. J Bone Joint Surg Am. 2006;88:46.
25. Faber, KJ. Coronal shear fractures of the distal humerus: The capitellum and trochlea. Hand Clin. 2004;20:455–464.
26. Farsetti, P, Potenza, V, Caterini, R, Ippolito, E. Long-term results of treatment of fractures of the medial humeral epicondyle in children. J Bone Joint Surg Am. 2001;83:1299.
27. Louahem, DM, et al. Displaced medial epicondyle fractures of the humerus: Surgical treatment and results. A report of 139 cases. Arch Orthop Trauma Surg. 2010;130:649–655.
28. Khashaba, A. Broken arm wrestler. Br J Sports Med. 2000;34:461–462.
29. Micheli, LJ, Luke, AC, Mintzer, CM, Waters, PM. Elbow arthroscopy in the pediatric and adolescent population. Arthroscopy. 2001;17:694.
30. Ring, D, Jupiter, J, Gulotta, L. Articular fractures of the distal part of the humerus. J Bone Joint Surg Am. 2003;85:232–238.
31. Olsen, SJ, 2nd., Fleisig, GS, Dun, S, Loftice, J, Andrews, JR. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34:905.
32. Hang, DW, Chao, CM, Hang, YS. A clinical and roentgenographic study of Little League elbow. Am J Sports Med. 2004;32:79.
33. Kaas, L, et al. Management of radial head fractures: Current concepts. J Shoulder Elbow Surg. 2011;3:34–40.
34. Karlsson, MK, Hasserius, R, Karlsson, C, Besjakov, J, Josefsson, PO. Fractures of the olecranon: A 15- to 25-year followup of 73 patients. Clin Orthop Relat Res. 2002;403:205.
35. Chalidis, BE, Papadopoulos, PP, Sachinis, NC, Dimitriou, CG. Aspiration alone versus aspiration and bupivacaine injection in the treatment of undisplaced radial head fractures: A prospective randomized study. J Shoulder Elbow Surg. 2009;18:676–679.
36. Karlsson, MK, et al. Comminuted fractures of the radial head. Acta Orthop. 2010;81:224–227.
37. Phillips, CS, Segalman, KA. Diagnosis and treatment of post-traumatic medial and lateral elbow ligament incompetence. Hand Clin. 2002;18:149.
38. Carter, SJ, Germann, CA, Dacus, AA, Sweeney, TW, Perron, AD. Orthopedic pitfalls in the ED: Neurovascular injury associated with posterior elbow dislocations. Am J Emerg Med. 2009;28:960–965.
39. Carson, S, Woolridge, DP, Colletti, J, Kilgore, K. Pediatric upper extremity injuries. Pediatr Clin North Am. 2006;53:41.
40. Chasm, RM, Swencki, SA. Pediatric orthopedic emergencies. Emerg Med Clin North Am. 2010;28:907.
41. Bek, D, Yildiz, C, Köse, O, Sehirlio lu, A, Ba
lu, A, Ba bozkurt, M. Pronation versus supination maneuvers for the reduction of ‘pulled elbow’: A randomized clinical trial. Eur J Emerg Med. 2009;16:135–138.
bozkurt, M. Pronation versus supination maneuvers for the reduction of ‘pulled elbow’: A randomized clinical trial. Eur J Emerg Med. 2009;16:135–138.
42. Kim, MC, Eckhardt, BP, Craig, C, Kuhns, LR. Ultrasonography of the annular ligament partial tear and recurrent “pulled elbow”. Pediatr Radiol. 2004;34:999–1004.
43. Van Hofwegen, C, Baker, CL, 3rd., Baker, CL, Jr. Epicondylitis in the athlete’s elbow. Clin Sports Med. 2010;29:577–597.
44. Rinner, CA, Ruch, DS. Elbow tendinopathy and tendon ruptures: Epicondylitis. J Hand Surg. 2009;34:566.
45. Hay, EM, Paterson, SM, Lewis, M, Hosie, G, Croft, P. Pragmatic randomised controlled trial of local corticosteroid injection and naproxen for treatment of lateral epicondylitis of elbow in primary care. BMJ. 1999;319:964.
46. Mariscalco, MW, Saluan, P. Upper extremity injuries in the adolescent athlete. Sports Med Athrosc. 2011;19:17.
47. Sutton, KM, Dodds, SD, Ahmad, CS, Sethi, PM. Surgical treatment of distal biceps rupture. J Acad Orthop Surg. 2010;18:139–148.
48. Anderson R: Biceps tendon rupture in NFL athletes. Presented to the NFL Physicians Society National Meeting, Indianapolis, Ind, February 25, 2011.
49. Safran, M, Graham, SM. Distal biceps tendon ruptures: Incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;404:275.