Chapter 30 Human sexuality
HUMAN SEXUAL RESPONSE
Care needs to be taken to not see these phases as directional, assuming orgasm to be the goal.
SEXUAL DYSFUNCTIONS
Women have four main sexual dysfunctions:
Table 30.1 lists the sexual dysfunctions that occur in men and women. The approximate prevalences of these disorders are given in Table 30.2.
| Clinical Syndrome | ||
|---|---|---|
| Male | Female | |
| Inhibited sexual desire | No arousal | No arousal |
| Fear of sexual (genital) activity | Primary erectile failure (impotence) | Vaginismus |
|
Absence or inadequate vasocongestion* due to failure to respond to erotic stimulation because of anxiety, guilt, or fear of injury
|
Reduced libido and secondary erectile failure (impotence) | Reduced libido |
| Impairment or failure of orgasm. Extremely rapid, or absence of clonic rhythmic contractions of pelvic musculature due to inhibition of genital tactile or psychic erotic stimulation | Premature ejaculation Restricted ejaculation | Orgastic dysfunction |
* In the male, penile erection; in the female, vaginal lubrication and perivaginal swelling.
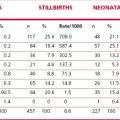
Table 30.2 Prevalence of sexual disorders in the community*
| Females (%) | Males (%) | |
|---|---|---|
| Inhibited sexual desire | up to 30 | 10–15 |
| Impairment of sexual arousal | 10–20 | 10–20 |
| Failure to achieve orgasm | 10–20 | |
| Premature ejaculation | 20–30 | |
| Dyspareunia | 10–15 | |
| Vaginismus | 1–3 | |
| Total sexual dysfunction | 30–50 | 20–45 |
| Total sexual dysfunction causing distress | 9–15 |
* Figures depend on age, presence of partner, medical, psychological and psychiatric status of the community studied.