3 Human immune deficiency virus and AIDS
Introduction
Pathogenesis
Disease manifestations of hiv infection
These can be due to HIV itself, to the treatment of HIV and lastly to immunosuppression, which leads to opportunistic infections (p. 111) and cancer (p. 117).
HIV infection
HIV-associated nephropathy (HIVAN)
HIV-associated dementia
Manifestations due to treatment of HIV
Mitochondrial toxicity and lactic acidosis
Approach to the Patient
Initial diagnosis
In patients with undetermined/negative HIV serology, the diagnosis of an acute infection is by demonstrating a high viral load or a positive p. 24 antigen (which disappears after 8 weeks of infection).
Investigations and monitoring
Initial assessment
All clinicians should be of the competence necessary to obtain consent for an HIV test. The British HIV Association provides a list of associated presenting conditions for which an HIV test may be indicated (http://www.bhiva.org/cms1222621.asp). Many patients are diagnosed when they present themselves to a sexual health clinic.
Box 3.1
(Based on British HIV Association guidelines 2008)
Baseline investigations in a newly diagnosed asymptomatic patient with HIV infection
A full examination, including fundoscopy, neurological examination and palpation of all lymph node groups, is carried out.
CD4 count
The viral load
Genotyping
highly active anti-retroviral therapy (haart)
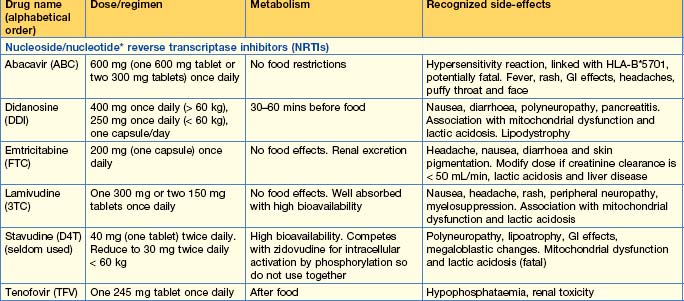
Available anti-retroviral medications, along with their side-effects, are shown in Table 3.1.
Available drugs
Nucleoside reverse transcriptase inhibitors (NRTIs)
Nucleotide reverse transcriptase inhibitors
Non-nucleoside/nucleotide reverse transcriptase inhibitors (NNRTIs)
Protease inhibitors (PIs)
Fusion inhibitors
Indications for anti-retroviral therapy
Symptomatic HIV infection
Asymptomatic HIV infection
Starting therapy
Adherence
• Patient factors include
Choice of drugs (Table 3.1)
The drug regimen used for starting therapy must be individualized to suit each patient’s needs.
Opportunistic infection in the haart era
Fungal infection
Candidiasis
Cryptococcosis
Histoplasmosis
Pneumocystis infection
Protozoal infection
Toxoplasmosis
Viral infection
Cytomegalovirus (CMV)
JC virus
The JC virus is a papova virus that can lead to progressive multifocal leucoencephalopathy (PML). It is seen in patients with CD4 counts < 100. Presentation is with cognitive impairment and confusion, but focal neurological signs are detectable in most patients on presentation. White matter disease, with non-enhancing high-signal lesions seen on T2-weighted MRI, is the classical radiological finding. JC virus can be detected in CSF by PCR techniques. Brain biopsy is the only definitive diagnostic procedure. The only specific treatment available is cidofovir, but data are inconclusive on its efficacy. Immune reconstitution is associated with improved survival but, despite this, PML remains a life-threatening condition with a poor prognosis.
Hepatitis B virus (HBV)
Bacterial infection
Mycobacterium TB
HIV-related malignancies
Primary CNS lymphoma
Barnett T, Whiteside A. AIDS in the Twenty-First Century, Disease and Globalisation, ed 2. London: Palgrave; 2006.
Chadwick DR, Geretti AM. Immunization of the HIV infected traveler. AIDS. 2007;21:787-794.
Dolin R. A new class of anti-HIV therapy. New Engl J Med. 2008;359:1509-1511.
Palella FJJr, Baker RK, Moorman AC, et al. Mortality in the highly active antiretroviral therapy era: changing causes of death and disease in the HIV outpatient study. J Acquir Immune Defic Syndr. 2006;43(1):27-34.
Simoni JM, Pearson CR, Pantalone DW, et al. Efficacy of interventions in improving highly active antiretroviral therapy adherence and HIV-1 RNA viral load. A meta-analytic review of randomized controlled trials. J Acquir Immune Defic Syndr. 2006;43(Suppl 1):S23-S35.
Taylor BS, Carr JK, Salminen MO, et al. The challenge of HIV-1 subtype diversity. New Engl J Med. 2008;358:1590-1603.
Young T, Arens F, Kennedy G, et al: Antiretroviral post-exposure prophylaxis (PEP) for occupational HIV exposure. Cochrane Database Syst Rev 21(1):CD002835 2007(1), 2007.
http://bashh.org. British Association for Sexual Health and HIV
www.bhiva.org. British HIV Association (BHIVA)
www.i-base.info/. HIV i-Base. HIV treatment information
www.aidsmap.com/. National AIDS Manual. Aidsmap information on HIV and AIDS
www.hiv-druginteractions.org/. University of Liverpool. HIV drug interactions
http://hivdb.stanford.edu/. University of Stanford. HIV Drug Resistance Database
http://www.aidsinfo.nih.gov/guidelines/. US Department of Health and Human Services. Clinical Guidelines Portal