Home Respiratory Care and Mechanical Ventilation
I Overall Goals of Home Respiratory Care
C Reduce morbidity associated with disease
D Arrest the progress of chronic diseases
E Improve overall physiologic and psychological function
F Provide an environment to enhance individual potential
II Home Care Coverage: Financial Considerations
A Federal programs such as Medicare Part B DME provision, Veterans Administration, Social Service Block Grants, or Medicare Hospice
B State programs such as Medicaid
C Local community organizations and chapter affiliates of large organizations such as American Cancer Society, National Easter Seal Society, Amyotrophic Lateral Sclerosis Association
D Private third-party payers, which include commercial health insurance companies, health maintenance organizations (HMOs), managed care organizations (MCOs), participating provider organizations (PPOs), and worker’s compensation
E Payment directly by patient and/or family, which may satisfy deductible, copayment, or total payment for uninsured or uncovered services
III Primary Forms of Home Respiratory Care
A Indication: Any cardiopulmonary disease resulting in significant, chronic hypoxemia in the patient’s chronic stable state.
B Chronic hypoxemia in the home care setting is defined by Health Care Financing Administration (HCFA) reimbursement criteria and is scientifically supported by the Nocturnal Oxygen Therapy Trial (NOTT study) and the British Medical Research Council Working Party study.
C Reimbursement criteria include each of the following
2. PO2: 56 to 59 mm Hg (group II) with
a. Dependent edema suggestive of congestive heart failure
b. Pulmonary hypertension or cor pulmonale determined by measurement of the pulmonary artery pressure, gated blood pool scan/echocardiogram, or “P” pulmonale on the electrocardiogram (ECG), or
3. Hemoglobin saturation: ≤88% (group I)
4. Hemoglobin saturation: 89% (group II), and
a. Dependent edema suggestive of congestive heart failure
b. Pulmonary hypertension or cor pulmonale determined by measurement of the pulmonary artery pressure, gated blood pool scan/echocardiogram, or “P’ pulmonale on the ECG, or
5. Criteria for activity-based oxygen desaturation
a. PO2 of ≤55 mm Hg or hemoglobin saturation of ≤88%
b. Taken during activity for a patient who demonstrates an arterial PO2 of ≥56 mm Hg or an arterial oxygen saturation of ≥89% during the day while at rest
c. In this case supplemental oxygen is provided for use during exercise if it is documented that the use of oxygen improves the hypoxemia that was demonstrated during exercise when the patient was breathing room air.
6. Criteria for sleep-induced oxygen desaturation
a. PO2 of ≤55 mm Hg or an arterial saturation of ≤88% taken during sleep for a patient who demonstrates an arterial PO2 of ≥56 mm Hg or an arterial oxygen saturation of ≥89% while awake, or
b. A greater than normal decrease in oxygen level during sleep (a decrease in arterial PO2 >10 mm Hg or a decrease in arterial oxygen saturation >5%) associated with “P” pulmonale on ECG, documented pulmonary hypertension, and erythrocytosis.
c. In either of these cases coverage is provided only for nocturnal use of oxygen.
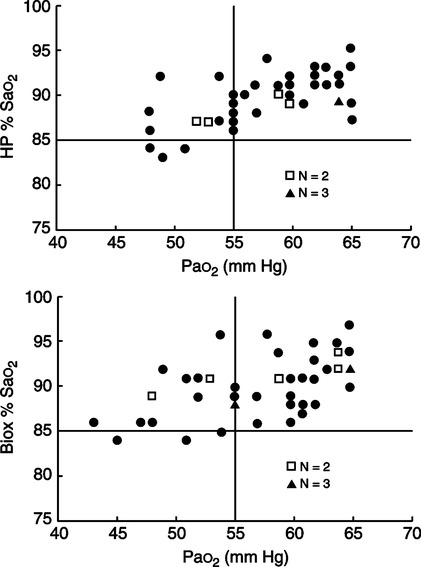
D Because the relationship between PO2 and hemoglobin saturation is variable and affected by a number of factors, criteria for home oxygen therapy generally should be based on PO2, not on HbO2%, as depicted in Figure 32-1, where some nonqualifying HbO2% are a result of qualifying PO2.
E Physiologic effects of long-term oxygen therapy
1. Increased exercise capacity
2. Decreased work of the myocardium
3. Decreased work of breathing
4. Decreased pulmonary hypertension
5. Normalization of the hemoglobin level
F Oxygen containment systems used in the home (see Chapter 34 for details)
1. System choice is commonly based more on cost versus reimbursement issues than on clinical efficacy; nonetheless the system chosen for a specific patient should satisfy the domicilary and mobility needs. Each system has major advantages and disadvantages (Table 32-1).
TABLE 32-1
Advantages Versus Disadvantages of Various Oxygen Delivery Systems
| Advantages | Disadvantages | |
| Cylinder oxygen | Fixed finite source of oxygen | Heavy/bulky |
| May be stored indefinitely | Represents the smallest content | |
| Large liter flows transiently available | Requires frequent redeliveries | |
| 100% oxygen source | High pressure 2000-3000 psi | |
| Quiet oxygen delivery | Represents weight and high-pressure danger | |
| Liquid oxygen | Patient can transfill portable | Evaporation/flash loss |
| Large content 860 times compressed | Requires frequent redeliveries | |
| Liter flow limited to 8-10 L/min | May freeze, interrupting O2 flow indefinitely | |
| Low pressure <20 psi | Represents thermal hazard | |
| 100% oxygen source | Requires backup cylinder O2 | |
| Quiet oxygen delivery | ||
| Concentrator oxygen | Infinite source of oxygen | Consumes patient electricity |
| Simplicity of operation | Noisy | |
| Least supplier intrusion | Potential of mechanical failure | |
| Requires patient/supplier maintenance | ||
| Liter flow limited to 5-6 L/min | ||
| Requires backup cylinder O2 | ||
| 85-98% O2 dependent on liter flow | ||
| Represents electric shock hazard |
2. Oxygen concentrators are most commonly used when the patient is essentially homebound for the majority of time. This system provides an infinite amount of oxygen supply with proper maintenance. However, being electrically powered, concentrators should have a backup source of oxygen for power and/or equipment failures. Oxygen cylinders typically provide backup oxygen in the amount to cover three times the supplier’s average response time. With the concentrator there exists the additional cost of electricity, which is incurred by the patient and can be substantial. Specialty concentrators are manufactured that allow the user to slowly transfill aluminum portable cylinders. Portable concentrators with internal battery power and integral oxygen conservers also have recently been introduced. Further a single manufacturer has brought a concentrator capable of delivering 10 L/min to market.
3. Liquid oxygen systems are especially useful for travel, work, and patients with consistent out-of-the-home mobility needs. Liquid oxygen systems represent a large finite source of oxygen with features allowing patient transfilling of portable units. Liquid oxygen units should have a backup source of oxygen for equipment failures or complete depletion of the liquid oxygen contents. Oxygen cylinders typically provide backup oxygen in the amount to cover three times the supplier’s average response time. This finite source of oxygen, which is continuously being consumed, requires weekly (or more often) replenishment by the oxygen supplier.
4. Oxygen cylinders are the least commonly used, are the most labor intensive, and are the most expensive. However, cylinders represent a small finite source of oxygen that can be stored indefinitely, hence making them ideal backup sources of oxygen for the home care patient. Smaller cylinders are commonly used to satisfy the periodic mobility needs of patients using an oxygen concentrator for their primary oxygen source. Cylinders made of composite light-weight resin material that may be filled to 150% the normal filling pressure (3000 psi) are available and represent a significant increase in duration and portability (Table 32-2).
TABLE 32-2
Comparison of Available Portable Oxygen Delivery Systems
| Portable Device | Weight | Gas Contents | Duration† |
| Aluminum M-6 or “B” cylinder* | 2.2 lb | 164 L | 42 min |
| Aluminum M-9 or “C” cylinder* | 3.7 lb | 255 L | 2 hr 7 min |
| Aluminum M-15 or “D” cylinder* | 5.3 lb | 425 L | 3 hr 30 min |
| Aluminum M-22 or “E” cylinder* | 7.9 lb | 680 L | 5 hr 40 min |
| Composite 3000 psi M-9 “B” cylinder size* | 1.7 lb | 246 L | 2 hr 3 min |
| Composite 3000 psi M-15 “C” cylinder size* | 2.6 lb | 410 L | 3 hr 23 min |
| Composite 3000 psi M-22 “D” cylinder size* | 3.2 lb | 640 L | 5 hr 20 min |
| Small representative LOX portable | 5.5 lb | 542 L | 4 hr 31 min |
| Large representative LOX portable | 8.5 lb | 1058 L | 8 hr 50 min |
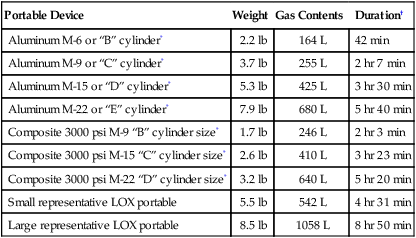
*Require cylinder valve stem and regulator weighing 1.75 lb.
5. Some patients use a combination of oxygen concentrator for their stationary oxygen source and a portable liquid oxygen unit (transfilled from a stationary liquid oxygen reservoir) for their portable oxygen needs. Note that third-party payers will only pay for one stationary oxygen source under most circumstances.
G Oxygen therapy equipment (see Chapter 34)
1. The simple cannula is most common; however, smaller-sized, low-flow cannulas have been used by long-term users of oxygen because of their comfort and inconspicuous appearance. Such cannulas are reserved for liter flows of ≤2 L/min.
2. The simple cannula is usually supplemented with a 25- to 50-foot oxygen extension to provide mobility from the stationary oxygen source. The 50-foot extension is the longest recommended by oxygen equipment manufacturers.
3. Oxygen-conserving devices are used for normal mobility, long-distance travel, or high oxygen demand.
a. Oxygen reservoir systems function by increasing the anatomic reservoir available for oxygen accumulation.
b. Pulse dose or demand systems deliver a predetermined dose of oxygen at the initial portion of inspiration on every- or multiple-breath variations. Such devices are either independent or integral to the oxygen equipment.
(1) Independent devices are commonly electronically controlled sensors or fluidic switches that are connected in series between the patient and the oxygen source. These may be used with a variety of portable or stationary oxygen sources (e.g., cylinders or liquid oxygen units).
(2) Integral devices are incorporated directly by the oxygen manufacturer and are typically found on small liquid oxygen portable units that provide for extraordinarily small size and light weight without compromise in duration of oxygen provision.
c. Transtracheal oxygen is useful in continued work or other activities away from home or for those with hypoxemia refractory to conventional home oxygen system limits.
H Monitoring home oxygen therapy
1. Patients who meet the criteria for oxygen therapy at discharge frequently do not require oxygen after a few months as a result of
2. Monthly monitoring of status should occur in the home.
a. Pulse oximetry: After the need is established with PO2 criteria, HbO2% is concurrently determined with and without oxygen to establish an HbO2% baseline. Oximetry should also be performed with the patient performing the most strenuous activity of his or her normal day to ensure adequacy of the oxygen prescription. These data are to be used as the baseline for future home monitoring.
b. Sequential monitoring of HbO2% will provide screening for need to assess PO2 by arterial blood gas.
c. Adequacy of PO2 coupled with medical optimization should guide the physician’s decision to maintain or discontinue home oxygen.
3. Office follow-up evaluation: Frequency depends on the severity of the overall disease process.
I Complications/safety considerations
1. Fire hazard is increased in the presence of increased concentrations of oxygen. Generally oxygen should be kept a minimum of 5 feet away from any source of spark and/or flame.
2. Unsecured cylinders present a physical hazard, as does thermal (cold) burn from mishandling liquid oxygen and electric shock from ungrounded oxygen concentrators.
3. Fall secondary to oxygen extension tubing clutter.
4. Complications may occur from the oxygen appliance (e.g., cannula or transtracheal device).
A Patients with an intact airway and thick, tenacious secretions (e.g., cystic fibrosis, bronchiectasis) may require intermittent administration of aerosol therapy via pneumatic nebulizer.
B Patients with permanent artificial airways
1. Most patients are capable of acclimating to artificial airways without the need for continuous aerosol therapy other than the use of artificial noses or heat and moisture exchangers.
2. Many require nocturnal aerosol therapy. Whether heated or unheated, with or without oxygen, depends on the patient’s medical status and tolerance. Note that use of oxygen as a convenient vehicle of aerosol delivery, as is commonly used in the hospital setting, is normally not done in the home care setting. This is a result of home care equipment limitations and third-party payer (reimbursement) constraints.
3. Occasionally the direct instillation of 3 to 5 ml of sterile 0.9% NaCl into the tracheostomy tube on an intermittent or before suction basis is used to thin secretions and/or induce cough.
4. Systemic hydration remains the cornerstone of maintaining normal viscosity of pulmonary secretions.
C Small-volume aerosolized drug therapy (see Chapters 17 and 35) is typically delivered via metered dose inhaler (MDI) or small volume nebulizers (SVNs) with a compressor.
1. Many nontracheostomized, nonmechanically ventilated patients are capable of coordinating the use of an MDI with a spacer, and delivery of medication is best served in that fashion for convenience and cost.
2. However, in those who have psychomotor and/or cognitive impairments precluding the coordinated ventilatory act required of the MDI, the use of pneumatically operated SVNs is warranted. Young pediatric patients unable to grasp verbal instruction also commonly use such devices. These devices are typically AC powered, but variations with rechargeable self-contained batteries and/or cigarette lighter adapters are manufactured.
3. Most common drugs delivered by aerosol in the home include
D Complications/safety considerations
1. Aerosol provides the perfect vehicle for droplet nuclei transmission of contaminants to the lower airway; therefore
a. Proper hand washing should be used before handling equipment.
b. Equipment should undergo regular mechanical cleaning with liquid detergent and water.
c. Equipment should be disinfected periodically with weak acetic acid solution, quaternary ammonium compound, glutaraldehyde, or boiled per equipment manufacturer’s recommendations.
2. By ensuring that the patient and/or caregiver understand the prescription dosage, diluent, and frequency and can physically prepare medication for aerosolized delivery, improper medication dosing is minimized. Unit dose preparations often provide the greatest insurance of proper dosing for those experiencing problems.
VI Bronchial Hygiene Techniques Used in Home Care (Box 32-1)
A Postural drainage, percussion, and vibration (see Chapter 36)
1. Postural drainage uses bodily positioning along with gravity to drain secretions from specific targeted segments of the lung to larger, central airways.
2. Chest percussion is used to dislodge secretions and is performed on inspiration and exhalation using the cupped-hand technique, a palm-held, molded rubber cup-shaped device, or alternatively an electric- or pneumatic-powered percussor. Mechanical percussors are generally a nonreimbursed item.
3. Chest vibration is used to mobilize secretions to larger airways and is performed by placing one hand on top of the other over the affected area. The therapist performs a vibrating action with the arms and hands by tensing his or her shoulders during the patient’s exhalation. This can be delivered via a mechanical vibrating device, which is typically nonreimbursed. Vibration is used alone if the patient cannot tolerate percussion.
B Incentive spirometry, also referred to as sustained maximal inspiration (SMI), is designed to encourage and reinforce the patient to take protracted, slow, deep breaths. This is accomplished using a device that provides patients with visual positive feedback when they inhale at a predetermined flow rate or volume and sustain the inflation for a predetermined amount of time.
C Intermittent positive pressure breathing (IPPB) is a technique used to provide short-term or intermittent mechanical ventilation for the purpose of augmenting lung expansion, delivering aerosolized medication, or assisting ventilation. The goal is to deliver a tidal volume (Vt) greater than the patient can initiate on his or her own; therefore, delivered Vt measurement is used to assess the therapeutic efficacy of IPPB in select patient populations. However, it is used infrequently.
D Flutter valves and positive expiratory pressure (PEP) devices
1. The Flutter device is a small handheld mucus clearance device made of plastic with a pipelike shape. The mouthpiece (or mask) is connected on one end, and an encased steel ball (the flutter device) resting in a plastic circular cone is connected on the other end.
b. On exhalation into the device the steel ball rolls and bounces, creating vibrating PEP in the lungs. The vibrations loosen secretions, and the positive backpressure provides improved peripheral air distribution.
c. The resulting oscillation frequencies range between 6 and 20 Hz.
d. The vibrations, in conjunction with the increase in expiratory pressure, aid in opening airways and facilitate the clearance of mucus.
e. The optimal oscillating frequency for a given patient varies and is determined based on the response to therapy.
f. The oscillation frequencies are adjusted by changing the angle of the tilt of the Flutter device.
2. The PEP device consists of a removable mouthpiece (or mask) and includes a one-way inspiratory valve and an expiratory resistance/frequency adjustable dial with an optional pressure measurement port.
b. Exhaled air is directed through an opening, which is periodically closed by a pivoting cone. The result is a vibrating PEP.
c. The frequency of oscillations ranges from 0 to 30 Hz.
d. The vibrations, in conjunction with the increase in expiratory pressure, aid in opening airways and facilitate the clearance of mucus.
e. The frequency of the vibrations and the resistance of the opening are adjusted by rotating the dial.
3. The primary benefit of the Flutter or PEP devices is that after instruction, the need for a professional to oversee its use is only periodically necessary, with the patient typically self-administering therapy.
1. The forced expiratory technique (FET; “huff cough”) is performed as follows.
1. CoughAssist or in-exsufflator (formerly the Coffilator) by J.H. Emerson Company
a. A portable electric device that uses a blower and valve to alternately apply a positive followed by a negative pressure to the patient’s airway
b. Air is delivered to and from the patient via a breathing circuit with flex tube, bacteria filter, and patient attachment via mask, mouthpiece, or standard artificial airway adapter.
c. Indicated for patients with reduced peak expiratory flows, such as those with high spinal cord injury, neuromuscular deficits, or fatigue secondary to intrinsic pulmonary disease. Medicare reimbursement is provided in these cases.
G High frequency chest wall compression (HFCC)
1. THAIRapy vest developed by American Biosystems Inc.
a. The vest consists of an inflatable jacket and an air-pulse generator.
b. The vest fits snugly over the entire thorax and is connected to the front panel of the air-pulse generator by two hoses to create external chest wall oscillations.
c. Increasing oscillatory frequencies ranging from 5 to 20 Hz are used during the course of each treatment.
d. The device is activated at the patient’s full inspiration, and a 5-minute period of oscillation at low frequency is initiated.
e. Transient increases in airflow are produced at each stepwise increase in compression and result in mobilization and physical alteration of secretions.
f. The patient performs a forced expiratory maneuver before the device is deactivated to allow expectoration of secretions.
g. The cycle is repeated five or six times at gradually increasing frequencies.
2. Hayek Oscillator by Breasy Medical Equipment
a. Uses a microprocessor-controlled noninvasive ventilator
b. The unit is connected to the patient via a traditional cuirass.
c. There is a range of cuirass sizes suitable for preterm infants to adults.
d. The cuirass is attached to a piston pump that can provide ventilation up to high frequencies, and baseline negative pressure is produced from a vacuum pump.
e. Frequencies of up to 15 Hz can be achieved, and frequency, inspiratory and expiratory pressures, and inspiratory-to expiratory (I:E) ratio are controlled variables for patients.
f. Negative and positive pressures are alternately applied during inspiration and exhalation, respectively, with oscillations around a negative baseline followed by an artificial cough.
g. The artificial cough has a prolonged inspiratory phase followed by a short expiratory phase.
H Intrapulmonary percussive ventilation (IPV)
1. Percussionare developed by Dr. Forest Bird
2. IPV is used to mobilize and clear retained secretions, assist in the resolution of atelectasis, and deliver aerosolized medications.
a. Oscillatory pulsations are delivered that generate high frequency bursts of gas at rates of 100 to 300 cycles/min (2 to 5 Hz).
b. The minibursts of air are delivered to the patient’s airway at pressures of 10 to 45 cm H2O during inspiration, with the range adjusted to match the compliance and resistance of the lung and chest wall.
1. Clean versus sterile technique
a. Accepted practice to use a “clean” suction technique in the home
b. The patient should be instructed in self-care whenever possible.
c. Patient or caregiver should use proper hand-washing techniques before handling equipment.
d. Caregivers should use nonsterile (clean) gloves when suctioning a patient with an artificial airway to
e. Gloves are not necessary when suctioning the oral pharynx with a hard tonsillar-type (Yankauer) suction catheter.
2. Reuse of suction catheters is commonly used in the home care setting when the catheters are
a. Externally wiped clean, and the internal lumen is rinsed by aspirating cooled, boiled water (<24 hours old) until clear.
b. Air is aspirated to remove residual water and dry the internal lumen.
c. The catheter is then stored on a clean surface to air dry until next use.
d. Catheters should undergo regular mechanical cleaning with liquid detergent and water followed by daily disinfection with weak acetic acid solution, quaternary ammonium compound, glutaraldehyde, or boiled per equipment manufacturer’s recommendations.
e. Suction catheters handled in this fashion may be used until they lose their integrity.
VII Nasal CPAP and Nasal Positive Pressure Ventilation (NPPV)
A Nasal CPAP is used to manage obstructive sleep apnea (OSA).
1. Nasal CPAP is achieved by creating a prescribed CPAP from a flow generator via a nasal appliance. This same device may be alternatively used with an oral mask.
2. Medicare reimbursement criteria for nasal CPAP
a. Diagnosis of OSA documented by an attended, facility-based polysomnogram that meets either of the following criteria.
(1) The apneic/hypopneic index (AHI) is ≥15 events per hour, or
(2) The AHI is from 5 to 14 events per hour with documented symptoms of
b. Polysomnographic studies must be performed in a facility-based sleep study laboratory and not in the home or a mobile facility. These laboratories must be qualified providers of Medicare services and comply with all applicable state regulatory requirements.
c. A home medical equipment (HME) supplier must not perform polysomnographic studies.
d. Continued coverage of the CPAP device beyond the first 3 months of therapy requires that no sooner than the 61st day after initiating therapy, the supplier ascertain and document from either the patient or the treating physician that the patient is continuing to use the CPAP device.
e. Noncompliant and/or periodic discontinuation of usage of the device may interrupt the supplier’s billing for the equipment and related accessories and supplies.
f. Other third-party payers follow similar, less stringent criteria.
B Nasal noninvasive intermittent positive pressure ventilation (NIPPV) is used to manage OSA, restrictive thoracic disease, severe chronic obstructive pulmonary disease (COPD), or central sleep apnea (CSA). Numerous small NPPV units are available from many manufacturers, but all function in a similar manner.
1. Nasal NPPV is patient sensitive and assists ventilation by creating a prescribed positive inspiratory pressure (IPAP) followed by a less but still positive expiratory pressure (EPAP) via an electronically controlled flow generator applied via a nasal appliance. This same device may alternatively be used with an oral mask. Some units have the feature of setting a backup respiratory rate in the “timed mode,” providing for an assist-control mode.
2. Medicare reimbursement criteria for nasal NPPV
a. Physician must fully document in the patient’s medical record symptoms characteristic of sleep-associated hypoventilation, such as daytime hypersomnolence, excessive fatigue, morning headache, cognitive dysfunction, and dyspnea.
b. Indicated for those patients with clinical disorder groups characterized as (1)restrictive thoracic disorders (i.e., progressive neuromuscular diseases or severe thoracic cage abnormalities); (2) severe COPD; (3) CSA; or (4) OSA, and who also meet the following criteria.
(1) Restrictive thoracic disorders
(a) There is documentation in the patient’s medical record of a progressive neuromuscular disease (e.g., amyotrophic lateral sclerosis) or a severe thoracic cage abnormality (e.g., postthoracoplasty for tuberculosis), and
(b) An arterial blood gas Paco2, done while awake and breathing the patient’s usual FIO2 that is ≥45 mm Hg, or
(c) Sleep oximetry demonstrates oxygen saturation ≤88% for at least five continuous minutes, done while breathing the patient’s usual FIO2, or
(d) For a progressive neuromuscular disease (only), maximal inspiratory pressure <60 cm H2O or forced vital capacity is <50% predicted, and
(e) COPD does not contribute significantly to the patient’s pulmonary limitation.
(f) If all the aforementioned criteria are met, nasal NPPV (based on the judgment of the treating physician) will be covered for patients within this group of conditions during the first 3 months of therapy.
(a) An arterial blood gas Paco2, done while awake and breathing the patient’s usual FIO2 that is ≥52 mm Hg, and
(b) Sleep oximetry demonstrates oxygen saturation ≤88% for at least 5 continuous minutes done while breathing oxygen at 2 L/min or the patient’s usual FIO2 (whichever is higher), and
(c) Before initiating therapy, OSA (and treatment with CPAP) has been considered and ruled out.
(d) If all of the aforementioned criteria for patients with COPD are met, nasal NPPV will be covered for the first 3 months of therapy.
(3) CSA (i.e., apnea not caused by airway obstruction)
(a) A complete facility-based, attended polysomnogram must be performed documenting the following.
(c) The exclusion of OSA as the predominant cause of sleep-associated hypoventilation, and
(d) The ruling out of CPAP as effective therapy if OSA is a component of the sleep-associated hypoventilation, and
(e) Oxygen saturation ≤88% for at least 5 continuous minutes, done while breathing the patient’s usual FIO2, and
(f) Significant improvement of the sleep-associated hypoventilation with the use of nasal NPPV on the settings that will be prescribed for initial use at home, while breathing the patient’s usual FIO2.
(g) If all the aforementioned criteria for patients with CSA are met, nasal NPPV (based on the judgment of the treating physician) will be covered for the first 3 months of therapy.
(a) A complete facility-based, attended polysomnogram has established the diagnosis of OSA according to the following criteria:
(i) The AHI is ≥15 events per hour, or
(ii) The AHI is from 5 to 14 events per hour with documented symptoms of excessive daytime sleepiness, impaired cognition, mood disorders, or insomnia, hypertension, ischemic heart disease, or history of stroke, and
(b) A CPAP device has been tried and proven ineffective.
(c) If the aforementioned criteria for patients with OSA are met, nasal NPPV will be covered for the first 3 months of therapy.
c. Continued coverage of nasal NPPV therapy beyond the first 3 months of therapy requires that no sooner than the 61st day after initiating therapy the physician ascertain and document progress of relevant symptoms and that the patient continues to use the nasal NPPV device at least an average of 4 hours every 24 hours. The supplier also must obtain such documentation from the physician, as well as a statement from the patient documenting use, benefit, and intention for continued use.
d. This reimbursement criterion put forth by Medicare is supported by a review of the available science investigating the clinical indications for Noninvasive Positive Pressure Ventilation in Chronic Respiratory Failure Due to Restrictive Lung Disease, COPD, and Nocturnal Hypoventilation consensus report findings, published in 1999.
e. As with CPAP, other third-party payers follow similar but generally less stringent criteria.
A Thousands of individuals in the United States require long-term mechanical ventilatory assistance.
B It is likely that this number will increase in the future as a result of
2. Cost-effectiveness of elective nocturnal ventilatory support
3. U.S. population demographics increased health care demands
C Possible solutions to the increased need for long-term invasive ventilatory support in the home
1. Meticulous consideration before initiation of mechanical ventilation in the acute care setting of the following.
2. Appropriate elective use of alternative ventilatory assistance
D General indications and disease categories requiring long-term ventilatory support
1. Patients requiring invasive long-term ventilatory support who have demonstrated
a. An inability to be completely weaned from invasive ventilatory support
b. Progression of disease etiology that requires increasing ventilatory support
2. Neuromusculoskeletal disorders: The best candidates have chronic, slowly progressive diseases.
3. Central hypoventilation: Those with sleep apnea secondary to a dominant central (versus obstructive) component, including patients with obese hypoventilation syndrome (OHS), generally are good candidates.
4. Obstructive lung disease: Selective patients are good candidates. Many comply poorly, are difficult to treat, and have many other organ system problems and the typical sequelae associated with chronic pulmonary disease.
5. Restrictive lung disease: Normally such patients are rarely candidates; they generally have the highest respiratory needs.
E The ideal patient for long-term ventilatory support
F The keys to successful transition to the home are appropriate predischarge planning and a well-coordinated team effort. Key members of the discharge team include
2. Patient/family and/or caregivers
4. Respiratory care practitioner
7. Dietician, physical, occupational, and speech therapist as necessary
G Patients requiring nonelective mechanical ventilatory assistance generally require approximately 4 weeks of in-hospital training and acclimation to equipment before transitioning into the home. In the instance of elective ventilatory assistance, namely, the use of NIPPV, the equipment and care needs of the patient are typically less extensive. The discharge plan and process will be streamlined and much quicker than for nonelective cases. In either case the discharge timeframe should be accelerated or decelerated based on individual patient and family needs.
H All respiratory care and other assistive equipment anticipated to be used in the home should be used in the predischarge hospital training to allow mastery of related technique, patient acclimation, and documented medical efficacy. Further home care procedures that may differ from hospital procedures should be adopted by patient and family during the predischarge period as soon as educational mastery is achieved.
I The need for skilled full-time caregivers in the home is based on numerous factors.
a. Adult, adolescent, infant; most infants require at least 8 hr/day of skilled caregiver support.
b. Ventilatory dependence: Typically the greater the number of hours requiring continuous support, the greater the need for skilled caregivers.
a. Reimbursement for ventilator and related equipment and supplies varies greatly among payers. Coverage of outside professionals and/or lay care providers varies to an even greater extent.
b. Many insurers provide minimal home care support.
c. Others reimburse only registered nurse care, even though the patient requires only a companion or lay sitter.
d. Most private insurers have a maximum cap (lifetime benefit) on monies available.
4. Infants generally require more caregiver assistance than adults.
5. Length of time home on ventilatory assistance is generally inversely related to the need for skilled caregivers as patient and family become accustomed with requisite care provision over time.
J Invasive positive pressure ventilation
a. Absence of severe dyspnea or frequent episodes of dyspnea and/or tachypnea
b. Acceptable blood gases with FIO2 level <0.40
d. Stable cardiac function and absence of life-threatening arrhythmia
e. Manageable pulmonary secretions
g. Absence of significant nutritional deficit
h. In general, overall medical optimization and clinical stability with utilization of home care equipment and procedures
2. Other discharge criteria as modified from AARC clinical practice guidelines: 1995
a. The caregivers (lay and professional) must clearly demonstrate and have documented the competencies required for caring for the specific patient. This should include all aspects of the patient’s care needs.
b. Availability of caregivers for each 24-hour period must be ensured.
c. The chosen site must be capable of housing, operating, maintaining, and supporting the equipment required by the patient’s medical condition. This should include respiratory and ancillary equipment and supplies, such as the ventilator, suction, oxygen, intravenous therapy, nutritional therapy, adaptive equipment, and disposable supplies.
d. The physical environment must be evaluated for safety and suitability. It should be free of fire, health, and safety hazards; provide adequate heating, cooling, and ventilation; provide adequate electrical service (and backup generator as indicated); and provide for patient access and mobility with adequate patient space (room to house medical and adaptive equipment) and storage facilities.
e. Financial resources must be identified at the beginning of the discharge process. Lack of or inadequate funding impacts the entire discharge plan and can dictate the discharge care site. Sources and adequacy of funds for alternate-site care, medical equipment and supplies, the required medical personnel, any modifications necessary to environment, and ongoing medical care should be fully evaluated.
f. Development of a multidisciplinary plan of care is based on the evaluation of the patient’s needs and goals. The plan should be consistent with recommended practices and guidelines for the patient’s condition. Key elements of the plan should include
(1) Integration into the community
(2) Patient self-care as appropriate
(3) Roles and responsibilities of team members for daily care management
(4) Documented mechanism for securing and training additional caregivers
(5) Alternative emergency and contingency plans
(6) Use, maintenance, and troubleshooting of equipment
(7) Monitoring and appropriately responding to changes in the patient’s medical condition
(9) Method for ongoing assessment of outcomes
(10) Time frame for implementation
(11) Method to assess growth and development of pediatric patients
(12) Provision of professional medical follow-up evaluation
(13) Documented mechanism for recertifying and remediating patient and other caregivers
g. Some have found a 1- to several-day trial period at home helpful in allowing unanticipated, real day-to-day issues to be identified and then later prepared for in the controlled environment of the hospital before final discharge home. Others view such efforts as laborious and expensive, consuming disproportionate emotional and physical resources for small return. There are no hard and fast rules, and individual consideration of the concept should be given to each discharge situation.
h. When all medical and other criteria have been satisfied, the patient is appropriately prepared for discharge. It should be noted that whatever the external demands, fiscal or otherwise, there are no shortcuts to education or planning that will allow safe, successful discharge.
3. Home mechanical ventilators (general descriptions)
a. Today there are essentially five categories of mechanical ventilators specifically designed and manufactured for home use.
(a) Widespread use in noninvasive home ventilation
(b) New generations continue to be produced; this is the fastest growing segment of home ventilation.
(c) Flow generators capable of delivering high flows
(d) Some have a timed mode providing for backup rate.
(e) Most offer clinician-settable inspiratory rise time and duration.
(f) Some offer adjustable inspiratory and expiratory triggers.
(g) Quiet, compact, and lightweight
(h) Oxygen supplementation can be problematic.
(2) Volume-targeted home care ventilators
(a) Traditional, historical mainstay of home care ventilators
(c) Limited variety of mode application
(3) Pressure/volume-targeted home care ventilators
(a) Newest generation of home care ventilators
(b) Typically turbine driven, capable of delivering large flows
(d) Hybrid of bilevel and acute care ventilators
(e) Adjustable inspiratory rise time and duration
(f) Large variety of mode applications
(h) Stable to precise oxygen delivery
(i) Provide internal battery backup
(k) Can be used for invasive and noninvasive home ventilation
(4) Negative pressure ventilators (see Section K-1, a-g, Negative Pressure Ventilators)
(5) High frequency ventilators (HFVs) or oscillators (see Chapter 42)
b. Ventilators designed primarily for hospital use should not be used in the home. With the large variety of commercially available, full-featured, home care ventilators, it is rare to find a justified exception to this axiom.
4. Ideal characteristics of home care ventilators
a. Designed exclusively with the home care patient in mind
d. Absence of confusing digital readouts that change on a breath-by-breath basis
e. Provide ventilatory support of infant, children, and adult populations
f. Available modes: Assist/control (AC), control, pressure support, synchronized intermittent mandatory ventilation (SIMV), positive end-expiratory pressure (PEEP), and NPPV
g. Respiratory rate: 1 to 80 breaths/min
i. Peak flow capability: 30 to 140 L/min
j. Spontaneous demand peak flow provision: ≤180 L/min
k. Automatic and/or settable leak compensation
l. Inspiratory time: 0.3 to 3.0 seconds
m. Assisted breaths triggered by PEEP compensated, proximal patient airway pressure sensing
n. Direct setting of FIO2 or access for titration of oxygen
p. Internal battery capable of functioning for >2 hours
s. Remote “nurse” call capability
t. Compact (fits on wheelchair), light (<35 lb)
u. Such home care ventilators are manufactured; however, they are the newest, generally most expensive, and not the norm and probably contain features not required in a given patient situation.
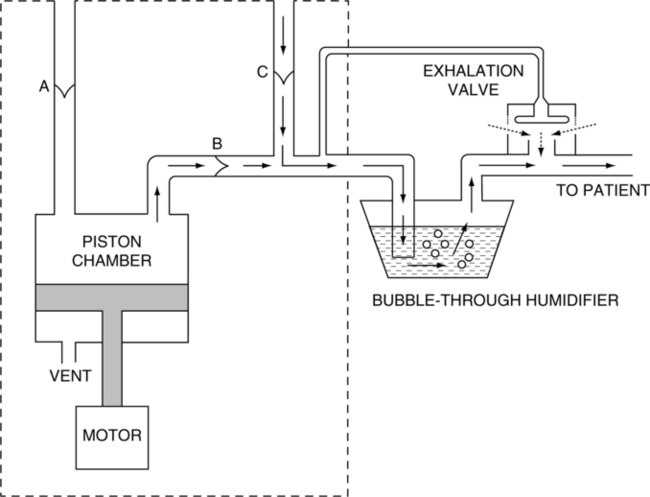
5. The internal gas flow pathway of an older simple, piston-operated, volume-targeted, commonly used home care ventilator in the United States is illustrated in Figure 32-2.
a. Gas enters these units by way of an oxygen-accumulating device with a one-way valve.
b. A one-way valve is also located just inside the unit’s intake filter.
c. From here gas enters the piston chamber during the piston’s back stroke.
d. During the piston’s forward stroke gas exits the piston chamber via a one-way valve, which prevents gas from being drawn into the piston chamber during the piston’s back stroke.
e. A pop-off valve is located in the piston chamber (vent) to prevent excessive chamber pressurization.
f. Once gas exits the piston chamber it normally passes a pressure limit control adjustable by operator and a one-way inlet valve, allowing inspiration of gas from the unit’s circuit during the piston’s back stroke.
g. Not all units include the one-way inlet valve.
h. No demand or continuous gas flow system is included. During spontaneous breathing or SIMV the patient must draw gas from
i. Note: Spontaneous demand flow systems are integral on bilevel and pressure/volume-targeted home care ventilators that avoid the aforementioned problems observed with the older volume-targeted ventilators.
a. Some of these units accept a high 50-psi oxygen and/or air source or a low-pressure 0.5- to 10-psi source.
b. Essentially all units allow an oxygen-accumulating device (reservoir) to be attached to the gas entry port.
c. The use of the integral FIO2 blender is the most accurate when supplied; however, the use of an accumulator produces a suitably consistent FIO2 (±3% to 4%) with home care ventilators.
d. Oxygen may also be bled into the circuit by the use of a T attached between the ventilator and the humidifying device.
e. In the instance of NPPV, oxygen may be bled directly into the facial appliance within manufacturer-recommended limitations.
a. Bilevel and most pressure- and volume-targeted home care ventilators have an integral PEEP feature with manually settable or automatic sensitivity compensation available.
b. The traditional volume-targeted home care ventilators are not designed for the application of PEEP.
c. A PEEP valve may be placed at the exhalation valve.
d. However, the patient’s ability to trigger the machine is grossly affected with the work of breathing (WOB) greatly increased (see Chapter 40).
e. As a result the use of external PEEP devices with these ventilators is discouraged.
a. Spontaneous demand systems are integral on pressure- and volume-targeted home care ventilators and are capable of meeting most patient peak inspiratory flow demands.
b. Many of the volume-targeted home care ventilators posing a SIMV/IMV mode do not have a demand system or continuous flow setup included in the system’s basic design.
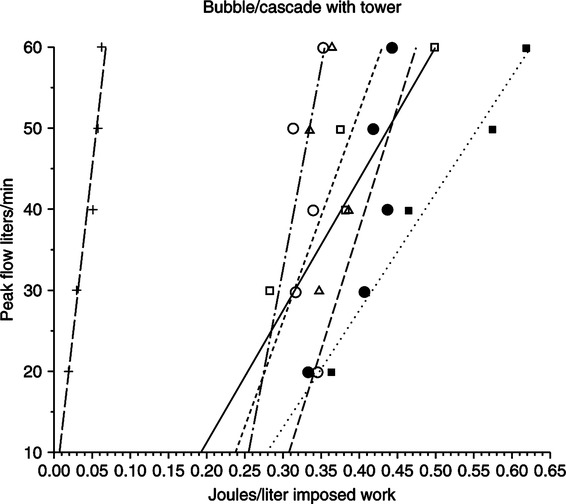
c. When such a unit is set on SIMV/IMV with the use of a bubble-through humidifier, the imposed WOB is excessive (Figure 32-3).
d. Even the use of passover humidifiers or heat and moisture exchangers does not sufficiently reduce the WOB.
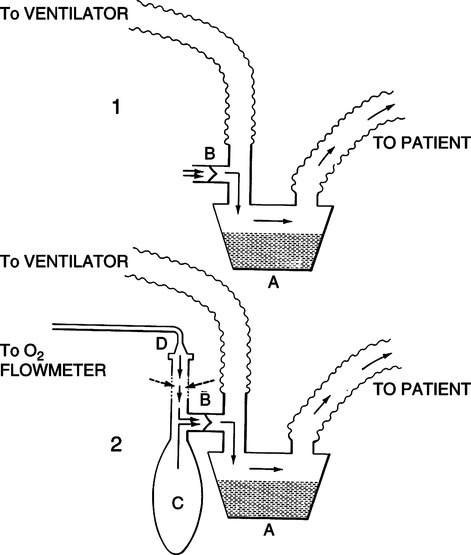
e. In this situation if the SIMV/IMV mode is to be used, a one-way H-valve system placed before the system’s passover humidifier should be used (Figure 32-4).
f. If an increased FIO2 value is needed oxygen can be titrated into the one-way H-valve system as shown in Figure 32-4.
g. The use of a one-way valve and a passover humidifier greatly reduces the imposed WOB of these systems in the SIMV/IMV mode.
9. Selection of ventilator parameters (adults)
a. Criteria outlined in Chapters 21, 22, and 41 should be followed.
b. Volume or pressure AC when the ventilator is equipped with a spontaneous demand system; otherwise volume AC
10. Selection of ventilator parameters (infants)
a. Many infants are weaned from mechanical ventilation in the home.
b. Small, eventually weanable infants may require the use of pressure-limited continuous flow SIMV or PSV.
c. Accomplished by most of the commercially available home care ventilators or alternatively by the addition of the one-way H-valve reservoir system depicted in Figure 32-4 and the use of a pop-off valve in the ventilator circuit to maintain the pressure plateau.
d. Criteria outlined in Chapters 28 and 30 should be followed during parameter selection.
K Noninvasive nonpositive pressure approaches to mechanical ventilation
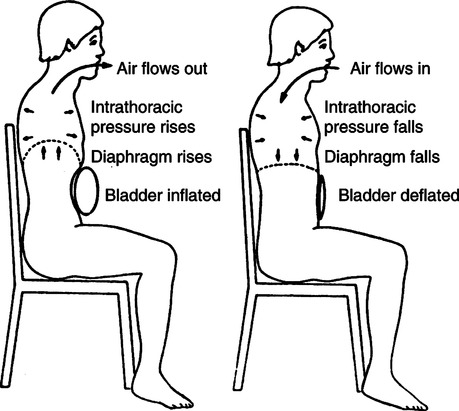
a. NPV is provided by applying a settable subatmospheric pressure to the thorax and abdomen on an intermittent basis, which causes an increase in thoracic and abdominal volume and a resultant decrease in respective pressures. These subatmospheric pressures are in turn transmitted to the lungs, creating a pressure gradient from atmosphere to lungs and resulting in inspiratory flow. Exhalation occurs passively when the machine-imposed subatmospheric pressure is intermittently stopped, and the normal elastic recoil of lungs, thorax, and abdomen increases intrapulmonary pressure, creating a pressure gradient from lungs to atmosphere.
b. NPV can be provided with the use of
c. The size of the Vt generated by a given negative pressure is a function of the thoracic and abdominal compliance, the airway resistance, and the surface area of negative pressure exposure. Hence NPV functions best on individuals with normal lungs and normal thoracic compliance typical of patients with neuromuscular disease. However, NPV has successfully been used to support other disease entities.
d. It should not be used for patients with upper airway obstruction because it will exaggerate the obstructive component.
e. For optimal use, respiratory rates and pressure must be high enough to capture the diaphragm and inhibit spontaneous ventilation. Optimally the diaphragm will work in synchrony with the ventilator.
f. Most negative pressure units are controllers, with the newly manufactured units featuring a patient-triggered AC mode providing greater synchrony with spontaneous ventilatory effort.
g. The use of NPV is frequently successful when it is combined with other noninvasive approaches to ventilation.
a. This is a belt with an inflatable bladder designed to compress the abdominal contents and move the diaphragm up to assist exhalation.
b. Inspiration occurs when the balloon deflates, allowing the abdominal contents and diaphragm to move downward.
c. It is effective only in the sitting position (at least 30 degrees).
d. A pressure generator is used to inflate the bladder. Pressures of 50 to 70 cm H2O are required, with the volume of gas entering the bladder approaching 2000 ml to ensure appropriate movement.
e. Vt of 300 to 500 ml can be achieved.
f. These units typically function as controllers, with newer devices incorporating an AC mode.

a. A rocking bed is a hospital-style bed designed to move the head and the foot of the bed in alternating rhythmic, opposite directions.
b. Thus head up/feet down tilt assists inspiration by moving the abdominal contents downward.
c. Head down/feet up tilt assists exhalation by moving the abdominal contents upward.
d. A maximum of a 60-degree arc is available.
e. The rocking occurs at a rate between 8 and 34/min.
f. It is most effective for neuromuscular disease patients.
g. Normally it is ineffective in thin patients.
h. Frequently it is used with other forms of noninvasive mechanical ventilation.