Chapter 22 HIV/AIDS
GASTROINTESTINAL AND LIVER MANIFESTATIONS
INTRODUCTION
Clinical advances have evolved in consonance with a greater understanding of the virologic and immunologic markers of disease stage, mechanisms of viral transmission and the problem of viral resistance to antiretroviral drugs. Gastrointestinal and hepatobiliary complications are important components of the HIV/AIDS syndrome. They are common and affect most patients with AIDS during the course of their illness.
CHRONIC DIARRHOEA
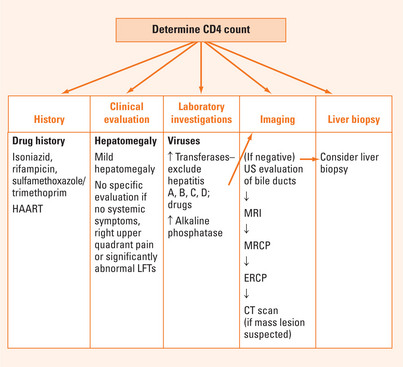
Because of the wide spectrum of potential infections that may cause diarrhoea (Table 22.1), it is appropriate to have a systematic approach in investigating the aetiologic agent/s (Figure 22.1; Table 22.2). Weight loss and diarrhoea suggest an opportunistic infection, malabsorption or small bowel bacterial overgrowth. Severe watery diarrhoea suggests cryptosporidiosis. Diarrhoea with nausea and abdominal pain may indicate Giardia, Isospora belli or Mycobacterium avium. Rectal bleeding may indicate viral or bacterial colitis or Kaposi’s sarcoma.
| Protozoa | Microsporidium; Cryptosporidium; Isospora belli, Giardia lamblia, Blastocystis hominis; Pneumocystis carinii; Entamoeba histolytica |
| Bacteria | Mycobacterium tuberculosis; Mycobacterium avium complex (MAC); Clostridium difficile; Salmonella, Shigella, Campylobacter |
| Viruses | Cytomegalovirus; herpes simplex; adenovirus; rotavirus |
| Fungi | Candidiasis; Cryptococcus; Histoplasmosis; Coccidioidomycosis |
| Neoplasms | Lymphoma, Kaposi’s sarcoma |
| Drug-induced | HIV protease inhibitors |
| Idiopathic | AIDS enteropathy |
| Pancreatic disease | Pancreatitis; infectious pancreatitis; drug-induced pancreatitis |
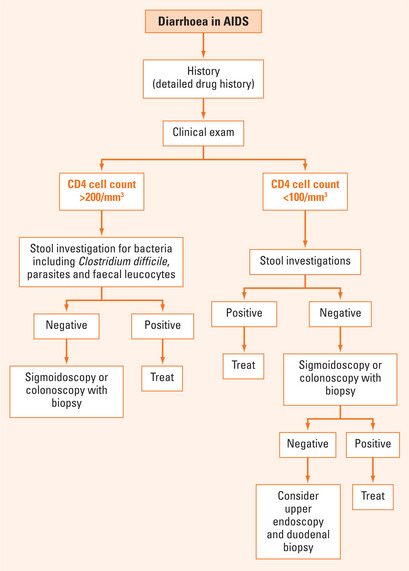
FIGURE 22.1 Assessment of diarrhoea in AIDS.
Based on Wilcox CM. AIDS and the gut. In: Weinstein WM, Hawkey CJ, Bosch J, eds. Clinical gastroenterology and hepatology. Philadelphia: Mosby; 2005:8331–6, with permission.
TABLE 22.2 Assessment of diarrhoea in AIDS
A clinical caveat is to assess whether the patient is at risk for an opportunistic infection. The CD4 lymphocyte count is critical to answer the question (see Figure 22.1). If the CD count is less than 100/mm3 (μ/L), opportunistic infections are probable.
Appropriate tests on faeces can facilitate a diagnosis. The initial laboratory investigation is an assessment of microscopy, culture and parasites. Three sampling tests are recommended. If the CD4 lymphocyte count is <200/mm3, then check for cryptosporidia, microsporidia and Clostridium difficile. Blood cultures should be done in febrile patients with a CD4 <100/mm3, including mycobacteria.
The risk for small intestine Mycobacterium avium infection is increased when the CD4 count is <100/mm3. Duodenal biopsy is required to establish the diagnosis. However, if blood cultures are positive for mycobacteria, biopsy is unnecessary and antimicrobial therapy should be initiated. Table 22.3 lists treatment options for diarrhoea as a result of specific pathogens.
TABLE 22.3 Treatment of diarrhoea
| Protozoa: treatment duration 14–28 days |
| Bacteria
• Mycobacterium tuberculosis: isoniazid, rifampicin, pyrazinamide, ethambutol. Treatment duration: 9–12 months
|
| Viruses |
| Fungi |
N.B. Prior to the advent of HAART, diarrhoea occurred in 90% of AIDS patients.
However, with the inception of HAART, diarrhoea is still frequent but is most often drug-induced or caused by disorders unrelated to HIV infection.
Drug-induced diarrhoea due to the highly active antiretroviral treatment (HAART) regimen is frequent but is usually mild. If no cause of diarrhoea is found, symptomatic therapy is indicated.
HEPATOBILIARY DISEASE
The diagnosis of liver disease should encompass history, physical examination, liver tests and CD4 lymphocyte count (Figure 22.2).
Table 22.4 details the spectrum of hepatobiliary disease in AIDS. Opportunistic infections and neoplasms usually involve the liver secondarily through lymphohaematogenous dissemination. Therefore, initial evaluation of blood or bone marrow specimens may provide important information towards a diagnosis.
| Hepatobiliary disease | Example |
| Viral hepatitis | Hepatitis A, B, C and D, cytomegalovirus, Epstein-Barr virus, herpes simplex virus, human immunodeficiency virus |
| Opportunistic infections | Mycobacterium avium complex (MAC), Cryptosporidium, Candida albicans, Mycobacterium tuberculosis, Coccidioides immitis, Pneumocystis carinii, Cryptococcus neoformans, Histoplasma capsulatum |
| AIDS cholangiopathy | Acalculous cholecystitis, sclerosing cholangitis, papillary stenosis, lymphoma of the biliary tree, Kaposi’s sarcoma |
| Neoplasms | Kaposi’s sarcoma, non-Hodgkin’s lymphoma |
| Drug-induced hepatitis |
Causes of hepatobiliary disease depend on the extent of immunocompromise. If the CD4 count is >500/mm3, hepatic complications usually represent liver specific processes. When the CD4 cell count is <200/mm3, then the liver is usually involved as part of a systemic opportunistic infection due to M. avium complex, fungi or CMV.
Liver biopsy should be considered in patients in whom a treatable cause of parenchymal liver disease is suspected, and when blood cultures and other non-invasive tests do not reveal a cause.
TREATMENT OF HIV
Initiation therapy is recommended in all symptomatic persons and in asymptomatic persons after the CD4 cell count falls below 350/mm3 and before it declines to 200/mm3. A non-nucleoside reverse transcriptase inhibitor or a protease inhibitor boosted with low-dose ritonavir each combined with two nucleoside (or nucleotide) reverse transcriptase inhibitors is recommended with choice based on the individual patient profile. Therapy should be changed when toxicity or intolerance mandate it, or in the event of treatment failure. The virologic target for patients with treatment failure is a plasma HIV-1 RNA level below 50 copies/mL.
Campbell MS, Reddy RK. HIV and the liver. In: Friedman LS, Keefe EB, editors. Handbook of liver disease. 2nd edn. Philadelphia: Churchill Livingstone; 2006:317-327.
Hammer SM, Saag MS, Schechter M. Treatment of adult HIV infection: 2006 recommendations of the International AIDS Society–USA Panel. JAMA. 2006;296:827-843.
UNAIDS/WHO. AIDS epidemic update: December 2005. Report. Online. Available: http://www.unaids.org/epi/2005/doc/report.asp
Wilcox CM, Rabeneck L, Friedman S. AGA technical review: malnutrition and cachexia, chronic diarrhea, and hepatobiliary disease in patients with human deficiency virus infection. Gastroenterology. 1996;111:1724-1752.
Wilcox CM. AIDS and the gut. In: Weinstein WM, Hawkey CJ, Bosch J, editors. Clinical gastroenterology and hepatology. Philadelphia: Mosby; 2005:8331-8336.