History taking
Abnormalities of the blood are associated with a wide range of symptoms and these are discussed in detail under diagnostic headings in subsequent sections. The intention of this section is to give an overview of history taking in patients with blood disorders. Despite the advent of sophisticated laboratory equipment to test blood, a thorough history remains fundamental to accurate diagnosis. In practice the history may precede and then follow the knowledge of a laboratory test abnormality. Whatever the order of events, only by considering symptoms, physical signs and laboratory results in conjunction can the correct conclusion be reached and the patient be managed in the appropriate psychosocial setting (Fig 7.1).
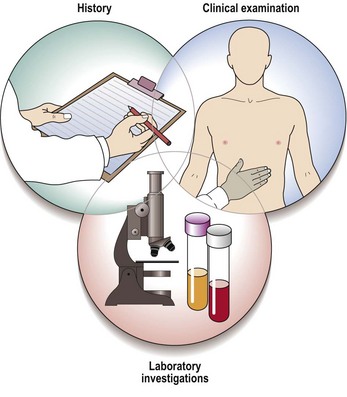
Fig 7.1 The history, clinical examination and laboratory investigations are all essential in the diagnosis of a disorder of the blood.
History of the presenting complaint
Patients may be asymptomatic and have an unpredictable abnormality detected on a routine blood count. Other patients present to the doctor with complaints dependent on the nature of the change in the blood. Some will have several blood abnormalities and present with a large number of symptoms. Despite this complexity it is possible to highlight some common groups of symptoms (Table 7.1).
Table 7.1
Common haematological abnormalities and associated symptoms
| Nature of abnormality1 | Commonly associated symptoms |
| Anaemia | Fatigue, weakness, dyspnoea, palpitations, headache, dizziness, tinnitus |
| Leucopenia (particularly neutropenia) | Unusually severe or recurrent infections |
| Thrombocytopenia | Easy bruising, excessive bleeding after trauma, spontaneous bleeding from mucous membranes |
| Defective coagulation (e.g. key factor deficiency) | Excessive bleeding after trauma, spontaneous bleeds into joints and muscles |
| Infiltration by malignancy (e.g. leukaemia, lymphoma) | ‘Lumps’ caused by lymphadenopathy, pain, neurological symptoms |
1The haematological abnormalities have many possible causes but will always tend to lead to the symptoms shown.
Drug history
Drugs can cause haematological problems – some commoner examples are listed in Table 7.2. A careful drug history (wherever possible verified by checking tablets) may suggest a likely offending agent. If the problem is of sufficient severity to cause concern the drug should ideally be discontinued and the blood count monitored to check resolution. It is as relevant to obtain a history of allergy in haematology as in other areas of medicine. Indeed, patients with haematological malignancies are often given an unusually large number of chemotherapeutic and antimicrobial agents and possible reactions have to be vigilantly documented to avoid repeat exposure.
Table 7.2
Possible haematological side-effects of drugs
| Haematological abnormality | Drugs1 |
| Marrow aplasia | Chloramphenicol (idiosyncratic) |
| Cytotoxics (dose-related) | |
| Haemolytic anaemia | Cephalosporins |
| Penicillins | |
| Leucopenia/agranulocytosis | Phenothiazines |
| Sulphonamides | |
| Thrombocytopenia | Quinine |
| Thiazide diuretics |
1Many drugs have been implicated in all these abnormalities – the examples shown are some of the more common offenders.
Family history
As can be seen from Table 7.3, a number of blood diseases are inherited. A knowledge of the mode of inheritance is useful in diagnosis and essential in counselling the patient and family. A simple question as to the presence of ‘anaemia’ or a ‘bleeding problem’ in other family members can prevent unnecessary investigation and delay in diagnosis.
Table 7.3
Some inherited blood disorders
| Red cell disorders | |
| Disorders of the membrane | Hereditary spherocytosis and elliptocytosis |
| Disorders of haemoglobin | Thalassaemias and sickle syndromes |
| Disorders of metabolism | Glucose-6-phosphate dehydrogenase and pyruvate kinase deficiencies |
| Coagulation disorders | |
| Factor deficiency | Haemophilia A and B |
| Combined factor and platelet abnormality | von Willebrand disease |
| Platelet abnormality | Bernard–Soulier syndrome (rare) |
| White cell disorders | Rare functional disorders (e.g. chronic granulomatous disease) |
The mode of inheritance of these disorders is discussed in the relevant sections.





