Chapter 1 History of Neurostimulation
 The Melzack-Wall gate control theory was a defining event in the use of neurostimulation in modern medicine.
The Melzack-Wall gate control theory was a defining event in the use of neurostimulation in modern medicine.Early Discoveries
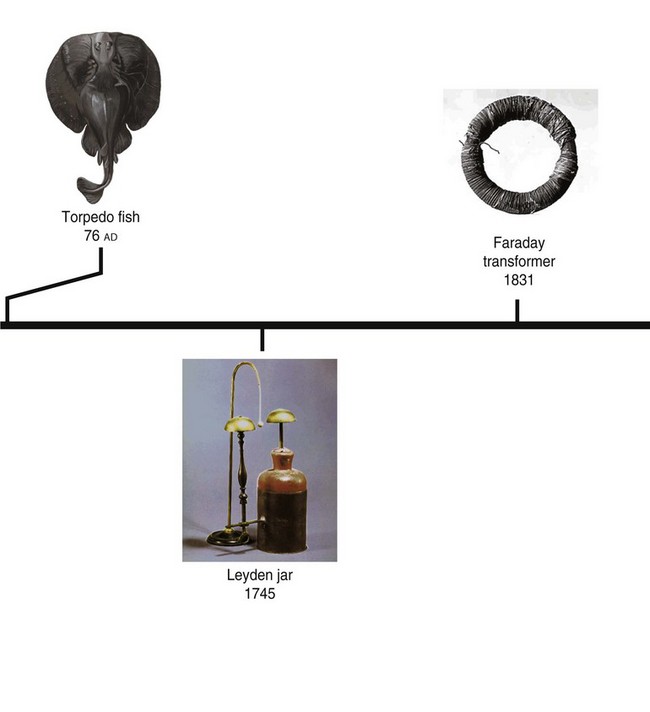
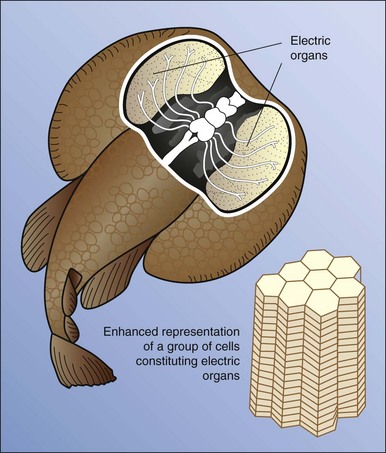
The first documented use of neurostimulation for pain relief occurred in Greece around 63 ad. It was reported by Scribonius Largus that pain from gout was largely relieved by standing on a torpedo fish (Fig. 1-1), and recommended this treatment for pain in general. He said,
“For any type of gout, a live black torpedo should, when the pain begins, be placed under the feet. The patient must stand on a moist shore washed by the sea, and he should stay like this until the whole foot and leg up to the knee is numb. This takes away present pain and prevents pain from coming on if it has not already arisen. In this way Ateros, a freedman of Tiberius, was cured.”1
In 1771 Luigi Galvani, an Italian physician and physicist, discovered that the leg muscles of a frog twitched when electricity was applied, thereby effectively debuting the study of bioelectricity.2 Gilbert, a famous 17th century scientist, described the relationship of electromagnetism to pain symptom management on his discovery that a piece of magnetic iron ore could be used in the treatment of headaches, mental disorders, and marital infidelity.3
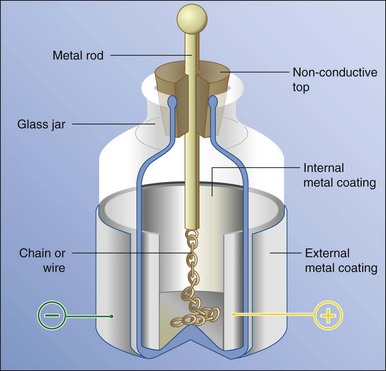
In the years following Gilbert’s work, a method of harnessing electrical current was invented that would allow for the development of modern therapies. This device was called the Leyden jar (Fig. 1-2). This device was constructed by placing water in a metal container and placing brass wire through a cork top into the water. In 1746, using a Leyden jar, Jean Jallabert discovered the ability to use electricity to stimulate muscle fibers. Jallabert treated a paralyzed limb by causing involuntary contractions leading to regeneration of muscle and increased blood flow.4 This success led many others in the field to pursue similar methods of treatment.
In 1756 Leopoldo Caldani observed that a Leyden jar could be discharged in the vicinity of a dissected frog’s leg and cause it to twitch. This discovery led many scientists to believe that application of electricity was in fact a “miracle cure” and that its use in stimulating the body had far-reaching application.5 The French physiologist d’Arsonval found that the application of high-frequency current (10,000 oscillations/sec) could reduce pain. In 1890 Hertz demonstrated that when he was able to achieve 1,000,000,000 oscillations/sec, tissue was not stimulated in a painful manner. This initial stimulation was at a low voltage. This was eventually increased by Hertz’s spark gap resonator, which allowed the use of a gap in the otherwise complete electrical circuit to discharge current at a prescribed voltage. This increase in voltage control, along with high frequency, led to successful treatment of arthritis, pain, and tumors. The developments of d’Arsonval and Hertz remain critical for modern-day stimulation programming platforms.
Between 1884 and 1886 Sir Victor Horsely introduced the first practical use of intraoperative neurostimulation. Horsley’s application of stimulation was used to identify a particular cortical area in a patient with epileptic foci.6
Modern Medicine
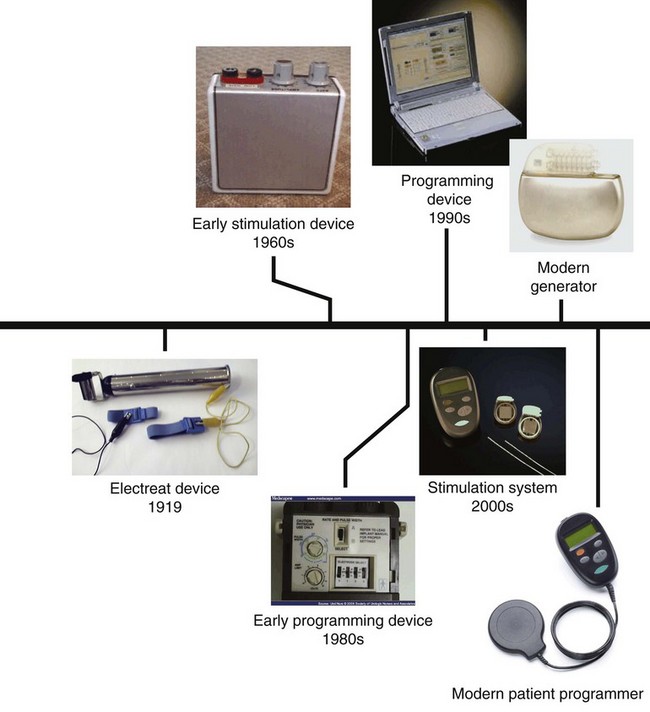
By the early 1900s many devices, including transcutaneous electrical nerve stimulation (TENS) devices, similar to today’s TENS units, were available to treat all manner of pain conditions. The Electreat (Fig. 1-3), patented by Charles Willie Kent in 1919, sold as many as 250,000 units in 25 years. Most physicians’ offices had one of these devices, and used it to treat all manner of conditions, including baldness, gout, and rheumatic feet.
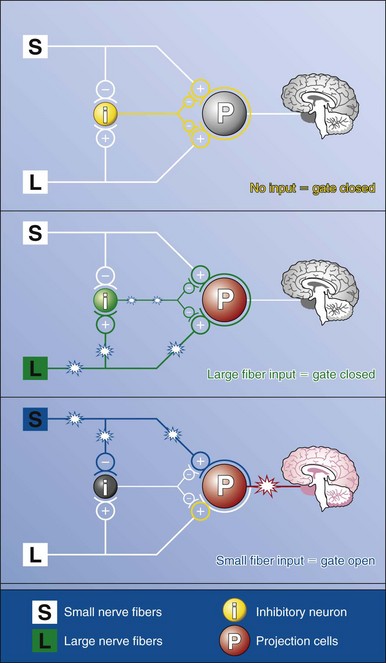
The use of neurostimulation in modern medicine had its true beginning in the 1960s. In the 1965 Science article, “Pain Mechanisms: A New Theory,” Melzak and Wall proposed the gate control theory,7 which assisted in furthering the understanding of neurostimulation by describing the inhibitory and excitatory relationships in pain pathways (Fig. 1-4). Norman Shealy is credited with introducing the neurostimulation in true clinical practice when he and his research assistant developed a stimulating lead to work on the dorsal columns of the spinal cord.8 The lead consisted of a platinum electrode with positive and negative electrodes. It was used in the treatment of a terminally ill cancer patient, placed in the intrathecal space, and attached to an external cardiac electrical generator. Shealy referred to these devices as dorsal column stimulators; they were specifically intended for pain relief. Unfortunately, many serious complications were associated with these early devices, including compression of the spinal cord and spinal fluid leakage. These safety concerns led many to believe that this form of treatment was not a safe alternative to other noninvasive techniques; and, until the development of the extradural placement method, many were wary of its use.
By the late 1960s Medtronic obtained Food and Drug Administration approval to distribute these devices for the treatment of pain. Shealy, Mortimer, and Reswick8 advanced the technique to stimulate the epidural space with increasing success.
Deep Brain and Motor Cortex Stimulation
In 1973 Hosobuchi, Adams, and Rutkin9 discovered that these devices could be used in the deep brain to treat facial pain, effectively leading to the discovery of DBS for pain control. In 1991 Tsubokawa and colleagues10 reported that motor cortex stimulation alleviated pain of central origin. This landmark study introduced the theory and practice of motor cortex stimulation. After some early concerns, DBS was given approval for the treatment of movement disorders in Parkinson disease and dystonia. A number of clinical studies related to depression, obsessive-compulsive disorder, and brain injury are currently underway for deep brain and motor cortex stimulation.
Peripheral Nerve Stimulation
Nerve conduction theory was described in 1826 by Johannes P. Muller, and in 1912 von Perthes was the first to describe the technique of peripheral nerve stimulation to localize a particular nerve.11 In 1955 Pearson12 reported success in locating motor nerves by using a transformer, a vacuum tube stimulator, and an electrophrenic stimulator. In 1969 Ballard D. Wright13 described the usage of the block-aid monitor, a commercially available device, for successful peripheral nerve stimulation; it was one of the first published accounts of success. Wiener, Hassenbusch, Stanton-Hicks and other important research works have shown that devices could be successfully implanted around the peripheral nerve and create paresthesia in the innervation dermatome of the nerve. Older methods of device placement that required surgical dissection have been replaced with percutaneous placement, leading to improved patient satisfaction and patient safety. Many new devices and treatment indications are on the horizon for this type of stimulation.
Conclusion
Work by Shealy and others in the early development of neurostimulation has been followed by steady advances in both the clinical and technological aspects of pain management. The development of smaller implantable devices (Fig. 1-5), new lead arrays, battery technology, and programmable devices has advanced treatment options for a wider variety of patients. Studies regarding the clinical effectiveness of neurostimulation have further proven the effectiveness of this technology for treatment of multiple disease states. The future holds promise for additional indications and increased access to technology.
1 Stojanovic MP, Andi S. Spinal cord stimulation. Pain Physician. 2002;5(2):156-166.
2 Luigi Galvani and animal electricity: two centuries after the foundation of electrophysiology. Trends Neurosci. 1997;20(10):443-448.
3 Pumfrey S, Tilley D. William Gilbert: forgotten genius. Physics World. November 2003.
4 Experiments on electricity with some conjectures on the cause of its effects (Geneva, vol 8, ed 2, Paris, 1749, 12 mo).
5 Cotti Piero. The discovery of the electric current. Physica B. 1995;204(1-4):367-369. condensed matter
6 Sakas D, Simpson A, Krames E. Operative neuromodulation. Volume 1: Functional neuroprosthetic surgery: an introduction. Verlag, Vienna: Springer; 2007. Volume 1: 482 pages
7 Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971-979.
8 Shealy CN, Mortimer JT, Reswick JB. Electrical inhibition of pain by stimulation of the dorsal columns: preliminary clinical report. Anesth Analg. 1967;46(4):489-491.
9 Hosobuchi Y, Adams J, Rutkin B. Chronic thalamic stimulation for the control of facial anesthesia dolorosa. Arch Neurol. 1973;29(3):158-161.
10 Tsubokawa T, et al. Chronic motor cortex stimulation for the treatment of central pain. Acta Neurochir (Wien). 1991;52(suppl):137-139.
11 Pithers C, Raj P, Ford D. The use of peripheral nerve stimulators for regional anesthesia: a review of experimental characteristics, techniques and clinical applications. Reg Anesth. 1985;10:49-58.
12 Pearson RB. Nerve block in rehabilitation: a technic of needle localization. Arch Phys Med Rehabil. 1955;36(10):631-633.
13 Wright BD. A new use for the block-aid monitor. Anesthesiology. 1969;30(Issue 2):236-237.