4 History and examination
Case 4.1
Questions
• 4.1.1 Which cranial nerves can you examine that will give you information about the level of function of her parasympathetic nervous system? Which tests would you perform?
• 4.1.2 What examinations would you perform to evaluate the level of function of her sympathetic nervous system?
• 4.1.3 What is dermatographia and in what situations would you expect to find it?
Introduction
In learning the traditional approach to the neurological examination a student or inexperienced practitioner may be less interested in minor asymmetries of cranial nerve function or motor and sensory signs, especially when the history does not alert to serious pathology. This is not the case in the functional examination where minor asymmetries or altered functional output are of great significance in the analysis of the physiological lesion. Each test must be performed with alert observational skills and meticulous care, comparing the results bilaterally when possible.
The five parameters of effector response are important clues in gauging the cis of upstream neuron systems
1. Latency and velocity of the response
3. Smoothness of movement of the response
Latency and velocity of a response
The time to summation (TTS) and time to peak summation (TTSp) are terms that describe, respectively, the latency and average velocity of effector responses. The pupillary action observed in response to a light stimulus offers a good illustration of these concepts. Under normal conditions, the pupils will respond with a relatively equal TTS and TTSp in both eyes when stimulated with an equal light stimulus. However, in the situation where the central integrative state of the neurons in the right Edinger–Westphal nucleus or mesencephalic reticular formation is further away from threshold, the TTS of the right eye would be expected to be increased from that of the left. The same result may be expected when measuring the velocity of the response, or an increased time to maximal pupil constriction (increased TTSp). The same result, that is increased TTS and TTSp in the right eye, may be found with an afferent pupil defect such as would occur if the right eye end organ was impeded by a photoreceptor or axonal conduction deficit such as in retinal or optic nerve dysfunction. Thus there is the need for a complete fundoscopic and visual acuity examination when unequal pupil responses are present.
Approaches to developing a differential diagnosis
The basic functional neurological examination
• Blind spots and visual fields
• Pupil size and PLRs (pupil light reflexes)
• Motor and sensory examination of the head
• Motor and sensory examination of the trunk and limbs
• Skin and tympanic temperature patterns
• Ophthalmoscopic/otoscopic examination
Before discussing the history and physical examination procedures in general, it is necessary to give some thought to the reason for performing these activities in the first place. The history and physical examination are procedures that allow the practitioner to develop a clinical impression of the state of health or disease of the patient. Based on the clinical impression, the practitioner then arrives at a working diagnosis of the patient’s condition and develops the most appropriate approach to treatment of the patient.
Once a clear history has been taken from the patient, possibilities from each category can be considered and analysed in light of the symptom picture that the patient has presented with. The following example should illustrate the approach: A 54-year-old male presents with a history of low back pain that radiates into his left leg. The patient works as a construction worker and has a 30-year history of smoking. Diagnostic possibilities based on the VINDICATES approach should be considered (Table 4.1).
Table 4.1 Diagnostic possibilities utilising the VINDICATES pneumonic
| V=Vascular | Deep vein thrombus, varicose veins, Burger’s disease, heart failure, myocardial infarction (atypical presentation), abdominal aortic aneurysm, arthrosclerosis |
| I=Infection | Meningitis, HIV, osteomyelitis |
| N=Neoplastic, Neurological | All carcinomas including emphasis on prostate carcinoma, lung carcinoma—Pancoast tumour, tumours of spinal cord and brain—Schwannomas, glioma, MM, Mets, osteosarcoma, Ewings sarcoma. Herniated or prolapsed vertebral disc, sciatic neuralgia, cervical spondylitic myelopathy, piriformis syndrome, cauda equine syndrome, neurogenic claudication |
| D=Degenerative | Spondylosis of IVF, osteoarthritis, DISH |
| I=Inflammatory | Osteomyelitis, RA, AS, EA, more arthropathie, gout |
| C=Cartilagenous, Congenital, Connective tissue |
Order of the history and examination process
Any healthcare practitioner with training in clinical and neural science has the ability to perform the neurological history and examination in a proficient manner. The key is to develop a routine that can easily be remembered, that can be performed in logical sequential order, and that can be easily improvised for different patient presentations. Two systematic approaches to the neurological examination include the anatomical and functional approaches. The anatomical approach requires examination of the nervous system in a rostrocaudal order (i.e. brain, brainstem/cranial nerves, spinal cord, spinal nerves, receptors, etc.), while the functional approach requires examination of related functions in groups (i.e. mental, motor, sensory, visceral, etc.). A combination of these two approaches is likely to be more efficient, less repetitive, and more appropriate for both the history-taking process and examination as well.
Greater efficiency may be achieved by limiting movement of the patient and using each tool or each type of test only once throughout the examination. If possible, the patient should be assessed in the sitting, standing, and lying positions once and should be assessed in a rostrocaudal order for each function tested. This will reduce the frequency of switching between tools and patient positions. Each instrument used in the examination should be laid out in order of use and within easy reach of the practitioner. With this orderly approach, the practitioner will be less likely to miss any component of the examination (DeMyer 1994). For example, it might be more efficient for the practitioner to determine sensitivity to pain at all levels from the ophthalmic division of the trigeminal nerve to sacral innervated regions, rather than switching between motor and sensory tests at each level.
4. Systems History (special senses, motor, sensory, autonomic, mental)
The neurological examination
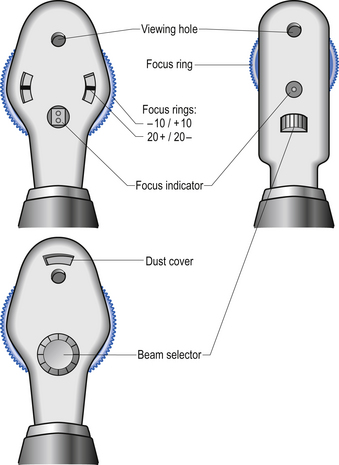
There are numerous excellent texts that cover neurological examination techniques and these have been outlined in the Further Reading section. What will be attempted here is a description of examination techniques or procedures that either differ from the norm or are not covered in traditional texts. As each technique is encountered in the text it will be expanded on to explain in detail the approach necessary. First, some neurodiagnostic testing equipment often utilised in functional neurology will be discussed.
Neurodiagnostic tests
1. Video nystagmography (VNG)—for objective analysis and documentation of visual tracking, saccade, and optokinetic dysfunction, spontaneous nystagmus with and without visual fixation, unilateral weakness (canal paresis) and directional preponderance (central asymmetry) via caloric irrigation, positional tests, and others.
2. Vestibular evoked myogenic potentials (VEMPs)—for objective analysis of certain components of the vestibulocollic reflex. Latency and amplitude of motor signals to the sternocleidomastoid (SCM) muscle are measured following stimulation of the saccule with loud auditory stimuli.
3. Balance platform—Objective analysis of postural sway in various conditions using a force platform.
4. Electrocochleography—Objective analysis of short latency responses from the cochlear apparatus and nerve.
5. Auditory brainstem responses—Objective analysis of brainstem responses to auditory stimuli to complement VEMPs.
6. Electroencephalography (EEG) and qEEG—the neuron electrical activity is measured over the scalp by very powerful receptors and then amplified to produce wave patterns that can be used to give objective projections of the state of brain function. This technique has become very powerful with the addition of source localisation software such as that offered by the Key institute which can combine low-resolution tomographic analysis (LORETA) and MRI anatomical library data to give very accurate localisation of EEG data.
7. Advanced imaging—MRI, CT, Doppler ultrasound if history and examination suggests ablative lesion of sinister aetiology or if patient is not responding to care. To be discussed further.
8. Audiometry—also useful and it is important that copies of all reports concerning hearing, vision, balance, and imaging are requested.
The examination process
Observation
1. Note the general appearance of the patient and their body morphology.
2. Note the patient’s manner and disposition.
3. Look for postural angulations of the head, trunk, and limbs.
4. Note the condition of the skin, nails, and hair.
5. Note skin lesions, pigmentary differences, nevi, oedema, and vascularity.
6. Note any asymmetries of pupil size or position, and observe for ptosis and lid lag.
7. Note any asymmetries of facial muscles and structure and observe the hairline.
Vital signs
1. Determine the heart and respiratory rate and rhythm. These signs can give an indication of the tone of the sympathetic and parasympathetic systems.
2. Determine respiratory dynamics including depth and inspiration/expiration ratio. This can give an indication of the ventilation patterns and thus the pH or acid/base state of the patient.
3. Determine blood pressure bilaterally and record even minor differences as these along with other findings can be important in determining the state of the sympathetic nervous system. Blood pressure should always be measured on both arms. Blood pressure is dependent in part on the peripheral resistance, which can be different on either side of the head and body due to asymmetrical control of vasomotor tone. Increased vasomotor tone can occur because of decreased integrity or CIS of the ipsilateral PMRF, or because of excitatory vestibulosympathetic reflexes.
4. Measure the core temperature. This may give you an indication of the basal metabolic rate of the patient, which is elevated in hyperthyroidism and some cases of infection.
5. Measure the skin and tympanic temperature bilaterally, again recording any differences as these seemingly small variations may be of great clinical importance in determining the blood flow and thus activity levels in each frontal cortex.
6. Determine oxygen saturation if the technology is available.
Examination of the pupils
Various components of the pupil light reflex are subserved by each component of the autonomic nervous system. The TTA, amplitude of constriction, smoothness and maintenance of constriction, TTF, and time to redilation of the pupil response need to be measured and recorded in each pupil. These are all aspects of the pupil light reflex that have been researched and correlated with central integrative state of the various contributing components of the nervous system.
Pupil constriction pathways
The ‘Wernicke’ pupil reaction refers to differential summation depending on whether you are shining the light into the nasal or temporal aspects of the retina (i.e. intact or ablated fields). This may be observed in an optic tract lesion. Supposedly, the resting size of the pupil is uninterrupted because of the consensual light reflex. The nasal half of the retina is significantly more sensitive to light than the temporal half of the retina and the direct responses are significantly larger than the consensual response. Direct and consensual pupil reactions when stimulating the temporal retina are nearly equal. This may suggest an input of temporal retina to both sides of the pretectum. Such a crossing of temporal fibres may take place in the chiasm. The net effect of the pupillary light reaction, which involves shining light into the monocular zone from the temporal hemi-field of one eye, leads to greater constriction of the pupil on that side (Schmid et al. 2000).
Horner’s syndrome
This syndrome is characterised by the following signs and symptoms:
• Ptosis/apparent enophthalmos;
• Anhidrosis (forehead or forequarter of body);
Different lesion levels affect sweating differently. Central lesions may affect sweating over the entire forequarter due to involvement of the descending pathways from the hypothalamus. Lower neck lesions may affect sweating over the face only because of involvement of sympathetic efferents in the arterial plexus (carotid/vertebral). Lesions above the superior cervical ganglion may not affect sweating at all, or it may be restricted to the forehead.
Blind spots and ophthalmoscopy
What are blind spots?
What does it mean?
The area of the visual striate cortex (occipital lobe) representing the blind spot and the monocular crescent (both in the temporal field) does not contain the alternating independent ocular dominance columns. This means that these areas only receive information from one eye. If one closes that eye, the area representing the blind spot of the eye remaining open (on the contralateral side) will not be activated because of the lack of receptor activation at the retina.
The size of the blind spot has been linked to the CIS of the cortex (Carrick 1997).
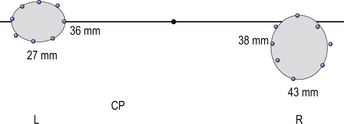
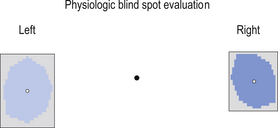
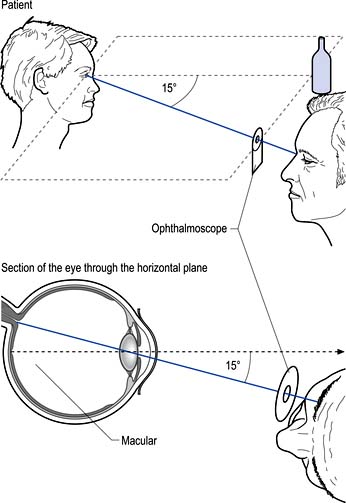
1. Measure the size of the patient’s blind spots using perimetry techniques (Figs 4.3 and 4.4).
Blind spots can also be mapped using the Microsoft Paint program or using the computerised physiological blind spot mapper (Fig. 4.5).
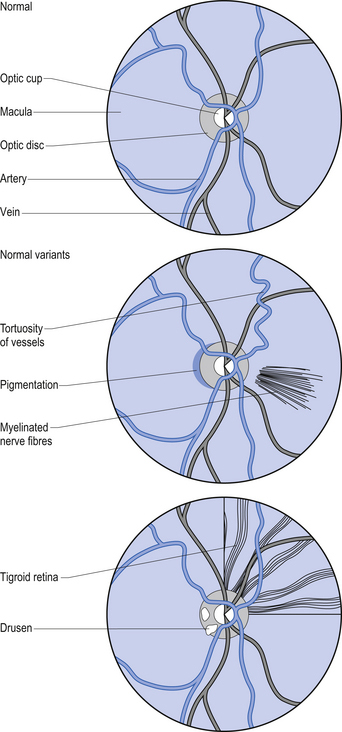
2. Observe the anterior to posterior and nasal to temporal structures of the eye.
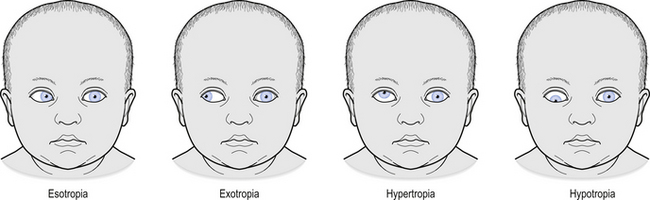
Figure 4.9 The retina in a variety of retinopathies as it may be observed during examination of the fundus. These conditions, unlike the normal variants in Fig. 4.7, warrant significant medical follow-up.
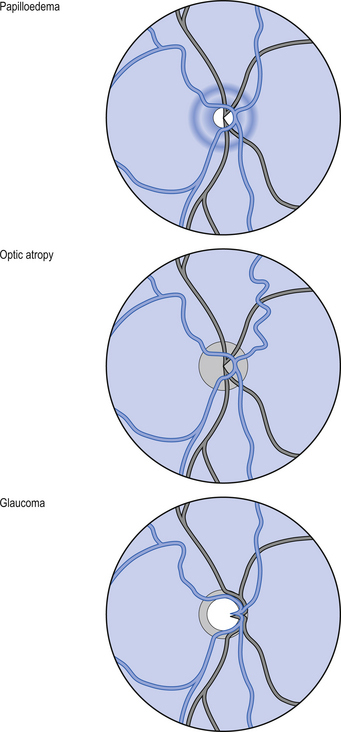
Figure 4.10 Pathologies that may be observed during examination of the fundus. These conditions, similar to those in Fig. 4.9, warrant significant medical follow-up.
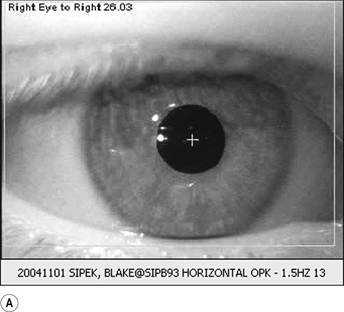
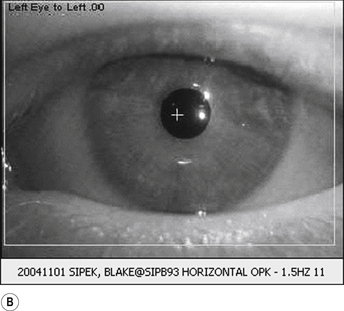
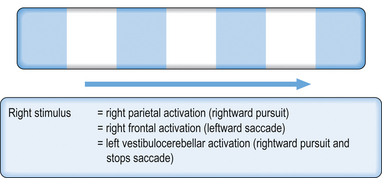
OR can be tested by passing a opticokinetic tape in front of the patient’s eyes, first in one direction and then in the other, and observing the motion of the eyes as the tape is passed. The motion of the eyes should be observed, keeping in mind the latency and velocity of the response, the amplitude of the response, smoothness of movement of the response, the fatigability of the response, and the direction of the response, all of which should be recorded (Fig. 4.11). The opticokinetic tape can be made using a piece of white cloth about 5 cm wide and 1 m long, onto which red pieces of cloth about 5 × 5 cm2 have been stitched at regular 5-cm intervals.
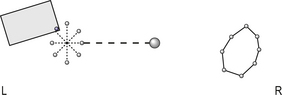
Saccadic eye movements, which are also referred to as saccades, are rapid movements that move the eye from one object to the next. These can be tested by holding up fingers about 1 m apart in front of the patient and asking the patient to look from one finger to the other.
Motor examination of the head
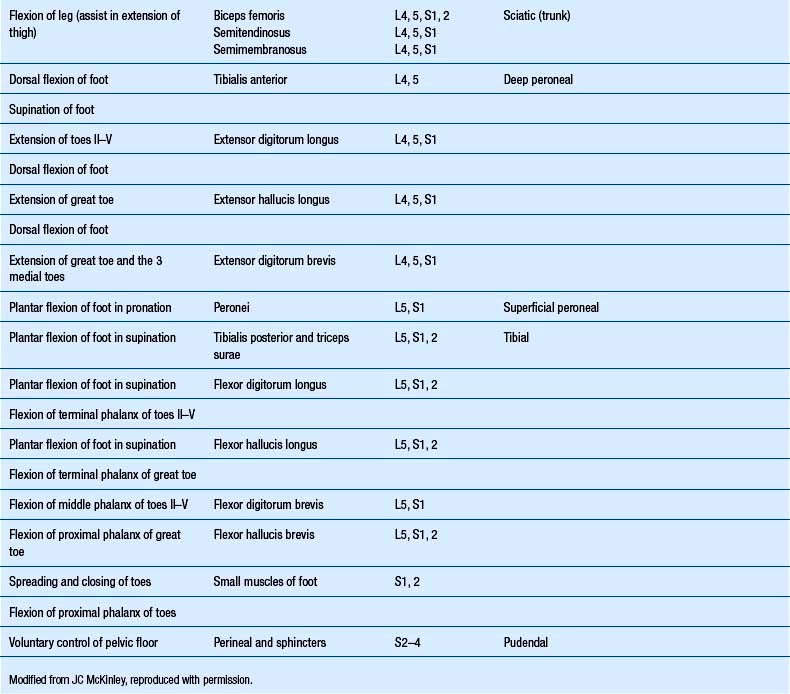
1. Observe the orientation of the pupils and the corneal reflections. This test utilises the reflection of light off the cornea of the eyes when the patient is looking off into the distance. The reflections should be equal in size and position if the eyes are equally deviated.
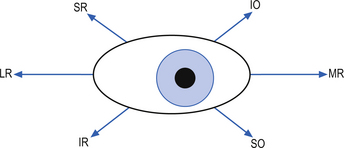
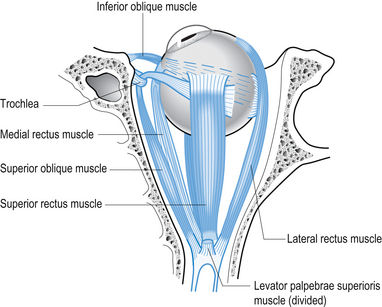
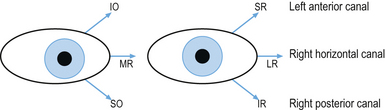
2. Test the six positions of gaze and look for conjugate movements and nystagmus (Fig. 4.12). Relate the movement of the eyes to the anatomy of the eye muscles and note that the muscles of the eye will have different actions when the eye is in different positions (Fig. 4.13).
3. Observe the quality of smooth pursuit in the planes of the semicircular canals. These eye movements require activation of the cerebellum without the activation of the vestibular system and can be used to differentiate between a cerebellar and vestibular dysfunction (Fig. 4.14).
4. Palpate the jaw muscles, observe for jaw deviation, and check the jaw jerk reflex. This reflex tests the motor and sensory divisions of the mandibular division of the trigeminal nerve.
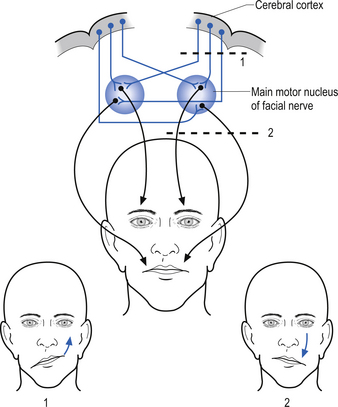
5. Observe for asymmetries in facial muscle contraction, both voluntary and involuntary actions, and both upper and lower face need to be tested. The CN VII nucleus is innervated bilaterally by upper motor corticobulbar neurons. The CN VII nerve itself is ipsilateral in projection to the face. This results in a situation where damage to the CN VII nerve (lower motor neuron) results in ipsilateral paralysis involving the whole side of the face. When supranuclear damage (upper motor neuron) is present, the paralysis is limited to the contralateral forehead area (Fig. 4.15).
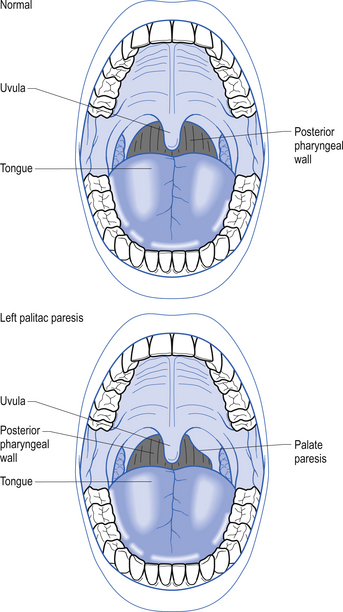
6. Observe for asymmetry in palate elevation (Fig. 4.16).
7. Observe for fasciculations, atrophy, and deviation of the tongue.
8. Observe and feel the tone of the SCM and trapezius muscles during head turning.
9. Observe the quality of the ocular tilt reaction. The OTR is a reflex movement of the eyeball when the head is tilted from one side to the other. When the head tilts to the right the right eye should intort (roll towards the nose) and the left eye should extort (roll away from the nose). This is a vestibular ocular reflex.
10. Observe the patient’s optokinetic reflexes (see above).
11. Observe the patient’s saccades and anti-saccades (see above).
Sensory examination of the head
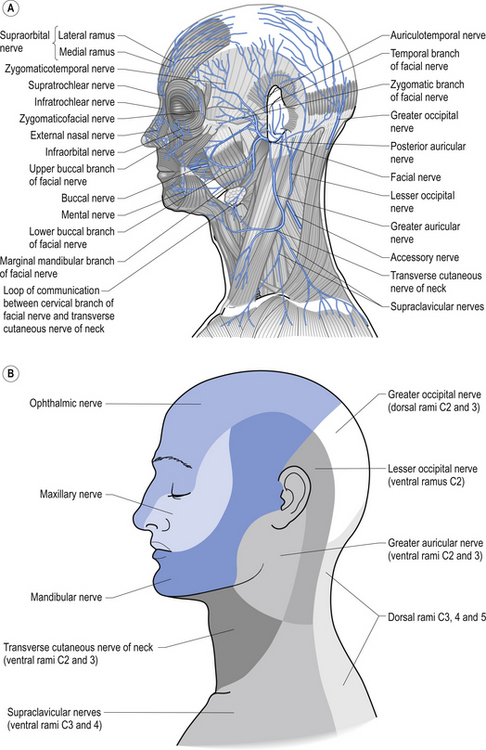
1. Check sensation to pinprick (or pinwheel) in trigeminal and cervical zones (Fig. 4.17).
2. Check sensation to light touch, if indicated.
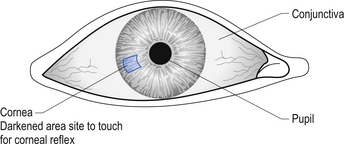
3. Check for quality and asymmetry of the corneal reflex. Many students and practitioners get false results from this reflex because of faulty technique. Several common mistakes include touching the conjunctiva instead of the cornea, approaching the eye too quickly, which is perceived as menacing and results in a blink reflex, and testing over a contact lens, all of which result in inaccurate findings. The area of the eye touched to trigger this reflex correctly is shown in Figure 4.18. The reflex is performed by asking the patient to look up and away and slowly bring a piece of cotton wool twisted to a point in contact with the cornea. Watch for the reaction of both eyes, and the ocular muscles surrounding the eye. The normal response is a bilateral blink and contracture of the muscles of the eyebrows bilaterally. If there is failure of either side to blink you can suspect an ipsilateral trigeminal nerve (CN V) V1 lesion on the side you are testing. If only one side fails to respond you could expect a facial (CN VII) lesion on the side that fails to contract.
Taste, smell, hearing, and otoscopic inspection
1. Check taste sensation on each side of the tongue.
2. Test for smell sensation in each nostril.
3. Check hearing with Weber’s, Rinne’s, and other tests if necessary.
4. Perform otoscopic inspection. This is useful for observing the integrity of the tympanic membrane and investigating the presence of middle and outer ear abnormalities including wax accumulation. History of ear infection may provide an insight into the aetiology of vestibular and auditory symptoms.
Cranial nerve screening
CN II Optic
CN VIII Vestibular and Cochlear
2. Corneal reflection abnormalities
3. Weakness on gaze—contralateral to deficit
4. Nystagmus—vestibular-induced slow phase contralaterally
7. Vestibulo-ocular reflexes (VORs)—decreased gain with rotation to side of deficit
8. Vestibulo-autonomic reflexes as above and below (heart, lungs, gut, head)
9. Neck muscle tension and pain—vestibular-induced increase
10. Extensor muscle tone—vestibular-induced increase
11. Somatic sensation—vestibular-induced pain, ‘numbness’, tingling, etc.
12. Motor and sensory trigeminal signs as above (5)
13. Light sensitivity—vestibular-induced increase contralaterally
14. Postural head tilt—most commonly to side of deficit
15. Deviation on Romberg’s test or walking—most commonly to side of deficit
16. Increased postural sway in sagittal or coronal planes
17. Rotation or side-stepping on Fukuda’s test (marching on the spot with eyes closed for 30 s)—most commonly to side of deficit
18. Accompanying hearing deficits and tinnitus—peripheral mechanisms
19. Hearing deficits and/or tinnitus—altered autonomic and/or dorsal cochlear nucleus integration
20. Aural fullness—sensation of fullness or pain in the ear or surrounding head
21. Frequent headaches (occipital to frontal)—aggravated by fatigue, visual work, light, oversleeping
CN X Vagus
1. Difficulty or tightness swallowing—vestibular-induced anxiety syndrome
2. Increased or decreased bowel movements/sounds (auscultation)—vestibular-induced activation of DMN X
3. Bradycardia—depending on interaction with vestibulosympathetic reflexes (vestibular-induced activation of nucleus ambiguus)
Motor examination of the trunk and limbs
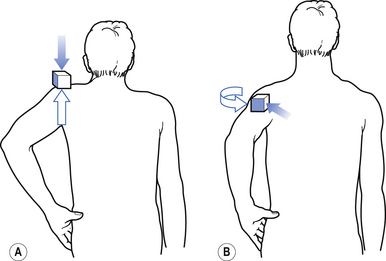
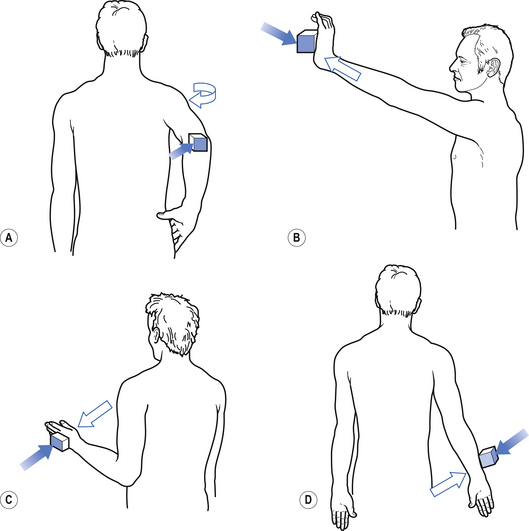
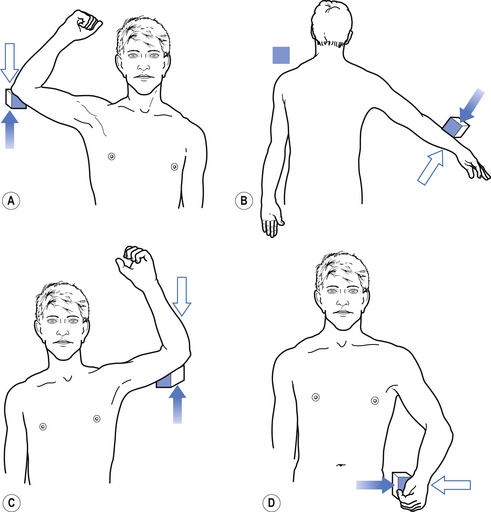
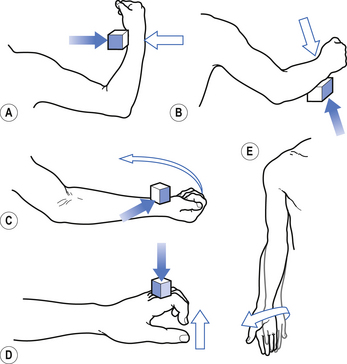
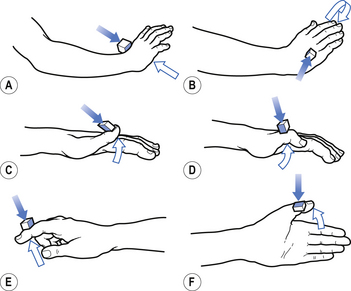
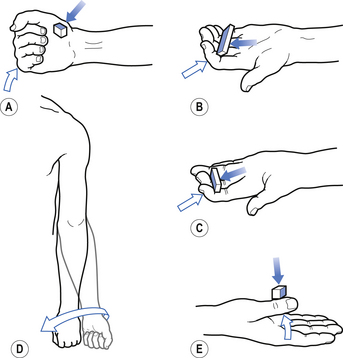
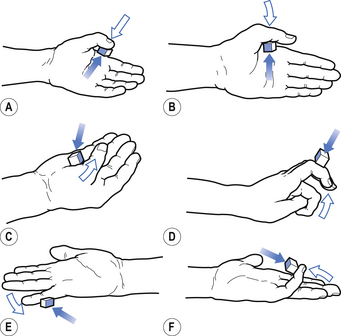
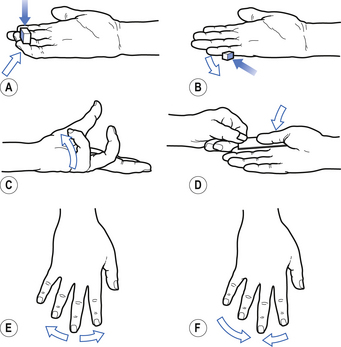
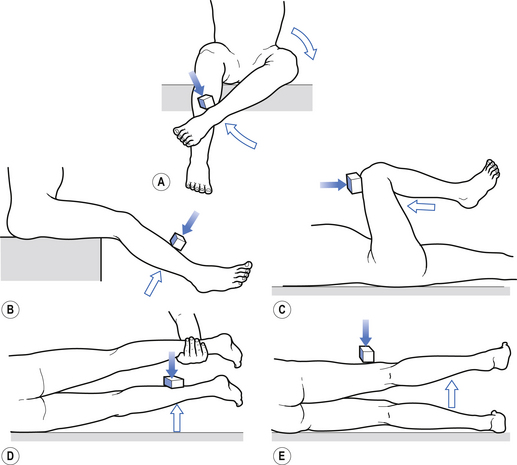
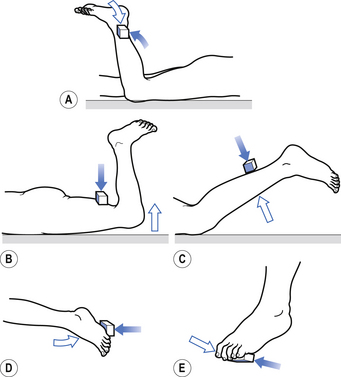
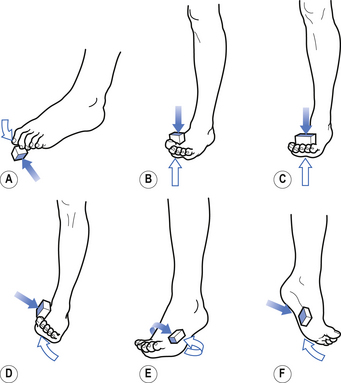
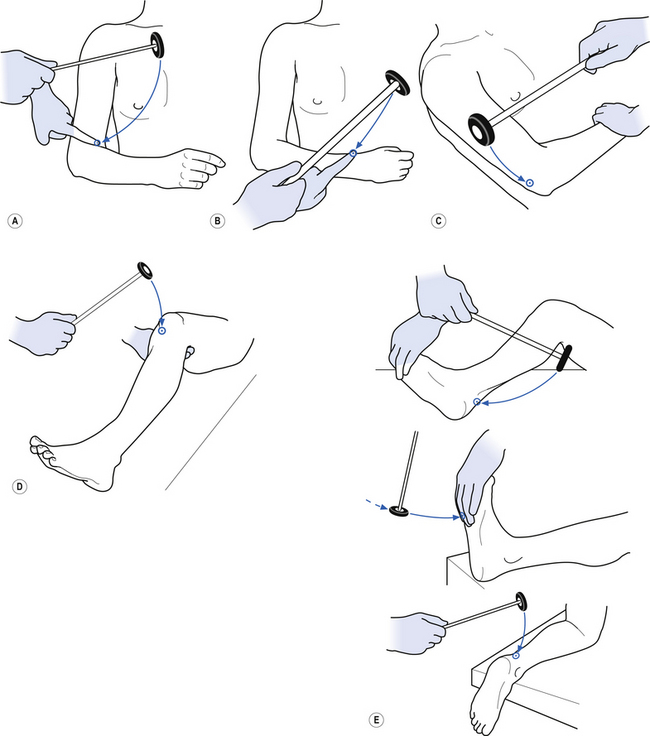
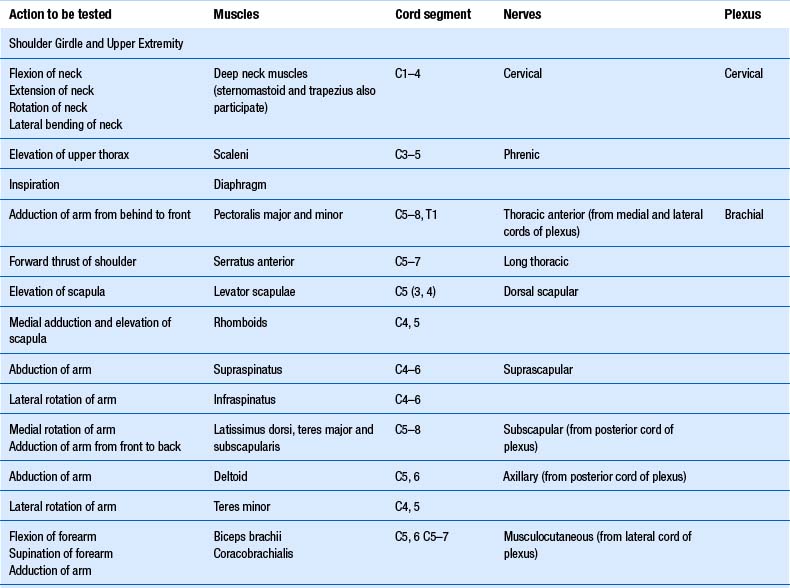
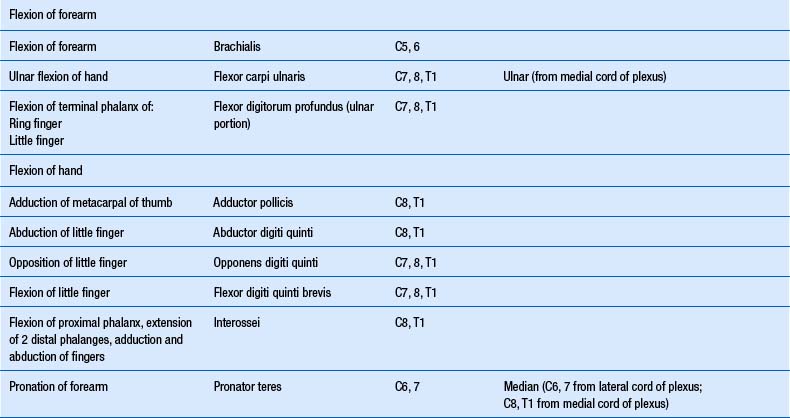
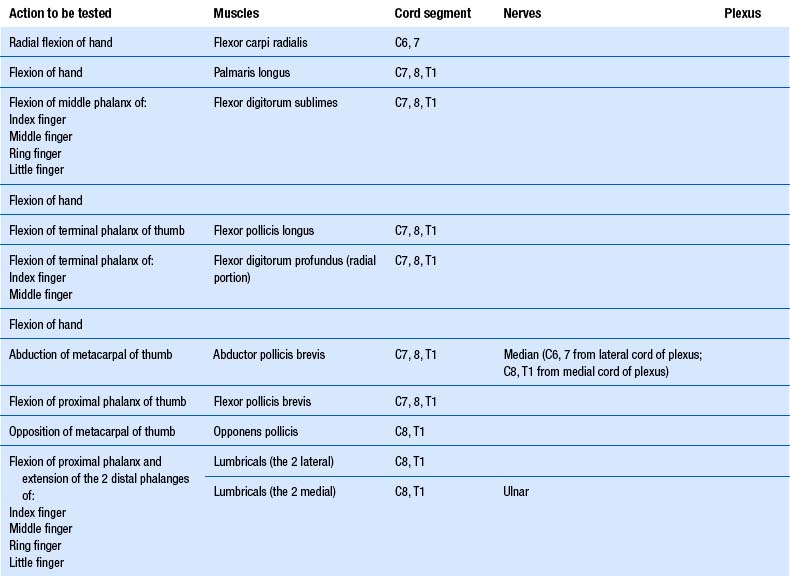
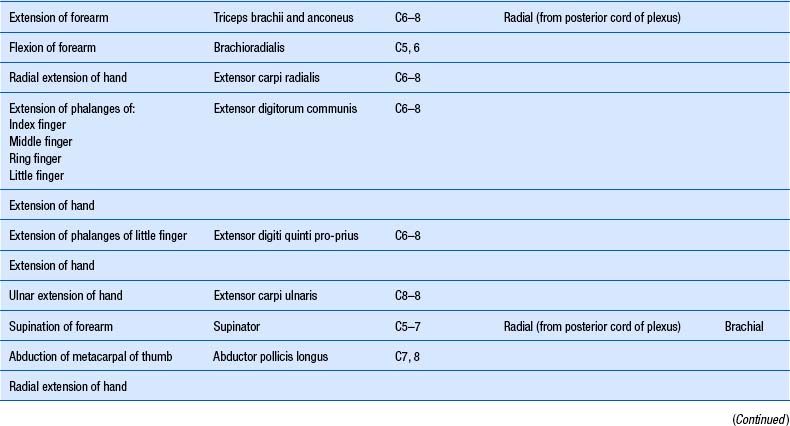
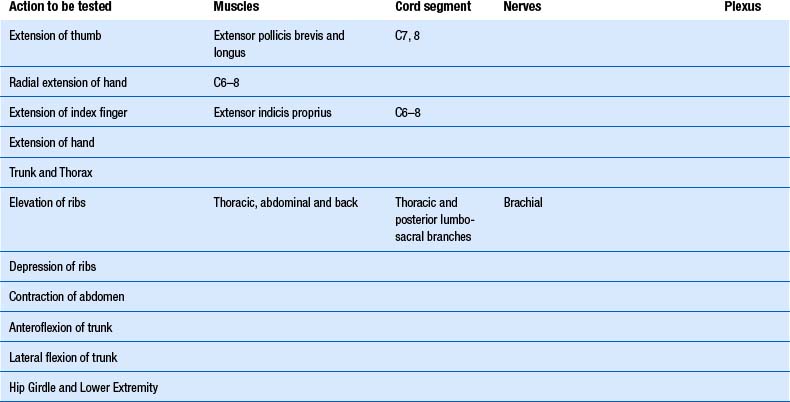
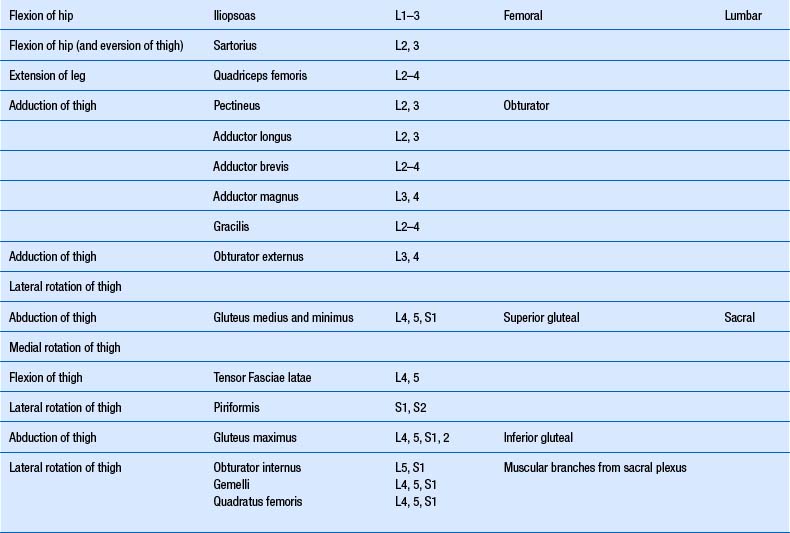
1. Check upper and lower limb muscles for segmental or suprasegmental weakness (see muscle testing diagrams at Figs 4.21 to 4.31).
2. Check upper and lower limb reflexes (see Fig. 4.32). Reflexes should be tested by applying repeated equal strikes of the reflex hammer to the tendon until fatigue occurs or until six or seven strikes have been performed. If the muscle maintains equal responses throughout the six or seven repeated stimuli then the area supplying that reflex can be thought of as expressing a healthy CIS.
3. Check the resistance in muscles to joint motion (muscle tone).
4. Assess for percussion irritability and myotonia.
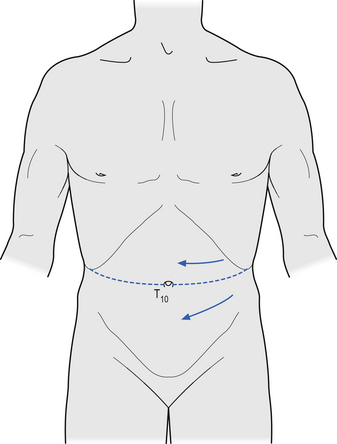
5. Check flexor reflex afferent reflexes, which include the superficial abdominal and plantar reflexes. The superficial abdominal reflex is performed by scratching the abdominal wall as shown in Figure 4.19 and observing the reaction of the abdominal muscles, which should contract on the same side. The afferent supply for this reflex is thought to be the segmental sensory nerves and the efferent supply the segmental motor nerves. The roots tested when striking above the umbilicus are T8–T9 and below the umbilicus T10 and T11. No reaction of the abdominal muscles is a positive response and is thought to indicate an upper motor neuron lesion at the level being tested, but may also present if the lower motor neuron is involved. However, this test is not accurate in a large number of individuals because of the presence of large amounts of abdominal fat or scar tissue formation, or in women who have experienced multiple pregnancies.
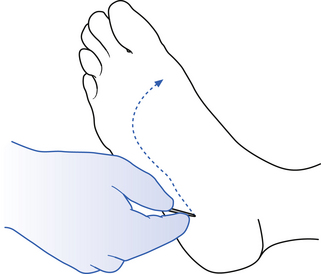
6. The plantar reflex or response (Fig. 4.20) is performed by stroking the plantar aspect of the foot, making sure to curve under the area where the toes join the foot. A normal response involves the toes curling downwards and a mild jerk of the foot away from the stimulus. A positive response, also known as a Babinski response, involves the upward movement of the toes, and in some cases only the big toe moves upwards, which is referred to as an up-going toe. A positive response indicates a lesion to the corticospinal tract on the ipsilateral side below the decussation of the fibres in the medulla, or a contralateral lesion of the corticospinal tracts above the decussation. Commonly, this type of neuron injury is referred to as an upper motor neuron lesion.
Sensory examination of the trunk and limbs
1. Check spinothalamic sensation, which includes pain and temperature in upper and lower limbs. A common mistake made when performing this test is to be too gentle and not actually cause pain. The patient may respond that they felt the stimulus but the stimulus they felt was not pain but pressure. If you are testing pain then it must cause pain to test it.
2. Check dorsal column sensation, which includes two-point discrimination and vibration sense, in upper and lower limbs. A good way to check vibration sense is to use a low C tuning fork, set it ringing, and apply the single pronged end to a distal point on the fingers or toes.
Cerebellar (and further vestibular) examination
1. Observe for the presence of a resting, postural, or kinetic tremor.
2. Instruct the patient to walk on their toes and heels and perform tandem gait.
Physical (visceral) examination
1. Chest—not covered in this text.
Examination of mental state
The patient should be tested for orientation to person: Do they know who they are? place—Do they know where they are? and time—Do they know what day, month, and year it is? One should also test for both short- and medium-term memory by asking the patient to remember a six-digit number and repeat it back immediately and then again after a few minutes have passed and they have been distracted by other testing.
Vestibulocerebellar dysfunction and asymmetry
Autonomic dysfunction and asymmetry
1. Width of palpebral fissure (ptosis)—This is dependent on both sympathetic and oculomotor innervation. Therefore, one needs to differentiate between a Horner’s syndrome, oculomotor nerve lesion, or physiological changes in the CIS of the mesencephalic reticular formation.
2. Skin condition—Increased peripheral resistance may result in decreased integrity of skin, particularly at the extremities.
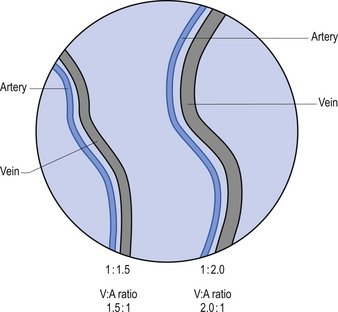
3. Ophthalmoscopy—V:A ratio and vessel integrity.
4. Heart auscultation—Arrhythmias and changes in heart sounds can occur because of altered CIS of the PMRF.
5. Bowel auscultation—This can be particularly useful during some treatment procedures to monitor the effect of stimulation on vagal function (e.g. caloric irrigation—further instruction required, adjustments and visual stimulation or exercises, etc.).
6. Skin and tympanic temperature and blood flow—This is particularly useful as a pre- and post-adjustment check. Profound changes in skin temperature asymmetry can occur following an adjustment. These changes are side dependent. An adjustment on the side of decreased forehead skin temperature will commonly result in greater symmetry or reversed asymmetry. Conflicting results are likely to be dependent on a number of factors, which are currently being investigated further. Remember that forehead skin temperature depends on fuel requirements of the brain, and vestibular and cortical influences on autonomic function, among other things.
7. Dermatographia—The red response is often observed in patients who suffer from sympathetically mediated pain.
8. Lung expansion, respiratory rate and ratio, etc.—An inspiration:expiration ratio of 1:2 is considered to represent approximately normal sympathovagal balance. This means that expiration should take twice as long as inspiration. This is difficult to achieve for some patients at first and requires some training.
Shallow and rapid breathing can result in respiratory alkalosis, which leads to hypersensitivity in the nervous system. CO2 is blown off at a higher rate, resulting in decreased [H+] ions in the blood. Lower [Ca++] follows, causing [Na+] to rise in extracellular fluid. This can be seen clinically by the presence of percussion myotonia, which is also often seen in various metabolic and hormonal disorders.
9. Forehead skin temperature—Measurement of skin temperature above the browline may provide useful information concerning sympathetic control of blood vessels to the eye, as sympathetic supply to the vessels of the forehead are branches of the sympathetic supply to the retinal vessels. Activation of cervical afferents has been found to have an antagonistic effect on the excitatory vestibulosympathetic reflexes. It is therefore proposed that a cervical spine adjustment may enhance cervical inhibition of the vestibulosympathetic reflex, resulting in increased blood flow to the eye and brain (Sexton 2006).
Motor examination of the trunk and limbs
| Upper extremity | Lower extremity |
|---|---|
From Chusid 1964 with permission.
Case 4.1
4.1.1
You would need to examine CN III, V, VII, IX, and X. The examinations one would perform are:
1. Width of palpebral fissure (ptosis)—This is dependent on both sympathetic and oculomotor innervation. Therefore, one needs to differentiate between a Horner’s syndrome, oculomotor nerve lesion, or physiological changes in the CIS of the mesencephalic reticular formation.
2. Skin condition—Increased peripheral resistance may result in decreased integrity of skin, particularly at the extremities.
3. Ophthalmoscopy—V:A ratio and vessel integrity.
4. Heart auscultation—Arrhythmias and changes in heart sounds can occur because of altered CIS of the PMRF.
5. Bowel auscultation—This can be particularly useful during some treatment procedures to monitor the effect of stimulation on vagal function (e.g. caloric irrigation—further instruction required, adjustments and visual stimulation or exercises, etc.).
6. Skin and tympanic temperature and blood flow—This is particularly useful as a pre- and post-adjustment check. Profound changes in skin temperature asymmetry can occur following an adjustment. These changes are side dependent. An adjustment on the side of decreased forehead skin temperature will commonly result in greater symmetry or reversed asymmetry. Conflicting results are likely to be dependent on a number of factors, which are currently being investigated further. Remember that forehead skin temperature depends on fuel requirements of the brain, and vestibular and cortical influences on autonomic function among other things.
7. Dermatographia—The red response is often observed in patients who suffer from sympathetically mediated pain.
8. Lung expansion, respiratory rate and ratio, etc.—An inspiration:expiration ratio of 1:2 is considered to represent approximately normal sympathovagal balance. This means that expiration should take twice as long as inspiration. This is difficult to achieve for some patients at first and requires some training. Shallow and rapid breathing can result in respiratory alkalosis, which leads to hypersensitivity in the nervous system. CO2 is blown off at a higher rate, resulting in decreased [H+] ions in the blood. Lower [Ca++] follows, causing [Na+] to rise in extracellular fluid. This can be seen clinically by the presence of percussion myotonia, which is also often seen in various metabolic and hormonal disorders.
9. Forehead skin temperature—Measurement of skin temperature above the browline may provide useful information concerning sympathetic control of blood vessels to the eye, as sympathetic supply to the vessels of the forehead are branches of the sympathetic supply to the retinal vessels. Activation of cervical afferents has been found to have an antagonistic effect on the excitatory vestibulosympathetic reflexes. It is therefore proposed that a cervical spine adjustment may enhance cervical inhibition of the vestibulosympathetic reflex, resulting in increased blood flow to the eye and brain.
References