History
The Interview
Obtaining a thorough and accurate patient history is truly an art. One important goal of history taking is to establish a good patient-therapist rapport. The patient must be allowed to explain the history in his or her own words and at a comfortable pace.1 If the therapist appears hurried, distracted, preoccupied, irritated, or uncaring; is often interrupted; or fails to be an attentive listener, the patient-therapist relationship will likely suffer.
The interviewer must be careful not to allow personal feelings about the patient’s grooming, appearance, demeanor, or behavior during the interview to unduly question the validity of the chief complaints.2 By the time the patient is referred for physical therapy, he or she may have seen one or more physicians, have been subjected to a number of noninvasive or invasive studies, or have been prescribed oral or inhaled medications with variable or unsatisfactory alleviation of symptoms. The patient is likely to manifest a degree of anxiety and frustration. Therefore, the therapist’s approach, history-taking method, and interviewing style are important for gaining the patient’s confidence and cooperation.
The patient history interview can be divided into the data-gathering and interpretative sections.3 The data-gathering segment begins with asking why the patient has sought medical attention and has been referred for physical therapy services. In other words, what is the patient’s chief complaint—the symptom that caused the patient to seek help?
 Whether the individual is an inpatient or an outpatient. Many inpatients have detailed medical records available for the therapist to review. This reduces the amount of information the physical therapist needs to obtain from the patient during an interview. If the information in the chart is scant, or if the individual is an outpatient with only a treatment referral and few or no medical records available, the physical therapist should obtain a more detailed history.
Whether the individual is an inpatient or an outpatient. Many inpatients have detailed medical records available for the therapist to review. This reduces the amount of information the physical therapist needs to obtain from the patient during an interview. If the information in the chart is scant, or if the individual is an outpatient with only a treatment referral and few or no medical records available, the physical therapist should obtain a more detailed history.
 Whether the treatment order is narrow or broad in scope
Whether the treatment order is narrow or broad in scope
 The acuteness of the patient’s illness, level of consciousness, and ability to provide accurate information
The acuteness of the patient’s illness, level of consciousness, and ability to provide accurate information
Smoking History
The patient should be asked about his or her tobacco-smoking history.3 The number of pack-years of cigarette smoking may be calculated (average number of packs per day multiplied by the number of years smoked) as a relative risk for lung cancer and COPD. Regular smoking of marijuana is more damaging to lung health in the short term as well as potentially long term.4
Family History
The family history is useful in evaluating the possibility of hereditary pulmonary diseases, such as alpha1-antitrypsin deficiency, cystic fibrosis, allergic asthma, hereditary hemorrhagic telangiectasia, and others.5,6 A family history of diabetes, hypertension, coronary artery disease (CAD), or rheumatic fever raises the possibility that these conditions might exist in the patient as well.7
Occupational History
Taking an occupational history is particularly important for pulmonary patients who arrive for physical therapy with little or no accompanying medical information. The internal surface of the lung measures 50 to 100 m3 and is in constant contact with the environment.5 Jobs that involve exposure to silica or silicates (e.g., miners, sandblasters, foundry workers, stone cutters, brick layers, and quarry workers) or other inorganic substances place workers at risk for combinations of obstructive and restrictive lung disease (e.g., silicosis). Construction workers, shipyard workers, pipefitters, and other industrial workers exposed to asbestos are at increased risk for developing a restrictive lung disease such as asbestosis.8 Benign pleural plaques may be found on the diaphragmatic pleurae and bilaterally between the 6th and 10th ribs on the anterolateral or posterolateral chest wall. Progressive pleural thickening rarely occurs. These individuals have an increased incidence of malignant neoplastic diseases such as bronchogenic carcinoma and malignant mesothelioma. Some firefighters, iron workers, and other rescuers working at the World Trade Center disaster site following September 11, 2001, have developed respiratory symptoms and disorders.9,10
Coal workers are exposed to coal mine dust. About 10% have simple pneumoconiosis, whereas a smaller proportion develop the complicated form of the condition—progressive massive pulmonary fibrosis.11
A history of paroxysmal coughing, chest tightness, or dyspnea that is worse during the work week but remits on weekends (or other regular days off work) strongly suggests occupational asthma.11 This condition is difficult to diagnose because symptoms commonly occur several hours after exposure to the provoking agent. Causal agents include grain dusts, wood dusts, formalin, enzyme detergents, ethanolamines (in spray paints and soldering flux), nickel, and hard metals (e.g., tungsten carbide). Workers exposed to cotton flax and hemp dusts may develop byssinosis, an obstructive lung disease. In the early stages, this condition is reversible, but long-term exposure over a number of years causes chronic irreversible obstructive lung disease.
A history of fever, cough, shortness of breath, and recurrent pneumonias in farmers in the northern United States suggests farmer’s lung.11 This is the most common hypersensitive pneumonitis; it is caused by inhaling fungal agents such as thermophilic actinomycetes. Long-term exposure can lead to pulmonary fibrosis. Numerous occupations expose workers to factors that cause hypersensitive pneumonitis.
Questionnaires
Questionnaires can be used in a number of ways. Printed symptom or medical questionnaires can be beneficial or detrimental to the patient-therapist relationship, depending on how they are used. Questionnaires can expedite the data-gathering portion of the initial visit by allowing the patient to note in advance all symptoms, medical conditions, surgeries, occupations, medications, and other factors that may influence physical therapy intervention. They can reduce the amount of nontreatment time therapists may otherwise spend inquiring about irrelevant symptoms and conditions. Printed questionnaires also allow patients sufficient time to recall relevant information and respond more accurately than they often do in an interview setting.5 Used in this way, a printed questionnaire can be a valuable tool for expediting a comprehensive evaluation of cardiopulmonary patients. However, if questionnaires are used improperly, they can depersonalize the history-taking portion of the initial visit.1 If the physical therapist allows the printed form to become a substitute for interaction with the patient, patient satisfaction will be low and the patient-therapist relationship will suffer.
In addition, questionnaires are being increasingly used as standardized outcome measures to assess activity and participation capacity, as well as quality of life and life satisfaction (see Chapter 17). Many questionnaires have been validated and are reliable when used in the clinical setting.
Dyspnea
Dyspnea, commonly referred to as breathlessness or shortness of breath, can be defined as the sensation of difficulty in breathing.12 It is one of the most common reasons for patients to seek medical attention. Dyspnea is difficult to quantitate because it is subjective and at times is normal (i.e., at high altitudes and during or following vigorous exercise). Also, patients of different backgrounds use different descriptors for their breathlessness.13 Dyspnea is a symptom of cardiac and pulmonary diseases, among other conditions.
When a patient complains of shortness of breath or breathlessness, it should be noted that this complaint is often unrelated to the patient’s arterial oxygen level (PaO2). Many times, it appears that altered mechanical factors during breathing contribute to the sensation of breathlessness.14 Numerous receptors that have a role in sensing dyspnea have been identified; they include vagal receptors (e.g., irritant, stretch, and J-receptors), chemoreceptors, proprioceptive receptors (e.g., tendon organs, muscle spindles, joint and skin receptors), and upper airway receptors.3
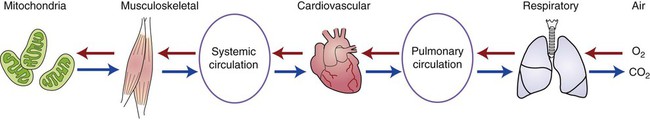
Analyzing the oxygen transport system (Figure 8-1) can help the physical therapist to determine the likely cause of each patient’s dyspnea and the most appropriate physical therapy intervention. The delivery of oxygen from ambient air to the mitochondrion within the cell depends on the intact interaction of the respiratory, cardiovascular, and muscular systems. Also, carbon dioxide (CO2) is eliminated in the opposite direction. Dyspnea can be caused by dysfunction in any of the systems.
Dyspnea commonly occurs when the body’s requirement for breathing (ventilation) exceeds the body’s capacity to provide it.3 In other words, the symptom varies directly with the body’s demand for ventilation and, inversely, with the body’s ventilatory capacity.
There are three basic causes of dyspnea: 12
An increased awareness of normal breathing is usually related to anxiety.5 The patient commonly complains of “not getting a deep enough breath,” a feeling of “smothering,” or “not getting air down in the right places.”15 These sensations have been designated as psychogenic dyspnea. The patient’s breathing pattern is irregular, with frequent sighs. When severe, it is associated with tingling of the hands and feet, circumoral numbness, and lightheadedness. Coaching the patient to hyperventilate and to reproduce the symptoms may help the patient better understand the cause of these symptoms and how to control them.5 The hyperventilation syndrome is properly diagnosed only after organic causes have been excluded and pulmonary function tests indicate normal respiratory mechanics and PaO2.
The time course of the appearance and progression of dyspnea should be identified.6,16 Acute dyspnea is common in pulmonary embolism, pneumothorax, acute asthma, pulmonary congestion related to congestive heart failure (CHF), pneumonia, and upper airway obstruction. Most of these conditions require immediate physician evaluation of the acute problem before physical therapy intervention. Subacute or chronic progression of dyspnea generally presents, over time, as increasingly severe dyspnea with exertion. It occurs with emphysema, restrictive lung disorders such as pulmonary fibrosis, chest wall deformities, respiratory muscle dysfunction, occupational lung diseases, chronic CHF, and large pleural effusions.
Dyspnea may also be related to body position.16 Therefore, when evaluating dyspnea, the physical therapist should ask whether the patient:
 Has difficulty breathing when reclining horizontally
Has difficulty breathing when reclining horizontally
 Finds it necessary to be propped up on several pillows to sleep at night (orthopnea)
Finds it necessary to be propped up on several pillows to sleep at night (orthopnea)
 Has more difficulty breathing when reclining on one side (trepopnea)
Has more difficulty breathing when reclining on one side (trepopnea)
 Wakes up at night short of breath and feels the need to sit up or walk around the room to “catch your breath” (paroxysmal nocturnal dyspnea)
Wakes up at night short of breath and feels the need to sit up or walk around the room to “catch your breath” (paroxysmal nocturnal dyspnea)
Acute Dyspnea
A patient who has acute dyspnea requires a rapid and thorough history and physical assessment. The physical therapist should ask several important questions to address the possible causes of acute dyspnea:14
1. Are you short of breath at rest? If the answer is yes, it suggests a severe physiological dysfunction. The patient likely needs prompt evaluation by a physician if this is of recent onset and the patient has not had a medical workup.
2. Do you have chest pain? If so, what part of your chest? Unilateral localized chest pain raises the possibility of spontaneous pneumothorax, pulmonary embolism, or chest trauma.
3. What were you doing immediately before or at the time of the onset of shortness of breath? Approximately 75% of spontaneous pneumothoraces occur during sedentary activity, 20% happen during some strenuous activity, and 5% are related to coughing or sneezing. A history of immobilization of a lower extremity, recent surgery, bed rest, travel requiring prolonged sitting, obesity, CHF, and venous disease of the lower extremities are all risk factors for pulmonary embolism. If the patient’s symptoms are related to chest trauma, the fact that a fall, a blow, or an accident occurred can usually be quickly established.
4. Do you have any major medical or surgical conditions? Cystic fibrosis, chronic obstructive pulmonary disease (COPD), interstitial lung disease, and malignancies are important causes of secondary spontaneous pneumothorax.
Acute dyspnea in cardiac patients is difficult to assess because the signs and symptoms are so similar to those caused by pulmonary disease. It is most often due to arrhythmias and acute coronary ischemia with associated left ventricular dysfunction, but it can be caused by any cardiac disorder.16
Dyspnea on Exertion
Dyspnea on exertion is a common complaint of patients with cardiopulmonary dysfunction. Dyspnea during exercise or exertion usually precedes dyspnea at rest.17 It most often is a result of chronic pulmonary disease or CHF. Some causes of dyspnea during exertion or exercise are listed in Table 8-1.
Table 8-1
Disorders Limiting Exercise Tolerance, Pathophysiology, and Discriminating Measures
| Disorders | Pathophysiology | Measures That Deviate From Normal |
| PULMONARY | ||
| Obstructive lung disease | ↓ Ventilatory capacity due to airflow limitation, increased ventilatory requirement due to V/Q mismatching, hypoxic stimulation to breathing | ↓ VO2 max, ↑ VD/VT, ↑ P(a–ET)CO2, ↑ P(A–a)O2, ↓ breathing reserve (MVV−VE2 max), ↓ HR at maximal WR (↑ HR reserve), abnormal (trapezoidal) expiratory flow pattern |
| Restrictive lung disease | ↓ Lung volumes, especially IC and TLC; V/Q mismatching, hypoxemia | ↓ VO2 max, ↑ VT/IC, RR >50 at maximal WR, ↓ breathing reserve, ↑ VD/VT, ↑ P(a–ET)CO2, progressively ↓ PaO2 and ↑ P(A–a)O2 with ↑ WRs |
| Chest wall defects | Respiratory pump dysfunction due to muscle weakness or ↓ chest wall compliance | ↓ VO2 max, ↑ VT/IC, ↑ RR at low WRs, nl ΔVO2/ΔWR, ↓ breathing reserve, ↓ HR at maximal WR, nl PaO2 |
| Diseases of pulmonary circulation | ↓ Pulmonary perfusion leading to V/Q mismatching | ↑ VE at submaximal WRs, ↑ VD/VT, ↑ P(a–ET)CO2, progressively ↓ PaO2 and ↑ P(A–a)O2 with ↑ WRs, ↓ VO2 max, ↓ AT, more shallow ΔVO2/ΔWR as WR is ↑ toward maximum, ↓ O2 pulse (VO2 max/HR) |
| CARDIAC | ||
| Coronary insufficiency | Relative imbalance between myocardial oxygen supply and demand, causing myocardial ischemia | May have chest pain and ischemic ECG changes, ↓ VO2 max, ↓ AT, ↓ O2 pulse, more shallow ΔVO2/ΔWR as WR is ↑ toward maximum, ↑ HR/ VO2, ↑ breathing reserve, metabolic acidosis at low WRs → ↑ WRs→VE, abnormal BP responses |
| Valvular | Cardiac output limitation due to ↓ effective SV | ↓ VO2 max, ↓ AT, ↓ O2 pulse, more shallow ΔVO2 max/ΔWR as WR is ↑ toward maximum, ↑ HR/ VO2, ↑ breathing reserve, metabolic acidosis at low WRs → ↑ VE, abnormal BP responses |
| Myocardial | Cardiac output limitation due to ↓ EF and SV | |
| OTHER | ||
| Obesity | ↑ Energy cost to move body; if severe, restrictive lung dysfunction and pulmonary insufficiency | ↑ VO2 per workload, nl O2 pulse when predicted from ht, ↓ VO2 max/wt and AT/wt but nl VO2 max/ht and AT/ht (unless extremely obese), ↑ P(A – a)O2 at rest that normalizes during exercise, nl VD/VT |
| Peripheral arterial disease | Impaired ability to ↑ blood flow to working muscles | Leg pain (claudication), ↓ ΔVO2/ΔWR, ↓ VO2 max, ↓ AT, possible hypertensive BP response |
| Anemia | ↓ Oxygen-carrying capacity | ↓ Hemoglobin and hematocrit, ↓ VO2 max, ↓ AT, ↓ O2 pulse, nl VD/VT, P(a – et)CO2, and P(A – a)O2 |
| Musculoskeletal disorders | Musculoskeletal coupling inefficiency; inflammation | ↓ Mechanical efficiency (VO2 per workload), ↓ maximal WR; possible pain and abnormal movement patterns |
| Chronic metabolic acidosis | Due to poorly controlled DM, CRF, CHF, or ingestion of certain drugs | ↓ HCO3−, steep / VCO2 relationship, nl P(a–ET)CO2 and P(A–a)O2, nl VD/Vt |
| Deconditioning | Inactivity or prolonged bed rest leading to loss of ability to effectively redistribute systemic blood flow | ↓ VO2 max, ↓ AT, ↓ O2 pulse, ↑ breathing reserve, metabolic acidosis at lower WRs → ↑ VE |
| Anxiety reaction | Hyperventilation and respiratory alkalosis with precisely regular RR, although possible breath-holding episodes | Abrupt tachypnea that sometimes starts at rest, ↓ PaCO2, respiratory alkalosis |
| Malingering, poor effort | Very irregular breathing with periods of hyperventilation and hypoventilation | AT not achieved or ↑ compared with VO2 max, ↑ breathing and HR reserve; often irregular breathing pattern with periods of tachypnea and bradypnea producing wide swings in PaCO2 and PetCO2 unrelated to changes in WR |
Data from American Thoracic Society/American College of Chest Physicians ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 167:211–277, 2003; Wasserman K: Dyspnea on exertion. Is it the heart or the lungs? JAMA 248:2039–2043, 1982; Wasserman K, Hansen JE, Sue DY, et al: Principles of Exercise Testing and Interpretation. Philadelphia, 1987, Lea & Febiger; and Weisman IM, Zeballos RJ: An integrative approach to the interpretation of cardiopulmonary exercise testing. Prog Respir Res 32:300–322, 2002. In Watchie J. Cardiovascular and Pulmonary Physical Therapy: A Clinical Manual, ed 2. St. Louis, 2010, Saunders.
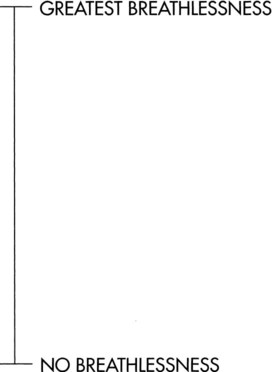
It is important to establish the amount of activity required to produce dyspnea. Various scales18,19 have been developed to categorize the level of dyspnea and impairment present in patients (Figure 8-2 and Table 8-2). The patient should be asked about daily activity and what activities produce breathlessness.20 Does the patient become short of breath climbing a flight of stairs or walking uphill? Is the patient able to walk and talk simultaneously? Does walking more slowly affect the individual’s dyspnea?
Table 8-2
American Thoracic Society Dyspnea Scale
| Grade | Degree | Description |
| 0 | None | Not troubled with breathlessness except with strenuous exercise |
| 1 | Slight | Troubled by shortness of breath when hurrying on level ground or walking up a slight hill |
| 2 | Moderate | Walks slower than people of the same age on level ground because of breathlessness or has to stop for breath when walking at own pace on level ground |
| 3 | Severe | Stops for breath after walking about 100 yards or after a few minutes on level ground |
| 4 | Very severe | Too breathless to leave the house or breathless when dressing or undressing |
Reprinted with permission from Brooks SM: Surveillance for respiratory hazards, ATS News 8:12-16, 1982.
Is wheezing present with the dyspnea on exertion? Has there been an associated weight gain? Does the patient have a positive smoking history and sputum production? If a positive response is received, these suggest that COPD is the primary cause of symptoms.20
The basic defect that cardiac diseases produce during exertion is a limited cardiac output, which is caused primarily by a reduced stroke volume.17 To compensate for the relatively low stroke volume, the patient develops a rapid heart rate and a wide arteriovenous O2 difference (decreased capillary PO2) at an inappropriately low work rate. Therefore the exercising muscles (both skeletal and myocardial) have increased difficulty getting an adequate oxygen supply to perform the necessary work: this results in dyspnea, fatigue, or pain. The lactic acidosis that results from the low level of oxygen delivery to the muscles can be measured by either invasive or noninvasive gas-exchange methods during exercise testing. The functional and therapeutic capacity of the patient with heart disease can be estimated on the basis of the history and symptoms (Table 8-3).
Table 8-3
Functional and Therapeutic Classification of Patients with Heart Disease
| Classification | Parameters |
| Functional Classification | |
| Class I | Patients with cardiac disease but without resulting limitations of physical activity; ordinary physical activity does not cause undue fatigue, palpitation, dyspnea, or anginal pain. |
| Class II | Patients with cardiac disease resulting in slight limitation of physical activity; they are comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnea, or anginal pain. |
| Class III | Patients with cardiac disease resulting in marked limitation of physical activity; they are comfortable at rest. Less than ordinary physical activity causes fatigue, palpitation, dyspnea, or anginal pain. |
| Class IV | Patients with cardiac disease resulting in inability to carry on any physical activity without discomfort; symptoms of cardiac insufficiency or of the anginal syndrome may be present even at rest. If any physical activity is undertaken, discomfort increases. |
| Therapeutic Classification | |
| Class A | Patients with cardiac disease whose physical activity need not be restricted in any way. |
| Class B | Patients with cardiac disease whose ordinary physical activity need not be restricted but who should be advised against severe or competitive efforts. |
| Class C | Patients with cardiac disease whose ordinary activity should be moderately restricted and whose more strenuous efforts should be discontinued. |
| Class D | Patients with cardiac disease whose ordinary activity should be markedly restricted. |
| Class E | Patients with cardiac disease who should be at complete rest, confined to bed or chair. |
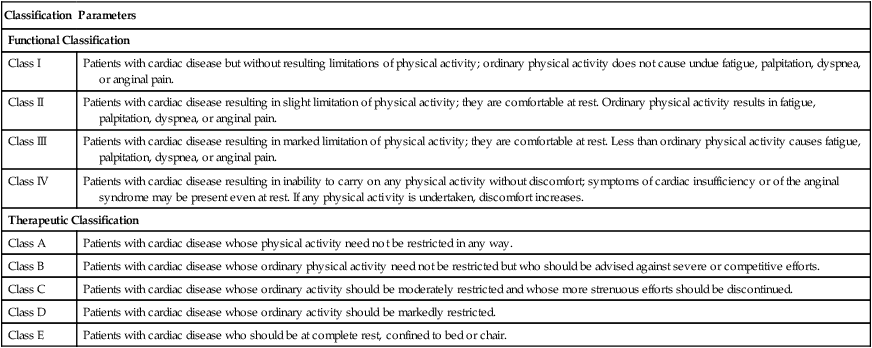
Reprinted with permission from the New York Heart Association: Diseases of the heart and blood vessels: Nomenclature and criteria for diagnosis, ed 6, Boston, 1964, Little, Brown.
Diseases that involve the lungs or thoracic cage generally prevent external respiration (ventilation) from keeping pace with internal respiration (in the cells).17 In other words, patients outwalk or outrun their lungs during activities or exertion. The primary symptom that limits exercise in patients with pulmonary disorders is dyspnea, which occurs because of the difficulty they have eliminating the CO2 produced by metabolism. Some individuals, such as those with pulmonary fibrosis and some of those with COPD, do experience a decrease in PO2 with exercise. Hence dyspnea on exertion in pulmonary patients is usually related to hypoxic or hypercapnic stimuli.
Dyspnea in Cardiac Patients
The cause of dyspnea in cardiac patients is determined by whether an associated stiffness of the lungs (a loss of compliance) is also present.15 Dyspnea is the primary symptom of a decompensating left ventricle.7,16 As the ventricle fails to eject the normal volume of blood, it produces chronic pulmonary venous hypertension, congestion, and pulmonary edema, resulting in stiff or less compliant lungs. This, along with modest hypoxemia that augments the respiratory drive, increases ventilation and the work of breathing. Tachypnea is often seen at rest. Exercise exaggerates the pulmonary congestion and edema and promotes arterial and mixed venous hypoxemia, which also increases the amount of dyspnea and tachypnea manifested. Fatigue, resulting from low cardiac output, also affects the respiratory muscles, further increasing the sensation of breathlessness.
Dyspnea in cardiac patients without stiff lungs is seen primarily during exertion or exercise.15 In uncomplicated pulmonic stenosis, it is probably related to an inadequate cardiac output during exercise. Patients with tetralogy of Fallot and other forms of cyanotic heart disease experience both dyspnea and fatigue during exercise when the arterial oxyhemoglobin saturation has fallen appreciably below the resting level.
Paroxysmal Nocturnal Dyspnea
Paroxysmal nocturnal dyspnea (PND) is an important type of shortness of breath. This symptom has strong predictive value as a sign of CHF.1 The patient usually falls asleep in the recumbent position, and 1 or 2 hours later, awakens from sleep with acute shortness of breath. The patient sits upright on the side of the bed or goes to an open window to breathe “fresh air” and get relief from shortness of breath.
The mechanism of PND is the transfer of fluid from extravascular tissues into the blood stream (or intravascularly) during sleep.20 The intravascular volume of fluid gradually increases until the compromised left ventricle can no longer manage it. The left atrial pressure rises when the rate of lymphatic drainage from the lungs is unable to keep up with the increased volume of fluid. The increased atrial pressure leads to a sufficiently elevated pulmonary capillary pressure to produce interstitial edema. Patients who are light sleepers awaken early with dyspnea. Deep sleepers may not awaken until they develop alveolar edema.
Platypnea
Platypnea is the onset of dyspnea when the patient assumes the sitting position from the supine position.6,16 This unusual phenomenon is commonly found in patients with basilar pulmonary fibrosis or basilar arteriovenous malformation. It can be related to the redistribution of blood flow to the lung bases when assuming the sitting position and the resultant ventilation-perfusion mismatching and hypoxemia.
Trepopnea
Trepopnea refers to dyspnea in one lateral position but not the other.3 It is caused by the positional mismatching of ventilation to perfusion in unilateral respiratory system pathology such as lung disease, pleural effusion, or airway obstruction.16,21,22 It also is commonly seen in patients with mitral stenosis.20 Occasionally, it may be the result of a fall in blood pressure when the patient is in the left lateral decubitus position. If the patient has ischemic heart disease, the reduction in coronary perfusion can cause either angina or dyspnea.
Functional Dyspnea
Functional dyspnea is defined as shortness of breath at rest but not during exertion.6 It is most commonly seen in young women who complain of the need to take a deep breath or to sigh, and they interpret this sensation as shortness of breath. The physical examination and pulmonary function tests are negative. Reassurance is usually all that is necessary.
Wheezing
Patients who complain of wheezing associated with dyspnea may have pulmonary or cardiac disease. This symptom, if first reported in patients over the age of 40, is often related to heart failure.1 When it has been confirmed that the wheezing results from heart disease, the patient is said to have cardiac asthma. Wheezing in cardiac patients is a manifestation of narrowed airways and thickened bronchial walls as a result of pulmonary edema.15 However, if patients have a history of episodes of wheezing and dyspnea since childhood, COPD or asthma is the likely cause. Other pulmonary conditions, such as eosinophilic pneumonia, bronchopulmonary aspergillosis, allergic granulomatosis, and others can cause wheezing.5 Wheezing must be differentiated from stridor, which is commonly caused by laryngotracheal narrowing due to a tracheostomy scar, trauma of intubation, laryngeal paralysis, epiglottitis, or tumors. Chronic pulmonary patients may also develop heart conditions, so it is good to remember that patients who complain of wheezing may have both cardiac and pulmonary disease.
Cough
Cough is a common symptom of pulmonary disease. The cough mechanism consists of three phases:23
Numerous cough-irritant receptors are located on the mucosa of the larynx, trachea, bronchi, pleura, and external auditory canal. These receptors are most sensitive at the glottis and carina and diminish rapidly beyond the fourth-generation bronchi. A cough follows stimulation of these mucosal receptors by any of a number of factors including inflammation, sputum, foreign bodies, noxious gases or odors, chemical substances, endobronchial tumors, and extrabronchial pressure on the trachea or bronchi.6
A productive cough is beneficial for clearing the airways of sputum and foreign material and generally should not be inhibited. However, a dry, hacking cough is usually of no value and can have a self-perpetuating irritant effect on the respiratory mucosa. A dry cough may be the initial symptom of certain interstitial lung diseases such as allergic alveolitis, sarcoidosis, and pulmonary fibrosis. Some causes and characteristics of coughs are listed in Table 8-4.
Table 8-4
Some Causes and Characteristics of Coughs
| Cause | Characteristics |
| Acute Infections of Lungs | |
| Tracheobronchitis | Cough associated with sore throat, running nose and eyes |
| Lobar pneumonia | Cough often preceded by symptoms of upper respiratory infection; cough dry, painful at first; later becomes productive |
| Bronchopneumonia | Usually begins as acute bronchitis; dry or productive cough |
| Mycoplasma and viral pneumonia | Paroxysmal cough, productive of mucoid or blood-stained sputum associated with influenza-like syndrome |
| Exacerbation of chronic bronchitis | Cough productive of mucoid sputum becomes purulent |
| Chronic Infections of Lungs | |
| Bronchitis | Cough productive of sputum on most days for more than 3 consecutive months and for more than 2 successive years; sputum mucoid until acute exacerbation, when it becomes mucopurulent |
| Bronchiectasis | Cough copious, foul, purulent, often since childhood |
| Tuberculosis or fungus | Persistent cough for weeks to months, often with blood-tinged sputum |
| Parenchymal Inflammatory Processes | |
| Interstitial fibrosis and infiltrations | Cough nonproductive, persistent; depends on causes |
| Smoking | Cough usually associated with injected pharynx; persistent, most marked in morning, usually only slightly productive unless succeeded by chronic bronchitis |
| Tumors | |
| Bronchogenic carcinoma | Nonproductive to productive cough for weeks to months; recurrent small hemoptysis common |
| Alveolar cell carcinoma | Cough similar to bronchogenic carcinoma, except in occasional instances when large quantities of watery, mucoid sputum are produced |
| Benign tumor in airways | Cough nonproductive, occasionally hemoptysis |
| Mediastinal tumor | Cough, often with breathlessness, caused by compression of trachea and bronchi |
| Aortic aneurysm | Brassy cough |
| Foreign Bodies | |
| Immediate, while still in upper airway | Cough associated with progressive evidence of asphyxiation |
| Later, when lodged in lower airway | Nonproductive cough, persistent, associated with localizing wheeze |
| Left ventricular failure | Cough intensifies while body is supine; aggravation of dyspnea |
| Pulmonary infarction | Cough associated with hemoptysis, usually with pleural effusion |
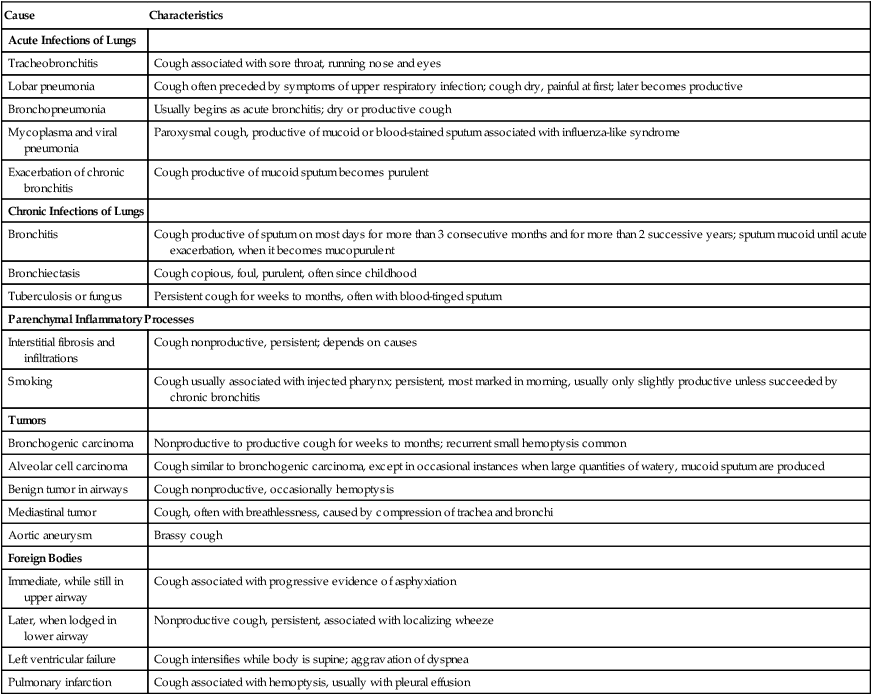
Reprinted with permission from Szidon J, Fishman A: Approach to the pulmonary patient with respiratory signs and symptoms. In Fishman A, editor: Pulmonary diseases and disorders. New York, 1988, McGraw-Hill.
Cough may be the only presenting symptom of asthma and is a common cause of chronic cough.24,25 In individuals with asthma, cough is precipitated by inhaling cold air and by exercising, and the cough is dry. Cough can precipitate an asthma attack in sensitive patients; in that instance, it is known as cough-induced bronchospasm.
It is important to determine the length of time cough has been present.6 The most common cause of an acute cough is a viral respiratory infection, which generally resolves within a few days or 2 to 3 weeks. Exposure to noxious gases also precipitates acute coughing.
A cough that has persisted for more than 3 weeks can be termed chronic.3 The most common cause of chronic cough is chronic bronchitis, which is present in up to 30% of cigarette smokers. The next most common cause is the postnasal discharge syndrome. Patients describe a sensation of secretions dripping from the back of the nose into the throat, prompting throat clearing or coughing. Gastroesophageal disorders are present in 10% to 40% of patients with chronic cough and may contribute to coughing due to microaspiration or irritation of cough receptors in the lower esophagus.25–27
Various cardiac conditions may stimulate receptors in the bronchi and provoke coughing.28 Because the bronchial veins empty into the pulmonary veins (leading to the left side of the heart), the systemic veins, and the superior vena cava (leading to the right side of the heart), venous congestion and coughing may occur with either right- or left-side CHF. It is more common, however, in left-sided CHF. The onset of a cough in a patient with paroxysmal tachycardia or acute myocardial infarction (MI) is often an early symptom of acute left-side heart failure.
A specific diagnosis can be made in 80% of cases of chronic cough by an appropriate history alone.29 Determining the precipitating causes or the time of onset points the clinician to a probable diagnosis. For example, does the patient cough primarily at night? If so, it points to heart failure, esophageal problems, bronchiectasis, or asthma as the potential cause. An early-morning cough is more common in bronchitis and in individuals with postnasal drip. Cough following meals suggests esophageal disease. Cough precipitated by exertion or deep breathing suggests asthma or interstitial lung disease. Allergens or irritant fumes at home or at work may be a cause of cough. Postviral cough may be present for weeks following a viral illness.
Cough Complications
One of the more common complications of cough is syncope. Tussive, or cough-induced, syncope, which is more common in men than in women, can be recognized through accurate history taking.5 It is typically reported by middle-aged men who “smoke hard, eat hard, drink hard, and cough hard.” They experience fainting or near-fainting following cough paroxysms. The cause is obscure but may be related to vagus-induced cardiac slowing or vasodilation or to high intrathoracic pressures that impair venous return, decrease cardiac output, increase intracranial pressure, and result in a reduced cerebral blood flow. Cough syncope is often resolved by smoking cessation.
Complications of cough include headache, back pain, muscular tears, hematomas, and rib fractures (along the posterior axillary line). Occasionally, vertebral compression fractures (in osteopenic patients), urinary incontinence (UI) (in women), and inguinal hernias (in men) may occur.30
Chest Pain
Taking an accurate history is crucial to the proper evaluation of chest pain.3 Although the definitive cause of chest pain cannot be fully established without diagnostic medical tests, it is usually possible to determine whether the pain originates in the pleurae, chest wall, or thoracic organs by means of careful history taking.
Pleuritic Chest Pain
Pleuritic chest pain originates from the parietal pleura or endothoracic fascia but not the visceral pleura, which have no pain receptors. The patient can usually identify it as being close to the thoracic cage.15 Pleuritic chest pain worsens sharply with inspiration as the inflamed parietal pleura are stretched with chest wall motion. Deep breathing, coughing, and laughing are extremely painful, requiring the patient to apply pressure over the involved area to control the pain.
Pleuritic chest pain is ordinarily found in patients who have other signs of respiratory illness, such as cough, fever, chills, and malaise. Inflammation of the central portion of the diaphragmatic pleura produces ipsilateral shoulder pain by way of the phrenic nerve.5 Outer portions of the diaphragmatic pleura are innervated by the 7th through 12th intercostal nerves. Irritation of these pleura causes referred pain in the lower thorax or upper abdomen.31
The onset of pleuritic chest pain varies according to its cause.3 Sudden severe pleuritic chest pain suggests a spontaneous pneumothorax, pulmonary embolism, or infarct. Pulmonary embolism is usually accompanied by sudden dyspnea, hemoptysis, tachycardia, cyanosis, hypotension, anxiety, and agitation.7
Cardiac Chest Pain
Three cardinal features are characteristic of cardiac chest pain. The patient should be asked the following questions:7
1. Does the pain have maximal intensity from the onset or does it build up for several seconds? Ischemic cardiac pain, or angina, is caused by the myocardium contracting in the absence of an adequate oxygen supply. The same type of pain can be produced by placing a blood pressure cuff around the upper arm and inflating it until the brachial pulse can no longer be palpated at the wrist. If a patient opens and closes a fist, pain will gradually appear and escalate in the forearm. The causal mechanism of this pain is the same as that of myocardial pain: continuing muscular contraction in the absence of an adequate oxygen supply. This type of pain requires several contractions of the myocardium to reach its maximal intensity. In other words, there is a characteristic buildup, or escalation, of angina pain.
2. Can you point to the area of pain with one finger? Anginal pain is characteristically demonstrated by patients’ using their entire hand or closed fist against the anterior chest wall. It is described as a sign of angina because it is so typical.7 By contrast, any pain that can be localized by pointing with a fingertip is unlikely to be angina.
3. Is the pain deep inside your chest, or does it seem as though it is close to the surface? Anginal pain is visceral pain that may be referred superficially but always has a deep internal component.
Angina is not limited to patients with CAD.7 Individuals who have normal coronary arteries but an insufficient oxygen supply for a given cardiac workload can also experience angina. These include individuals with anemia, hypertension, tachycardia, and thyrotoxicosis. Hypertrophic and dilated cardiomyopathy can produce typical angina pain, although the latter tends to be intermittent, usually occurring with episodes of CHF. Aortic valve disease can cause angina as a result of impairment of adequate coronary artery blood flow.
Angina is usually precipitated by exertion, such as walking uphill, against the wind, or in cold weather.7 It is more likely to be brought on after a meal or by emotional stress. The rapid resolution of chest pain by rest or sublingual nitroglycerin strongly suggests a cardiac origin. The pain produced by MI is longer, persisting more than 20 minutes; it occurs at rest and is accompanied by nausea, diaphoresis, hypotension, and dyspnea.
Pulmonary Hypertension
Chest pain related to pulmonary hypertension may mimic angina pectoris. It is usually found in patients with mitral stenosis or Eisenmenger syndrome (pulmonary hypertension related to an interventricular septal defect, a patent ductus arteriosus, or an atrial septal defect). This type of chest pain usually is absent at rest, occurs during exertion, and is invariably associated with dyspnea.1 It is believed to result from dilation of the pulmonary artery or from right ventricular ischemia. The pain is not relieved by nitrates. Primary pulmonary hypertension may be accompanied by syncope and the Raynaud phenomenon.6
Pericardial Chest Pain
Pericardial chest pain is also midline, but because of its anatomic relationship with the mediastinal pleura, it has features that suggest pleural involvement.3 Deep breathing, coughing, swallowing, movement, and lying down may make it worse. If the central tendon of the diaphragm is involved, the pain may be referred to the left shoulder or scapular area.7 The patient may report that each heartbeat affects the pain. Sitting up and leaning forward or lying on the right side often relieves the pain.
Esophageal Chest Pain
Diffuse esophageal spasm or esophageal colic is a common cause of chest pain. It is often confused with cardiac pain because it is located substernally, has a squeezing or aching quality, and may radiate into one or both arms.12 Furthermore, diffuse esophageal spasm may be relieved by sublingual nitroglycerin as a result of its generalized function as a smooth-muscle relaxant.
Pain that radiates through the chest to the back, pain that decreases with a change in position from supine to upright, or relief induced by ingesting antacids all suggest an esophageal origin.3 Also, diffuse esophageal spasm is often associated with pain on swallowing (odynophagia), dysphagia, and regurgitation of stomach contents. Swallowing hot or cold liquids and emotional stress tend to precipitate this type of chest pain.
Chest Wall Pain
Chest wall pain is the most common type of chest pain. Clues in the patient’s history to this type of pain include intermittent occurrence, variable intensity, and local tenderness.5 Because it is commonly located on the anterior chest wall, many patients believe it is heart pain. However, an important differentiation from cardiac pain is that it does not occur during, but rather following, exertion. It may worsen with inspiration, but its association with trunk motions (flexion, extension, rotation) distinguish it from pleuritic chest pain.
Localized anterior chest pain as a result of costochondritis of the second to fourth costosternal articulations (Tietze syndrome) is described as tender to touch.12 A complaint of rib tenderness, together with a history of trauma, fall, long-term steroid use, coughing, or upper extremity exertion, suggests rib fracture.
Degenerative disk disease and arthritis of the cervical or thoracic spine, thoracic outlet syndrome, spondylitis, fibromyalgia, kyphoscoliosis, and herpes zoster can all produce chest wall pain.3,5,32–34 Primary lung cancer that invades the adjoining chest wall, ribs, or spine produces severe, persistent, localized pain.3 Another possible cause of chest wall pain is the Pancoast syndrome (superior sulcus tumor), in which a primary lung tumor located in the extreme apex of the lung invades the brachial plexus and produces pain in the shoulder, scapular region, or medial aspect of the arm and hand.
Chest wall pain may be caused, rarely, by thrombosis of a superficial vein on the chest wall (Mondor’s disease). It is a self-limited condition of unknown origin and can last several weeks.3 The only physical finding is a subcutaneous cord that can be palpated along the lateral chest wall.
Hemoptysis
The timing and frequency of hemoptysis, as determined in the history, can offer clues about its cause. A history of nosebleeds is significant because blood may be aspirated during sleep at night and expectorated the following morning. Intermittent bouts of hemoptysis are characteristic of respiratory infections such as bronchiectasis, tuberculosis, fungus infections, or broncholithiasis.5 Persistent expectoration of blood-streaked sputum on a daily basis is highly suggestive of bronchogenic neoplasm.
The lung receives its blood supply in two ways: the pulmonary arteries (a low-pressure system) and the bronchial arteries (a high-pressure system) off the aorta.6 The appearance of hemoptysis may vary according to which blood supply is involved. If the bronchial vessels are the source, there tend to be large amounts of bright-red blood. This is often the site of bleeding in bronchiectasis, because bronchial arteries undergo enlargement and extensive anastomosis with the pulmonary artery system. In mitral stenosis, where there is increased pulmonary vascular resistance, hemoptysis arises from passively engorged submucosal bronchial veins.15
Hemoptysis sourced in the low-pressure pulmonary artery system tends to occur in small amounts and is composed of dark or clotted venous blood.3 It may arise from the pulmonary parenchyma, as in the case of the highly vascular granulation tissue found in the walls of lung abscesses. These abscesses may be caused by infections, such as tuberculosis, anaerobic bacteria, staphylococci, or chronic irritation by a fungus ball in an abscess cavity. If a blood vessel ruptures in an abscess cavity, hemorrhage tends to be massive, even exsanguinating.
Cardiovascular conditions, such as mitral stenosis, pulmonary infarction, Eisenmenger physiology, and aortic aneurysm, are also associated with hemoptysis.1 Pink frothy sputum is commonly found with acute pulmonary edema. Physical therapists should carefully evaluate complaints of hemoptysis and be certain of its cause before cautiously conducting treatment.
Fatigue and Weakness
There are multiple causes of fatigue and weakness.1 Physical therapists should not conclude too quickly that they are related to physical inactivity and decreased muscular strength in sedentary cardiopulmonary patients. The most common causes of complaint of fatigue and weakness are depression, anxiety, and emotional stress. They often accompany anemia, hypothyroidism, and chronic disease states.
Fatigue is commonly associated with CHF. In this condition, it is probably related to cardiac output insufficient to perfuse the entire body adequately, including the skeletal muscles. Generally, fatigue caused by cardiac disease is related to exertion, but fatigue related to anxiety tends to be continuous.1
Pedal Edema
CHF is a common cause of bilateral pedal edema.7 However, 10 to 20 pounds of fluid generally accumulate in the body before foot and ankle swelling is evident. Therefore weight gain is an even earlier indication of fluid retention due to CHF. Occasionally, patients may complain only about an increase in abdominal girth, which results from ascites. When caused by CHF, the onset of ascites virtually always occurs after pedal edema is present. If the amount of ascites is disproportionate to that of pedal edema, restrictive cardiomyopathy or constrictive pericarditis should be a consideration.
Patients with CHF and altered renal function commonly report edema of the ankle and lower legs while upright during the day, but indicate a decrease during the night.1 This is a result of local hydrostatic factors related to the upright position.
Hoarseness
Hoarseness (abnormal vocal cord motion during phonation) is a symptom of laryngeal dysfunction.5 It is usually associated with upper respiratory tract infections or allergies and resolves in 1 to 2 weeks.6 Trauma following intubation, laryngeal polyps, or tumors are other common causes of hoarseness. However, this symptom is also related to cardiopulmonary conditions. Because the recurrent laryngeal nerves pass through the upper thorax, intrathoracic pathology that involves one of these nerves can cause unilateral vocal cord paralysis, resulting in hoarseness.6 These include lung or mediastinal tumors, granulomatous disease, enlarged mediastinal lymph nodes, and pericardial or mediastinal adhesions.
Several cardiovascular conditions can produce hoarseness because the left recurrent laryngeal nerve loops under the arch of the aorta and above the pulmonary artery as it returns to the neck.1 Therefore an aneurysm of the arch of the aorta, a dilated pulmonary artery or atrium resulting from an atrial septal defect, or mitral stenosis can cause hoarseness.28