CHAPTER 18 Hirschsprung Disease
Transanal Pull-Through
Step 1: Surgical Anatomy
♦ Three important landmarks to consider for transanal pull-through:
 The anorectal squamocolumnar junction (dentate line)—The mucosal incision should be made high enough that the transitional epithelium is preserved. If this epithelium is damaged, sensation will be abnormal and continence will be impaired.
The anorectal squamocolumnar junction (dentate line)—The mucosal incision should be made high enough that the transitional epithelium is preserved. If this epithelium is damaged, sensation will be abnormal and continence will be impaired.
 The anorectal squamocolumnar junction (dentate line)—The mucosal incision should be made high enough that the transitional epithelium is preserved. If this epithelium is damaged, sensation will be abnormal and continence will be impaired.
The anorectal squamocolumnar junction (dentate line)—The mucosal incision should be made high enough that the transitional epithelium is preserved. If this epithelium is damaged, sensation will be abnormal and continence will be impaired.♦ The location of the pathological transition zone should be determined before beginning the anal dissection.
♦ In children with a more proximal transition zone, the normally innervated bowel might not reach the anus. In these cases a number of maneuvers can be performed, including dividing the lateral attachments of the descending colon, taking down the splenic flexure, and dividing mesenteric vessels proximally so that blood supply is maintained via the marginal vessels.
Step 2: Preoperative Considerations
♦ The diagnosis of Hirschsprung disease is suspected based on the clinical picture of intestinal obstruction, constipation, or enterocolitis. A contrast enema often shows a “transition zone.” However, around 10% of newborns with rectosigmoid Hirschsprung disease and all children with total colonic aganglionosis do not exhibit this finding.
♦ The diagnosis must be confirmed with a rectal biopsy reviewed by an experienced pathologist. The biopsy should be obtained from the posterior wall of the rectum about 1 cm proximal to the anorectal squamocolumnar junction (dentate line). The diagnosis is based on the absence of ganglion cells in an adequate specimen. A false-positive diagnosis may occur if the biopsy is taken too close to the dentate line or if there is not enough submucosa. There is controversy regarding the need for routine cholinesterase staining.
♦ Between the initial diagnosis of Hirschsprung disease and the definitive operation, rectal stimulations and irrigations should be performed as needed. If necessary, the infant can be discharged and scheduled for an elective operation at a later date. If this course is chosen, the parents must be taught how to perform rectal stimulations or irrigations before discharge and must be educated to recognize the signs of enterocolitis.
♦ In premature infants, it may be difficult for the pathologist to interpret a rectal biopsy because of the prematurity of the ganglion cells. These infants should be managed with rectal stimulation or irrigations or both until term, when a suction biopsy can be obtained.
♦ If long-segment Hirschsprung disease is suspected based on a radiologic transition zone extending proximal to the midtransverse colon or into the small bowel, we recommend performing a diverting stoma in the normally innervated colon or small bowel, followed by a Duhamel pull-through at a second stage after the stool has thickened.
Step 3: Operative Steps
Anesthesia
Position
♦ The infant is placed in lithotomy position, with the legs abducted at the hip joint and support under the knees to gain access to both the anus and to the abdomen.
♦ The infant is moved to the foot of the table so that the operating surgeon can sit on a stool below the child.
Leveling Biopsy
♦ We begin by making a supraumbilical incision, opening the fascia in a transverse fashion, including ligation and division of the umbilical vein.
♦ A Hegar dilator is carefully introduced through the anus and used to push the sigmoid colon toward the umbilical incision, where it is grasped with a Babcock clamp (Fig. 18-1). Care is taken to identify which part of the sigmoid is proximal and which is distal.
♦ A full-thickness biopsy is obtained from the antimesenteric border of the colon for immediate frozen-section evaluation. The biopsy site is closed using a running 4-0 PDS in a single layer, and the tail is left long for easy identification if additional biopsies are necessary. If a transition zone is identifiable by direct vision, the first biopsy is taken about 2 cm proximal to the transition zone. It must be recognized that the pathological transition zone is sometimes more proximal than either the grossly visible or radiologically evident transition zone.
♦ While waiting for the results of the frozen section, the mesentery to the colon distal to the biopsy can be divided either by ligation or by bipolar cauterization close to the bowel wall (Fig. 18-2).
♦ If the initial biopsies are aganglionic, additional biopsies must be obtained more proximally until normal ganglion cells are found.
Pull-Through
♦ Four 4-0 silk sutures are placed to evert the anus (Fig. 18-3). Some surgeons prefer the Lonestar retractor, but we find that it tends to tear through the tissue in infants and is therefore more traumatic.
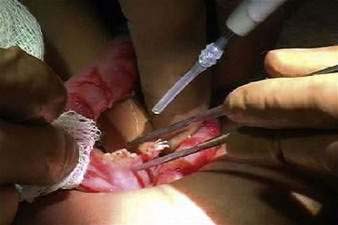
♦ With a nasal speculum in the anus, a circumferential mucosal incision is made using a needle-tip cautery (Fig. 18-4). The mucosal incision should be made 0.5 cm above the dentate line in an infant and up to 1.0 cm above the dentate line in an older child.
♦ Multiple 4-0 silk sutures are placed into the proximal edge of the mucosal incision for retraction. These sutures are brought together and secured with one straight hemostat.
♦ The dissection of the muscular cuff then proceeds using the needle-tip cautery (Fig. 18-5). The correct plane is in the submucosa, between the mucosa and the circular muscle fibers. It has a white appearance and is relatively avascular.
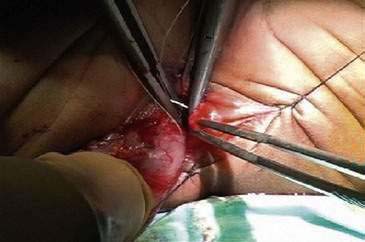
♦ The submucosal dissection is carried proximally for approximately 2 cm. At this point the muscular cuff is incised and divided circumferentially (Fig. 18-6), taking care to stay immediately on the outside of the rectal muscle.
♦ The dissection then proceeds proximally on the outside of the rectum, again taking care to stay immediately on the outside of the rectal muscle (Fig. 18-7). The rectal blood supply is divided as it enters the wall of the bowel. Most blood vessels can be “pinch-burned” (cauterized) and then transected. Larger vessels can be ligated and divided.
♦ Eventually the peritoneal reflection is encountered and divided so that the bowel that is pulled through is intraperitoneal. At this point, it is important to maintain the orientation of the rectum so that it is not twisted. A Kelly clamp can be placed in the vertical plane to maintain the orientation, which will prevent inadvertent 360-degree rotation of the bowel. Some surgeons also place sutures periodically along the antimesenteric surface of the rectum to ensure correct orientation.
♦ When the leveling biopsy site (proximal to the transition zone with confirmed ganglion cells) has been reached, the pull-through is extended for another 2 to 3 cm proximally to ensure that the transition zone is not included in the anastomosis (Fig. 18-8).
♦ The anterior half of the circumference of the normally innervated bowel is transected. The anastomosis is performed using interrupted 4-0 Vicryl sutures, starting with the 12, 3, and 9 o’clock positions. Bowel transection is then completed, the specimen passed off the field, and the 6 o’clock stitch is placed. The rest of the anastomosis is performed using a “divide and conquer” technique, bisecting the space between the initial stitches and then continuing to divide the spaces between sutures until the anastomosis is complete. It is important to obtain full-thickness bites of the pulled-through colon and generous bites of the underlying muscle on the distal rectum. It is also critical to ensure that the distal bites include only rectal mucosa and not transitional epithelium or skin (Fig. 18-9).
Closure
♦ After changing gloves and gowns, the surgeon closes the umbilical incision. We use a single layer of running 3-0 PDS, starting from both ends and working toward the middle.
Step 4: Postoperative Care
♦ Postoperatively the infant is observed for post-anesthesia problems, as well as for evidence of bleeding, abdominal distention, or fever.
♦ Feeding can be started as soon as the infant arrives in the nursery unit or on the surgical ward. We usually start with clear fluids such as a pediatric oral electrolyte solution and advance to a regular diet as tolerated.
♦ Postoperative pain is managed with 10 mg/kg of acetaminophen given orally every 4 hours. In unusual cases, particularly if the caudal block was not effective, intravenous narcotics may be necessary.
♦ The infant can be discharged home as soon as there is evidence of bowel function and toleration of full feedings.
♦ Before the infant is discharged, detailed instructions are provided with regard to signs and symptoms of enterocolitis, which can occur even within the first week postoperatively. Enterocolitis is the most common reason for readmission and is the most common cause of death in patients who have undergone a pull-through for Hirschsprung disease.
♦ The parents should also be instructed about how to prevent perineal excoriation from the frequent and loose bowel movements that most children experience early after a pull-through. Routine protection of the perineal skin with Ihle’s paste (a 25% zinc oxide–based barrier) and stoma powder is commonly recommended, although many other effective barrier creams exist. A stomal therapist can be very helpful in providing support and advice to the parents with respect to this common problem.
♦ The first postoperative visit is in 7 to 14 days. At this visit we calibrate the anastomosis using Hegar dilators. In infants a no. 10 dilator is adequate, and in older children a no. 12 Hegar should easily pass through the anastomosis. A small amount of bleeding can be expected. The patient is brought back again weekly over the next 6 to 8 weeks for calibration as the anastomosis heals. Although many surgeons instruct parents to dilate the anastomosis postoperatively on a daily basis, we use this approach only if the anastomosis is tight during the weekly calibration.
Step 5: Pearls and Pitfalls
♦ An accurate histologic diagnosis is necessary before a pull-through is performed. If there is any question about the diagnosis, the pull-through should be performed at a later time after multiple full-thickness leveling biopsies have been obtained and the samples have been examined by an experienced pathologist.
♦ For surgeons who prefer the use of laparoscopy to the umbilical incision, the operation is essentially the same as described above.
♦ Children who initially have profound malnutrition, severe enterocolitis, or massively dilated proximal bowel should be managed with a preliminary colostomy in normally innervated colon. Once the reason for the colostomy has resolved, the child can still undergo a transanal pull-through. In this situation the colostomy in taken down and used as the pull-through bowel. The rest of the procedure is done as described above.
♦ For children with long-segment Hirschsprung disease, we prefer to perform a Duhamel procedure rather than a transanal pull-through. If the transition zone is proximal to the midtransverse colon during the leveling biopsies, we bring a colostomy or ileostomy in normally innervated bowel. In most cases, the stoma is brought out through the umbilical incision. The umbilical incision can be used again when the colectomy and pull-through are ultimately performed, resulting in an excellent cosmetic appearance.
♦ The transanal pull-through is more difficult and treacherous in a child with massive dilatation of the rectum. This can be particularly problematic in older children (older than 2 years) with a delayed diagnosis and short-segment disease, in whom the rectum is both dilated and thickened. In these children, a Duhamel procedure may be a better choice.
♦ Attention to the technical details is extremely important to ensure a good outcome. These details include the following:
 Avoid stretching of the sphincter during the dissection. This is accomplished by pulling the bowel firmly down so that the operation is done outside the anus rather than placing retractors within the anus and stretching the sphincter unnecessarily.
Avoid stretching of the sphincter during the dissection. This is accomplished by pulling the bowel firmly down so that the operation is done outside the anus rather than placing retractors within the anus and stretching the sphincter unnecessarily.
 Avoid stretching of the sphincter during the dissection. This is accomplished by pulling the bowel firmly down so that the operation is done outside the anus rather than placing retractors within the anus and stretching the sphincter unnecessarily.
Avoid stretching of the sphincter during the dissection. This is accomplished by pulling the bowel firmly down so that the operation is done outside the anus rather than placing retractors within the anus and stretching the sphincter unnecessarily.Dasgupta R, Langer JC. Transanal pull-through for Hirschsprung’s disease. Semin Pediatr Surg. 2005;14:64-71.
Langer JC, Durrant AC, de la Torre ML, et al. One-stage transanal Soave pull-through for Hirschsprung’s disease: a multicenter experience with 141 children. Ann Surg. 2003;238:569-576.
Nasr A, Langer JC. Evolution of the technique in the transanal pull-through for Hirschsprung disease: effect on outcome. J Pediatr Surg. 2007;42:36-39.