CHAPTER 7 Hip Instability
Unlike the shoulder, which relies primarily on static and dynamic soft tissue restraints for its stability, the hip depends primarily on its osseous anatomy. The hip’s unique soft tissue envelope also plays a role in its stability, particularly when there is any significant deviation from normal.1 When considering a patient with hip pain that is believed to be at least in some way the result of hip instability, both osseous and soft tissue constraints must be considered. Traumatic dislocation is typically accompanied by a history of an acute event. Atraumatic hip instability can result from repetitive rotational movements. The hypothesized mechanism for this type of instability is a subclinical capsular laxity accompanied by mild hip dysplasia that may progress over time.2 Generalized laxity and connective tissue disorders are also causes of atraumatic instability.
ANATOMY
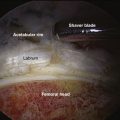
Although relying largely on its bony anatomy, hip stability is complemented by the acetabular labrum and capsuloligamentous complex. In the neutral anatomic position, the anterior part of the femoral head is not engaged in the acetabulum. The acetabular labrum compensates for this by covering this portion of the femoral head. The labrum is attached to the transverse acetabular ligament anteriorly and posteriorly at the base of the fovea and proceeds to run around the circumference of the acetabular rim.1 The labrum deepens the “socket” and aids in maintaining the suction effect that provides additional hip stability. Absence of the labrum can lead to a loss of this suction effect, as well as increased cartilage surface consolidation as a result of the loss of hydration, thereby increasing contact pressures.3–5 Proprioceptors and nociceptors have been identified within the labrum and may explain the decreased proprioception and increased pain in the athlete with a torn labrum.6 Much like the meniscus in the knee, the labrum is largely avascular, except for the most peripheral portion near the capsule, limiting its ability to heal.7
The labrum is not, however, a stand-alone structure. It functions in conjunction with the capsuloligamentous complex. The fibrous hip capsule and its ligaments are like a thick sleeve. Anteriorly, this complex primarily consists of the iliofemoral ligament (ligament of Bigelow), a 12- to 14-mm thick structure shaped like an inverted Y. It provides resistance to hip extension beyond neutral and resists external rotation. The pubofemoral ligament, which arises from the pubic portion of the acetabular rim and passes below the neck of the femur to blend with the most inferior fibers of the iliofemoral ligament, reinforces the inferior and anterior capsules, resisting extension and abduction. The ischiofemoral ligament reinforces the posterior surface of the capsule and has a spiraling pattern. Finally, the zona orbicularis is a deep layer of fibers within the capsule that forms a circular pattern around the femoral neck, constricting the capsule and helping maintain the femoral head within the acetabulum.1
The position of maximum hip joint stability is in full extension because it is in this position that the twisted orientation of the capsular ligaments causes a screw-home effect.1 However, the articular surfaces of the hip joint are not in optimal contact in this position (the close-packed position). Optimal contact occurs in the loose packed position of flexion and lateral rotation as the ligaments uncoil. The greatest risk of traumatic dislocation, then, is when the joint is between the close-packed and maximally congruent position (flexed and adducted position). The ligamentum teres and psoas tendon are two extra-articular structures about the hip that deserve additional discussion. The ligamentum has no real stabilizing effect on the joint, whereas the psoas protects the anterior intermediate capsule, which is devoid of ligamentous protection.
CLINICAL EVALUATION
History
Making the diagnosis of hip instability can be a diagnostic dilemma. Hip instability can manifest as overtly as frank traumatic dislocation or can be as obscure as occult groin pain or clicking. Hip pain, clicking, or “giving way” in the young adult patient may arise from any number of anatomic structures. The picture can be further complicated by referred pain from the lumbosacral region as well as the genitourinary tract and abdominal wall.8 Age also plays a significant role in determining a differential diagnosis for hip pain.9 In children, hip dislocation, bony avulsions, apophyseal injuries, fractures, slipped capital femoral epiphysis (SCFE), Legg-Perthes disease, developmental dysplasia of the hip (DDH), and toxic and septic arthritis are all potential causes.9
Physical Examination
Antalgic gait patterns in which there is shortening of the stance phase and step length on the affected side can result from instability. A Trendelenburg gait may indicate an attempt to bring the center of gravity over the affected side to decrease the moment arm across that hip joint.10 The patient with atraumatic instability may be able to demonstrate subluxation or dislocation of the involved hip, although this is rare.
Traumatic hip instability can manifest with pain on prone extension–external rotation of the involved hip. A positive axial distraction test can be confirmed with a positive vacuum sign on dynamic fluoroscopy (Fig. 7-1).1 Anterior apprehension may also be elicited with the patient in the lateral decubitus position while suspending the affected leg in slight abduction (Fig. 7-2). The presence of a positive examination indicates capsular laxity in traumatic and atraumatic instability.

FIGURE 7-2 Apprehension position. The patient is placed in the lateral decubitus position and the affected extremity is supported by the examiner. The examiner uses the other arm to push the hip in an anterior direction as pressure is applied over the posterior aspect of the greater trochanter. In symptomatic patients, a sensation of subluxation can sometimes be elicited, whereas in others, there is a reproduction of their pain.
In some patients, and with proper relaxation, a sense of the end range of capsular tightness and the end point of the ligamentum teres can be obtained by the supine external rotation test, in which the patient is placed supine and the affected leg is suspended in 30 degrees of flexion by the examiner. With gentle external rotation, while the patient is relaxed, the end point of external rotation can be assessed (Fig. 7-3). Also, a comparison can be made with the contralateral (and presumably normal) extremity. If there is a significant increase in external rotation as compared with the normal extremity, laxity of the Y ligament can be inferred. Also, if a large anterior labral tear exists, audible snapping and reproduction of pain can be elicited.
IMAGING
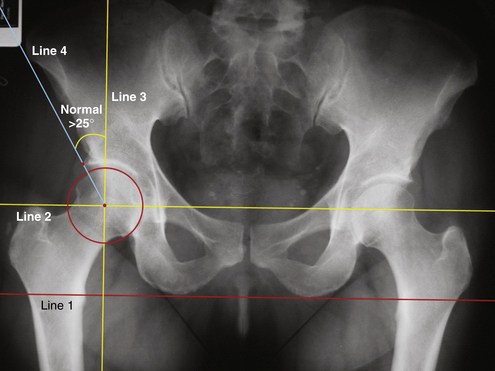
Several radiographic indices have been described to differentiate normal from abnormal osseous anatomy based on the AP pelvic radiograph. The Tonnis angle is used to assess lateral subluxation of the femoral head and subsequent increased forces across the weight-bearing acetabulum (Fig. 7-4).11 A measurement of less than 10 degrees is considered normal.
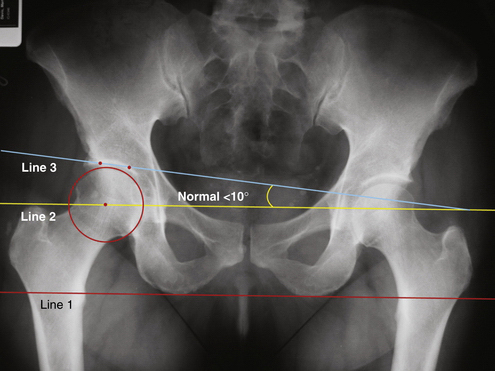
FIGURE 7-4 AP radiograph showing the technique of measuring the Tonnis angle (normal, <10 degrees). In this case, the red line (line 1) connecting the two ischial tuberosities is the reference line on which all other lines are based. The yellow line (line 2) is a line drawn parallel to line 1 through the center of the femoral head. The angle formed between line 2 and a third line connecting two points demarcating the sourcil or weight-bearing surface of the acetabulum is the Tonnis angle.
(Adapted from Delaney S, Dussault RG, Kaplan PA, et al. Radiographic measurements of dysplastic adult hips. Skeletal Radiol. 1997;26:75-81.)
The center edge angle of Wiberg assesses acetabular inclination (Fig. 7-5). This angle should measure at least 20 to 25 degrees to be considered normal.12,13 One can estimate acetabular version using the AP pelvis by looking for a crossover sign (Fig. 7-6). The two lines involved estimate the posterior and anterior rims of the acetabulum. The posterior rim is traced from the ischial tuberosity superolaterally to the roof of the acetabulum. The anterior rim is traced from the teardrop in a superior and lateral direction along the rim to the roof. If these lines cross, it is estimated that the acetabulum is retroverted; if not, it is assumed that the acetabular version is within the normal 10- to 15-degree anterior version.14,15
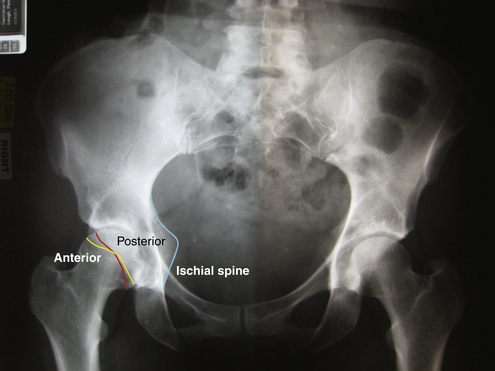
FIGURE 7-6 AP radiograph demonstrating the crossover sign indicating acetabular retroversion. Note that the red line (representing the anterior wall of the acetabulum) crosses the yellow line (representing the posterior wall of the acetabulum). Also of note is the visualization of the ischial tuberosity (blue line), which is normally superimposed by the acetabulum, but easily visible in the retroverted acetabulum.
When evaluating a patient with potential residual dysplasia, the faux profile view is often used to evaluate anterior and lateral coverage of the femoral head by the acetabulum. Although plain radiographs are sufficient for diagnosis in a number of cases, there are pathologic entities that require further investigation. Imaging of bony lesions about the hip is best accomplished using computed tomography (CT) because it provides the greatest spatial resolution of bony structures. Cases of questionable hip dysplasia should use CT in preoperative planning. The use of intra-articular contrast in CT arthrography can increase the contrast between cartilage and labral tissue.8
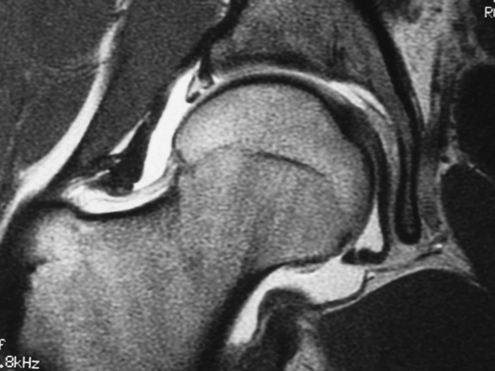
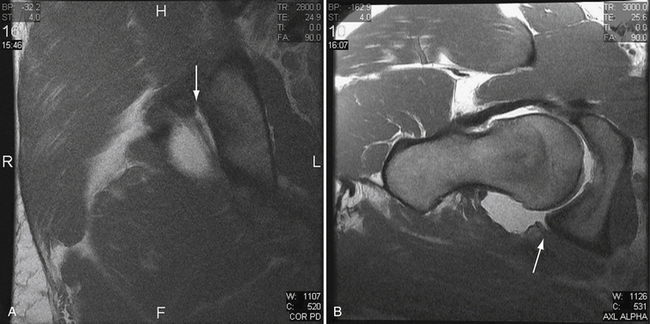
Magnetic resonance imaging (MRI) has become the most reliable means of diagnosing unresolved hip pathology in addition to direct visualization and is often useful in cases of instability. MRI has been shown to demonstrate inflammatory arthropathies and joint effusions effectively, but has been less accurate in assessing articular cartilage lesions.8,16,17 Contrast MRI studies in patients with a torn labrum or torn iliofemoral ligament can result in a larger volume of intra-articular contrast, and thus indirectly confirm the diagnosis of instability (Fig. 7-7).1
TREATMENT CONSIDERATIONS
Atraumatic Instability
Congenital connective tissue disorders can predispose a patient to atraumatic hip instability. There have been very few reports in the literature of habitual hip dislocation that have not been accompanied by Ehlers-Danlos syndrome, arthrochalasis multiplex congenital, Marfan’s syndrome, Down syndrome, or congenital or acquired hip dysplasia.1 As opposed to frank episodes of subluxation or dislocation that may be seen in atraumatic shoulder instability, idiopathic hip instability often presents with a more subtle pattern. In a review of five cases, a syndrome of idiopathic hip instability was described, in which all patients presented with a long history of snapping in the groin, gait disturbances, and pain in the provocative position of hip flexion, adduction, and internal rotation.18 Symptoms were alleviated by extension abduction and external rotation (maneuvers analogous to the Barlow and Ortolani signs), thus suggesting a posterior instability. When awake patients had their affected hip subjected to gentle manual traction, 4 to 10 mm of inferior subluxation was seen. The force used to subluxate the hip in these cases was much less than the 400 N of axial force described as necessary to create a radiographic vacuum sign of subluxation.19 All this evidence led the authors to postulate that subclinical hip dysplasia, combined with capsuloligamentous laxity, causes a break in the suction mechanism of the hip during gait, causing a popping sensation. Presuming that the instability was largely posteriorly directed and that preoperative arthrograms showed posterior capsular redundancy, one patient underwent open posterior capsular plication.
Atraumatic instability has also been attributed to a deficient labrum associated with redundant capsular or ligamentous tissue.1 This deficient complex can create an abnormal load distribution caused by a transiently incongruent joint. The screw-home mechanism caused by the dynamic nature of the hip capsule and its associated ligaments may help explain why pelvic rotation and external rotation of the hip commonly elicit symptoms of instability. Professional and high-level athletes who participate in sports that require repeated hip rotation (e.g., football, golf, gymnastics) are susceptible to overuse injuries to the labrum and capsuloligamentous complex. Tears of the labrum or iliofemoral ligament can result in insufficiency and cause an increased tension on the joint capsule, which can be further exacerbated in patients with slight superior and lateral inclination of the acetabulum. In addition, cadaveric analysis of hip stability following capsular venting and a 15-mm labral tear has shown that positions of hip extension, when combined with abduction or external rotation, result in large strains in the anterior labrum.20
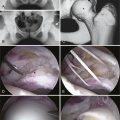
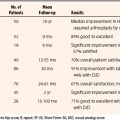
Labral degeneration, combined with subtle rotational hip instability secondary to redundant capsular tissue in elite athletes, has been described. Ten patients were treated with arthroscopic labral débridement and thermal capsulorrhaphy. All patients had improvement in their Harris hip scores, with 83% having significant improvement in their symptoms at 12- to 24-month follow-up.1 In contrast, Santori and Villar have reported only 67.5% success in 58 cases at a mean 3.5-year follow-up with labral débridement without capsular treatment.21 Alternatively, plication can also be performed by passing nonabsorbable, braided suture through the capsule, thus imbricating the capsular tissue (Fig. 7-8).7
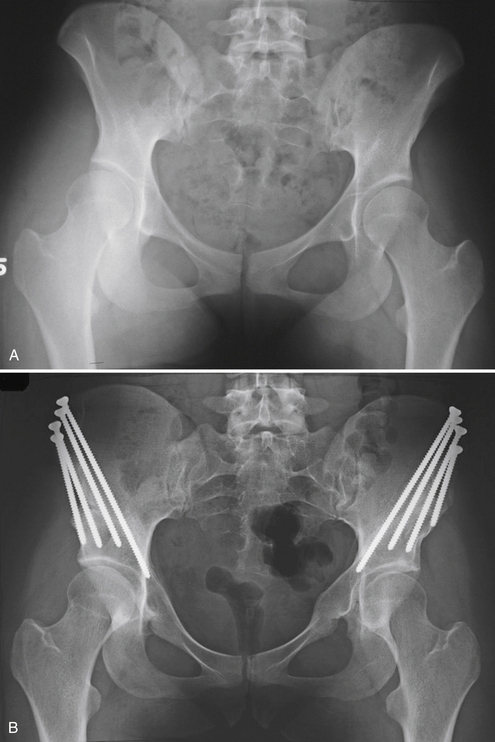
Although subtle hip dysplasia combined with capsular laxity and labral pathology can lead to symptomatic hip instability amenable to arthroscopic treatment, care must be taken to recognize more significant dysplasias. Overtly dysplastic hips typically share common abnormalities that occur to a greater or lesser extent, depending on the severity.22 The true acetabulum is usually shallow, lateralized, anteverted, and deficient anteriorly and superiorly. There may also be underdevelopment of the entire pelvis. On the femoral side, the femoral head is usually small and the neck is usually excessively anteverted and short, with an increased neck-shaft angle. The greater trochanter may be displaced posteriorly and the femoral canal may be narrow.23,24 The presence of significant hip dysplasia in the adult can be ascertained using primarily plain radiography.
A patient who presents with radiographic evidence of dysplasia but little or no symptomatology should be treated nonsurgically with strengthening and proprioceptive training of the hip and trunk musculature.23 Nonsteroidal anti-inflammatory drugs (NSAIDs) can be used and combined with cessation of high-impact activities. The patient should be educated about the potential natural history of increasing instability and the potential development of degenerative arthritis.
Surgical intervention should be reserved for those patients who fail conservative management and have persistent symptoms. Arthroscopic treatment in the patient with significant dysplasia is not indicated. In addition, significant labral hypertrophy occurs in these patients. The role of this excess labral tissue has not been completely elucidated, but it may be significant in its effect on joint stability. Aggressive resection of this tissue can accelerate degenerative changes and possibly lead to premature degeneration. Pelvic and femoral osteotomies, arthrodesis, resection arthroplasty, and replacement arthroplasties have all been described as potential treatment options.23 Osteotomies that may be expected to slow the progression of degenerative changes by distributing weight-bearing forces across the hip joint better have been described. These procedures may also provide better preservation of bone stock for potential subsequent arthroplasty (Fig. 7-9).
Traumatic Instability
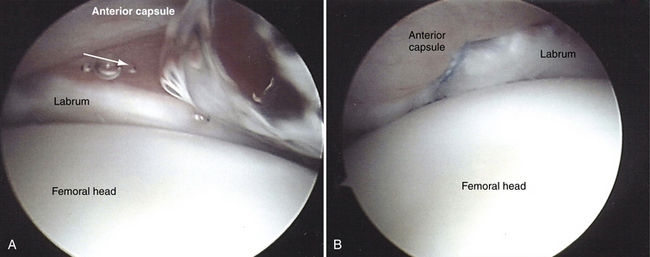
The most common mechanism for hip dislocation is a dashboard motor vehicle injury with a posteriorly directed force against a flexed knee and hip. During athletic activities, dislocations may occur via a forward fall onto a flexed knee with the hip flexed or a blow from behind while down on all four limbs (Fig. 7-10).25,26 Sports such as American football, skiing, jogging, gymnastics, basketball, biking, and soccer have all had reports of traumatic dislocations (Fig. 7-11).27–29 Excessive capsular laxity has been associated with these types of dislocations.30,31 Irrespective of the degree of initial trauma, if normal capsular healing fails to occur, persistent laxity may remain and predispose the patient to instability (Fig. 7-12). Two cases of posterior dislocation following minor trauma while playing soccer have been reported, probably secondary to large posterior capsular redundancy.32 Similarly, recurrent anterior dislocations have occurred as a result of excessive anterior capsular redundancy.33 These patients have been treated nonoperatively with brief immobilization, physical therapy, and activity modification. Open capsular shift or repair has been particularly successful in preventing further dislocation.34 Arthroscopic treatment of this type of capsular laxity using thermal capsulorrhaphy or capsular plication combined with labral débridement has shown promising early results while potentially avoiding the open surgical complications of heterotopic ossification and osteonecrosis of the femoral head.1
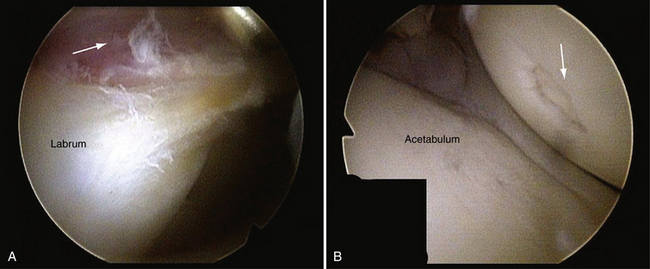
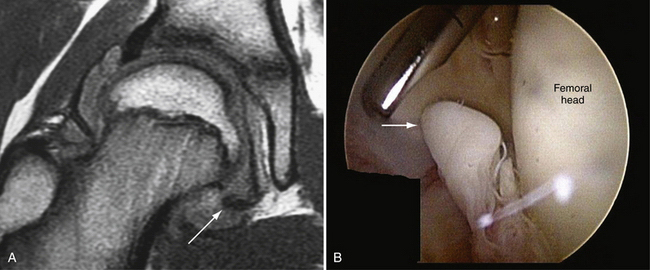
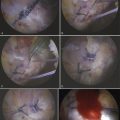
FIGURE 7-11 Labral tear following dislocation of the right hip in a 19-year-old college basketball player (viewed from the anterolateral portal). A, Note the significant synovial reaction (arrow) around the labral tearing. B, Focal femoral head defect (arrow) in the same patient.
Hip arthroscopy has been shown to be an important part of the armamentarium in the effort to at least delay the onset of post-traumatic degenerative joint disease (DJD) following traumatic dislocation.35,36 Residual intra-articular bony or osteochondral fragments may be responsible for the development of DJD in complex dislocations. The incidence of osteoarthritis secondary to traumatic hip dislocation has been reported between 24% to 57%, depending on the severity of the trauma.37 Simple dislocations (without radiographic evidence of fracture) have been shown to have the lowest incidence. However, the incidence of post-traumatic DJD in these injuries is still 24%.38
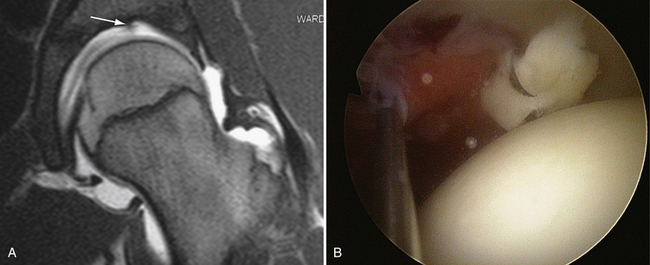
Nonconcentric reduction after a traumatic dislocation is considered an absolute indication for operative intervention. The presence of loose bodies (LBs), however, has been considered a relative indication, particularly if the reduction is concentric and the LBs are located below the fovea.35 An in vivo rabbit model has shown that free cartilaginous loose particles inside the joint increase chondrolytic enzyme activity and induce secondary arthrosis.39 Because 24% of simple dislocations have been shown to develop subsequent DJD, the literature would support that LBs should be addressed prophylactically, and arthroscopy is an excellent vehicle for accomplishing this (Fig. 7-13).38
Mullis and Dahners36 have reported on a series of 36 patients treated with arthroscopy following dislocation. Excluding procedures in which a repeat arthroscopy was performed for retained LBs, the average time to surgery was 15 days. Of 36 patients, 25 (69%) had radiographic evidence of LBs (nonconcentric reduction and/or radiographically visible LBs). In 9 patients, there was a concentric reduction without radiographic LBs. Intraoperatively, 33 of 36 patients(92%) were found to have LBs. Of the 9 patients with no preoperative radiographic evidence of LBs, 7 (78%) had some found at arthroscopy (Fig. 7-14).
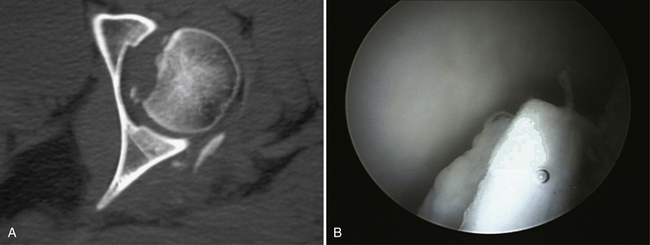
FIGURE 7-14 Loose bodies in the hip with nonconcentric reduction. A, CT scan through the center of the femoral head depicting multiple loose bodies within the joint. B, Intraoperative image of loose osteocartilaginous fragment that was removed.
In a 15-year experience with hip arthroscopy after traumatic dislocation, 10 joints in nine patients were treated 1 to 7 days postdislocation.35 Seven hips were classified as Thompson-Epstein (TE) I injuries, two type II, one type IV, and one central fracture dislocation. All dislocations had arthroscopic lavage and débridement and 7 of 10 joints revealed previously unrecognized loose osteochondral fragments. At a minimum of 5 years follow-up, 8 of 10 joints were asymptomatic. One joint (Pipken type 3 femoral head fracture) went on to develop femoral head AVN that was not symptomatic. The one TE IV injury developed hip joint DJD at 1 year. These results prompted the authors to recommend arthroscopic débridement for all TE types I and II dislocations, but not types III and IV.
Philippon and colleagues26 have recently documented acute dislocations in 14 professional athletes. The findings of importance in their study were a significant association between dislocations and additional findings, including significant labral tears (100%), as well as multiple LBs and osteochondral injuries on the acetabular and femoral surfaces in 73% of cases. In addition, 73% had tears of the ligamentum teres. Finally, there were 9 patients (60%) who had evidence of femoroacetabular impingement by radiographic and arthroscopic evaluation.
There has been some concern regarding the timing of arthroscopy after traumatic dislocation in terms of the risk of avascular necrosis (AVN), prompting those concerned to recommend a 6-week waiting period postdislocation before performing arthroscopy. In two of the previously discussed series, however, arthroscopic surgery was performed in the first 2 weeks.35,36 The only complications observed in the Mullis and Dahners study were three repeat procedures for retained LBs and some fluid extravasation into the gluteal compartment that resolved without incident. Although the possibility of extravasation and subsequent significant complication exists, it can be mitigated by keeping the pressure on the arthroscopic pump low (if one is used). Also, expeditious management of the pathology with limited exposure to inflow of fluid will avoid this issue. In cases in which extended surgical procedures are undertaken, it is important to palpate the abdomen and maintain a watchful eye on the patient’s vital signs to note any ongoing extravasation, particularly into the abdominal cavity.36 Yamamoto and associates35 had one case of AVN that developed in a patient with a Pipken type 3 injury.
SURGICAL TECHNIQUE
The first technique to discuss with regard to the challenges presented by dislocations is that of labral repair. A variety of techniques are available for repair of labral detachment; these are similar to the experience in the shoulder. The specific challenges presented by the hip include the limited maneuverability within the joint and sometimes the degree of damage to the labrum, precluding a good repair. The specific techniques have been described in the chapter on labral injury (see Chapter 3).
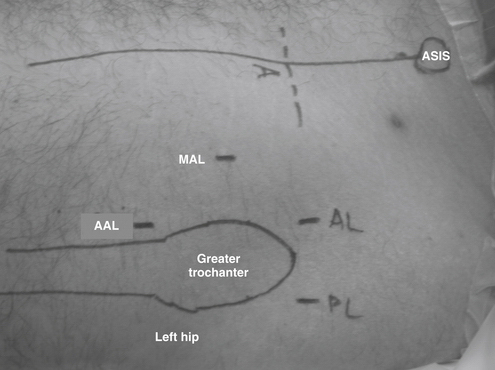
Once all the labral pathology has been addressed, the amount of capsular redundancy is assessed. It is important to assess the laxity over the area that is presumed to be abnormal based on the EUA and the mechanism of injury, if one is known. Most commonly, the anterior capsule is involved in atraumatic patients. The assessment and treatment of this problem are undertaken from the peripheral compartment with traction removed and the leg in approximately 45 degrees of flexion. To imbricate the capsule, an accessory portal needs to be established, in addition to the standard anterior and anterolateral portals. The portal that is typically established is termed the midanterolateral (MAL) portal and is established midway between the anterior and anterolateral portals, creating an equilateral triangle between the three portals (Fig. 7-15). This portal is used for manipulation of the sutures between portals.
In the typical case, the imbrication is undertaken in a medial to lateral direction. In patients in whom there is a very large perilabral sulcus, a proximal to distal imbrication is technically simpler easier to accomplish (see Fig. 7-8). When a medial to lateral imbrication is undertaken, the first step is to isolate the capsule on both the intra-articular and extra-articular spaces. The extra-articular preparation is undertaken by pulling the arthroscope out of the capsule (arthroscope in the anterolateral [AL] portal). Once the scope is out of the joint, the anterior portal is used to elevate the soft tissues away from the capsule to visualize the area where the imbrication will take place. Once an area of approximately 2 cm2 is cleared, preparation is made for suture passing. The anterior portal serves as the portal for delivery of sutures from outside the joint and the MAL serves as the portal to grasp the sutures within the joint. Using a suture penetrator device, one suture is placed through the capsule and grasped from the AL portal. The other limb of the suture is now passed through the capsule, approximately 1 cm more lateral than the first limb. This limb is retrieved through the AL portal and shuttled outside the cannula. A second suture is now passed proximally or distally to the first, depending on the configuration of the first suture. Once the two sutures are passed, the arthroscope is placed outside the joint again and the sutures are tied (see Fig. 7-8). Confirmation of appropriate tightening of the joint can be obtained by visualization of the joint through the AL portal.
PEARLS& PITFALLS
CONCLUSION
The spectrum of hip instability is wide and includes symptomatology that ranges from what is similar to that of a simple snapping hip to a complete dislocation that results in persistent repeated dislocations or subluxations. A thorough history and physical examination, combined with the appropriate imaging studies, are essential for determining where the patient’s complaints fit on this spectrum.
1. Philippon MJ. The role of arthroscopic thermal capsulorrhaphy in the hip. Clin Sports Med. 2001;20:817-829.
2. Takechi H, Nagashima H, Ito S. Intra-articular pressure of the hip joint outside and inside the limbus. J Jpn Orthop Assoc. 1982;56:529-536.
3. Ferguson SJ, Bryant JT, Ganz R, et al. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171-178.
4. Ferguson SJ, Bryant JT, Ganz R, et al. The acetabular labrum seal: a pro-elastic finite element model. Clin Biomech. 2000;15:463-468.
5. Ferguson SJ, Bryant JT, Ganz R, et al. The influence of the acetabular labrum on hip joint cartilage consolidation: a pro-elastic finite element model. J Biomech. 2000;33:953-960.
6. Kim YT, Azuma H. The nerve endings of the acetabular labrum. Clin Orthop. 1995;320:176-181.
7. Kelly BT, Williams RJ, Philippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med. 2003;316:1020-1037.
8. Kallas KM, Guanche CA. Physical examination and imaging of hip injuries. Oper Tech Sports Med. 2002;10:176-183.
9. Scopp JM, Moorman CTIII. The assessment of athletic hip injury. Clin Sports Med. 2001;20:647-659.
10. Hoppenfeld S. Physical examination of the hip and pelvis. In: Hoppenfeld S, editor. Physical Examation of the Spine and Extremities. Norwalk, Conn: Appleton and Lange; 1976:143-152.
11. Tonnis D, Heinecke A. Acetabular and femoral anteversion. relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:747-1770.
12. Delaunay S, Dussault RG, Kaplan PA, et al. Radiographic measurements of dysplastic adult hips. Skeletal Radiol. 1997;26:75-81.
13. Wenger DR, Bomar JD. Human hip dysplasia: evolution of current treatment concepts. J Orthop Sci. 2003;8:264-271.
14. Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:747-1770.
15. Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281-288.
16. Edwards DJ, Lomas D, Villar RN. Diagnosis of the painful hip by magnetic resonance imaging and arthroscopy. J Bone Joint Surg Br. 1995;77:374-376.
17. Hodler J, Trudell D, Pathria MN, et al. Width of the articular cartilage of the hip: quantification using fat suppression spin echo MRI in cadavers. AJR Am J Roentgenol. 1992;192:351-355.
18. Bellabarba C, Sheinkop M, Kuo K. Idiopathic hip instability. Clin Orthop. 1998;355:261-271.
19. Arvidsson I. The hip joint: Forces needed for distraction and appearance of the vacuum phenomenon. Scand J Rehabil Med. 1990;22:157-161.
20. Crawford MJ, Dy CJ, Alexander JW, et al. The biomechanics of the hip labrum and the stability of the hip. J Orthop Res. 2007;465:16-22.
21. Santori N, Villar R. Acetabular labral tears: result of arthroscopic partial limbectomy. Arthroscopy. 2000;16:11-15.
22. Massie WK, Howorth MB. Congenital dislocation of the hip. Part 1. Methods of grading results. J Bone Joint Surg Am. 1950;32:519-531.
23. Tonnis D, Legal H, Graf R, editors. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin: Springer-Verlag, 1987.
24. Lequesne M, De Seze M. False profile of the pelvis: A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies. Rev Rheum Mal Osteoartic. 1961;28:643-652.
25. Sanchez-Sotelo J, Berry DJ, Trousdale RT, et al. Surgical treatment of developmental dysplasia of the hip in adults: II. Arthroplasty options. J Am Acad Orthop Surg. 2002;210:334-344.
26. Philippon MJ, Kuppersmith DA, Wolff AB, et al. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthroscopy. 2009;25:169-174.
27. Chudik S, Lopez V. Hip dislocations in athletes. Sports Med Arthrosc Rev. 2002;10:123-133.
28. Lamke LO. Traumatic dislocations of the hip. Follow-up on cases from the Stockholm area. Acta Orthop Scand. 1970;41:188-198.
29. Mitchell JC, Giannoudis PV, Millner PA, et al. A rare fracture-dislocation of the hip in a gymnast and review of the literature. Br J Sports Med. 1999;33:283-284.
30. Lieberman J, Altchek D, Salvati E. Recurrent dislocation of a hip with a labral lesion. Treatment with a modified bankart repair. J Bone Joint Surg Am. 1993;75:1524-1527.
31. Sullivan CR, Bickel WH, Lipscomb PR. Recurrent dislocation of the hip. J Bone Joint Surg Am. 1955;37:1256-1270.
32. Townsend R, Edwards G, Bazant F. Posttraumatic recurrent dislocation of the hip without fracture. J Bone Joint Surg Br. 1969;51B:38-44.
33. Liebenberg F, Dommisse G. Recurrent posttraumatic dislocation of the hip. J Bone Joint Surg Am. 1969;51:632-637.
34. Dall D, MacNab I, Gross A. Recurrent anterior dislocation of the hip. J Bone Joint Surg Am. 1970;52:574-576.
35. Yamamoto Y, Takatoshi I, Ono T, Hamada Y. Usefulness of arthroscopic surgery in hip trauma cases. Arthroscopy. 2003;19:269-273.
36. Mullis BH, Dahners LE. Hip arthroscopy to remove loose bodies after traumatic dislocation. J Orthop Trauma. 2006;20:22-26.
37. Armstrong JR. traumatic dislocation of the hip: review of 101 dislocations. J Bone Joint Surg Br. 1948;30:430-445.
38. Brav CEA. Traumatic dislocation of the hip. J Bone Joint Surg Am. 1962;44:1115-1134.
39. Epstein HC. Traumatic dislocations of the hip. Clin Orthop. 1973;92:116-142.