Chapter 57 Hip Dislocation: How Does Delay to Reduction Affect Avascular Necrosis Rate?
A dislocated hip represents a true orthopaedic emergency and requires immediate attention. Reduction of any dislocated joint helps to reduce pain, improves circulation within the surrounding soft tissues, removes pressure on the chondral surfaces, and allows for better radiographic imaging. In the case of the hip joint, an associated risk for avascular necrosis of the femoral head is present. Time to reduction of the dislocated hip has been implicated as a factor in the development of avascular necrosis.
OPTIONS
Avascular necrosis is a devastating complication that results in death of the osteocytes in the femoral head, subsequent chondral collapse, and secondary degenerative osteoarthritis of the hip joint. Death of these osteocytes is thought to occur because of ischemia from damage to the blood supply to the femoral head.1 Blood is supplied to the femoral head through both extraosseous and intraosseous vessels. Extraosseous vessels include the medial femoral circumflex, the ligamentum teres, and the retinacular vessels.2,3 Several basic science studies have shown that traumatic dislocation of the hip places tension on the medial femoral circumflex artery and more proximally at the junction of the common femoral artery with the external iliac artery.4–6 This leads to disruption of both the intraosseous and extraosseous vasculature. Does this disruption improve with early reduction of the hip?
A subset of hip dislocations (3–13% in the literature) are irreducible closed and require open reduction.7–11 These irreducible hip dislocations are frequently associated with fracture of the femoral head or acetabulum with incarceration of a bony fragment in the hip joint. Alternatively, the head may have “buttonholed” through the hip capsule, the piriformis muscle may block relocation of the head, or the labrum may have torn and flipped into the joint.12 Given this scenario, when should surgical relocation of the hip be preformed? Most general orthopedic surgeons can perform an open reduction of a hip dislocation; however, those associated with femoral head or acetabular fracture often necessitate referral to a trauma specialist for definitive fixation. Should the referring surgeon perform an open reduction and relocate the hip before transferring to the specialist for a second procedure to fix the fracture? Should relocation of the hip be deferred and managed definitively by the trauma specialist?
EVIDENCE
Animal studies suggest that the disruption of the vascular supply to the femoral head may improve with reduction within 12 hours. Duncan and Shim4 found that early reduction of the dislocated hip improved early and complete recovery of blood supply to the femoral head in a rabbit model. Reduction of the dislocated hip delayed beyond 12 hours did not benefit the rate and extent of the circulatory recovery of the femoral head. Histologic avascular necrosis was observed in hips reduced early and late; however, it was less frequently observed and less severe in those reduced early. In a subsequent study using rabbits and canines, Shim5 found that vascular damage was largely due to compression, traction, and spasm of the extraosseous vessels (only a minority of these was ruptured). This is reinforced by a human cadaveric study demonstrating that dislocation caused compression of the medial femoral circumflex and common femoral vessels.6 These basic science studies suggest that the vascular disruption is reversible with reduction of the hip. Furthermore, early reduction may reverse ischemic changes that occur in the femoral head at a cellular level.
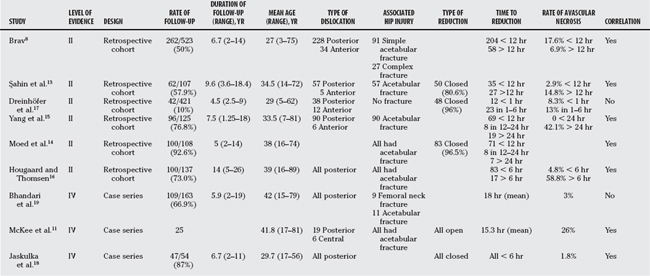
Clinical studies that explore the effect of timing of hip reduction on the rates of avascular necrosis are largely retrospective cohort studies. No study was identified that focused solely on the rate of avascular necrosis as a function of time to reduction. Rather, these studies explored several different outcome measures (e.g., avascular necrosis, patient satisfaction, degenerative osteoarthritis) and several different variables (e.g., type of dislocation, time to weight bearing). We have identified six Level II and three Level IV studies with regard to effect of reduction on rate of avascular necrosis (Table 57-1).
Brav8 reviewed traumatic hip dislocations that presented to U.S. Army hospitals during a 12-year period from 1947 to 1958.8 He found that the rate of avascular necrosis was 17.6% when reduction occurred before 12 hours and 56.9% when reduction was delayed over 12 hours. Although no statistical analysis was done to prove significance (no P value was reported), there is a definite trend to reduced avascular necrosis in the group treated early.
Subsequent Level II studies have presented similar results with respect to timing of reduction and rates of avascular necrosis. Şahin and colleagues13 examined 62 cases of traumatic hip dislocation (5 anterior and 57 posterior with associated acetabular fracture) and found a trend for decreased avascular necrosis when the hip was reduced within 12 hours (2.9%) as compared with after 12 hours (14.8%). In addition, they found that there was no significant difference between hips reduced less than 6 hours and those reduced between 6 to 12 hours after injury. Moed and coworkers14 also note a significant reduction in rates of avascular necrosis in hips reduced within 12 hours (P < 0.001) but did not comment on the absolute rates. Yang and coauthors15 present a retrospective cohort of 96 hip dislocations that included both anterior and posterior dislocations with and without acetabular fractures. They found no avascular necrosis in dislocations reduced within 24 hours and a rate of 42.2% in those reduced after 24 hours. Hougaard and Thomsen16 presented 100 posterior hip dislocations with and without associated fracture of the acetabulum. They found a decrease in avascular necrosis when the hip was reduced within 6 hours (4.8% at <6 hours, and 58.8% at ≥6 hours). They had insufficient data to comment on a difference between reduction less than 6 hours and reduction between 6 and 12 hours. This study also found an increase in avascular necrosis with severity of injury (5% with minor acetabular fracture and 52.6% with severe acetabular fracture and/or femoral head or neck fracture).
Dreinhöfer and investigators’17 study was the only Level II study that suggested there was no difference in avascular necrosis with delayed reduction.17 However, all 35 hip dislocations (anterior and posterior dislocations without associated fracture) in their series were reduced within 6 hours of injury. They focused on a difference in avascular necrosis in a group treated within 1 hour (8.3%) versus a group treated in 1 to 6 hours (13%) and found no significant difference.
Three Level IV evidence articles were identified. These articles are case series because they present rates of avascular necrosis for dislocations reduced at a specific time. Two of these articles, by Jaskulka and colleagues18 and McKee and coworkers,11 conclude that there was an increase in avascular necrosis with time to reduction.11,18 Jaskulka and colleagues18 report a rate of 1.8% (i.e., 1 case) in their series of 47 posterior fracture dislocations and attributed this low rate to the fact that all hips were reduced within 6 hours.18 McKee and coworkers11 presented a series of 25 central and posterior dislocations with associated severe acetabular and femoral neck fractures. They attribute their high avascular necrosis rate (26%), in part, to the relatively long time to reduction (mean, 15.3 hours). However, patients in this series all sustained severe trauma, and this may be a more significant factor in the high rate of avascular necrosis. Bhandari and coauthors19 report on 109 posterior hip dislocations with associated acetabular fracture and conclude that time to reduction was not a prognostic factor. Their reported rate of avascular necrosis was 3%, and their average time from injury to reduction was 18 hours. They did not use avascular necrosis as an outcome but rather used radiologic grade, clinical grade, or the development of arthritis as outcomes. Their multivariate analysis suggests that the quality of fracture reduction has the greatest impact on these outcomes, and that time to reduction has less of an impact. However, these outcome measures do not specifically address development of avascular necrosis and likely are better indicators of the development of secondary osteoarthritis in the hip.
AREAS OF UNCERTAINTY
Position of Hip Dislocation
Anterior dislocations of the hip are rare and account for 6.3% to 13% of reported hip dislocations.13,15, 18 These injuries are typically grouped together with posterior dislocations in studies. However, of the two studies that analyzed anterior dislocations as a separate group, no avascular necrosis was reported in one study, and a rate of 4.8% was reported in the other study.8,17 This lower rate of avascular necrosis may be because of the position of the dislocated proximal femur and the resulting trauma to its vasculature.
Yue and researchers6 showed in their cadaveric study that a posteriorly dislocated hip with the leg in external rotation (i.e., the hip was first posteriorly dislocated and then the leg was forced into external rotation) created filling defects in both the common femoral and medial femoral circumflex arteries. The filling defects in the common femoral artery were reversed when the leg was rotated internally (the hip remained posteriorly dislocated); however, the filling defects in the medial femoral circumflex arteries remained. Presumably, the filling defects in the medial femoral circumflex arteries are due to pressure exerted on the posterior hip capsule and overlying vasculature because of the posteriorly displaced head of the femur. Defects in the common femoral artery result from twisting of the artery because of the position of the leg (i.e., worse when the leg is externally rotated). Although not specifically tested, one may assume that an anteriorly dislocated hip would result in a reversible defect in the common femoral artery (because the leg is externally rotated) and no defect in the femoral circumflex arteries (because the femoral head is displaced anteriorly and the posterior hip capsule is not under tension).
Associated Acetabular and Proximal Femur Fractures
Brav8 reports lower rates of avascular necrosis in anterior and posterior dislocation groups without associated acetabular fracture (13.9% < 12 hours and 47.8% > 12 hours), and quite high rates of avascular necrosis in those with severe associated acetabular and femoral head fractures (62.5% < 12 hours and 81.8% > 12 hours). Greater rates of avascular necrosis were observed in series that included acetabular and femoral head/neck fractures as compared with those that did not (see Table 57-1). This may be explained by the more significant trauma to the soft tissue and vasculature that is sustained with these injuries. These injuries also often require surgical management, and this may further damage the vasculature.
Letournel and Judet20 suggest that time to reduction had little prognostic value. Their series of acetabular fracture dislocations demonstrates low rates of avascular necrosis despite a long interval of time between injury and reduction (5% < 6 hours, 8% between 6 and 24 hours, and 4% > 24 hours). Bhandari and coauthors’19 results agree with this as they have reported a low rate of avascular necrosis (3%) with posterior dislocation and associated acetabular fracture. Their explanation is that the posterior acetabular fracture allows the femoral head to sit in a position that places less tension on the medial femoral circumflex and retinacular vessels than if the acetabulum was intact. If this is correct, the greater rates of avascular necrosis observed in other series (see Table 57-1) may be caused by associated surgical trauma or inclusion of femoral head/neck fractures in these series. However, we cannot discount the Level II studies that suggest greater rates of avascular necrosis in patients with associated acetabular fracture that experience delay in reduction beyond 12 hours.
Hip dislocations are relatively rare and result from significant trauma. These injuries frequently occur in the patient with multiple injuries who is often medically unstable. Definitive management of these injuries often requires transfer to a specialist. In both of these scenarios, knowledge of optimal time for reduction is required. Based on our review of the literature, we have made the following recommendations (Table 57-2):
TABLE 57-2 Grades of Recommendations for the Treatment of Hip Dislocation
| RECOMMENDATIONS | LEVEL OF EVIDENCE/GRADE OF RECOMMENATION |
|---|---|
1 Rodriguez-Merchan EC. Osteonecrosis of the femoral head after traumatic hip dislocation in the adult. Clin Orthop. 2000;377:68-77.
2 Sevitt S, Thompson RG. The distribution and anastomoses of arteries supplying the head and neck of the femur. J Bone Joint Surg Br. 1965;47-B:560-573.
3 Gautier E, Ganz K, Krügel N, et al. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82-B:679-683.
4 Duncan C, Shim S. Blood supply of the head of the femur in traumatic hip dislocation. Surg Gynecol Obstet. 1977;144:185-191.
5 Shim SS. Circulatory and vascular changes in the hip following traumatic hip dislocation. Clin Orthop. 1979;140:255-261.
6 Yue JJ, Wilber JH, Lipuma JP, et al. Posterior hip dislocations. A cadaveric angiographic study. J Orthop Trauma. 1996;10:447-454.
7 Thompson VP, Epstein HC. Traumatic dislocations of the hip. A survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg Am. 1951;33-A:746-778.
8 Brav EA. Traumatic dislocations of the hip. Army experience and results over a twelve-year period. J Bone Joint Surg Am. 1962;44-A:1115-1134.
9 Hunter GA. Posterior dislocation and fracture-dislocation of the hip. A review of fifty-seven patients. J Bone Joint Surg Br. 1969;51-B:38-44.
10 Proctor H. Dislocations of the hip joint (excluding “central” dislocations) and their complications. Injury. 1973;5:1-12.
11 McKee MD, Garay ME, Schemitsch EH, et al. Irreducible fracture-dislocation of the hip: A severe injury with a poor prognosis. J Orthop Trauma. 1998;12:223-229.
12 Canale ST, Manugian AH. Irreducible traumatic dislocations of the hip. J Bone Joint Surg Am. 1979;61-A:7-14.
13 Şahin V, Karakas ES, Aku S, et al. Traumatic dislocation and fracture-dislocation of the hip: A long-term follow-up study. J Trauma. 2003;54:520-529.
14 Moed BR, Willson Carr SE, Watson JT. Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am. 2002;84-A:752-758.
15 Yang RS, Tsuang YH, Hang YS, et al. Traumatic dislocation of the hip. Clin Orthop. 1991;265:218-227.
16 Hougaard K, Thomsen PB. Coxarthrosis following traumatic posterior dislocation of the hip. J Bone Joint Surg Am. 1987;69-A:679-683.
17 Dreinhöfer KE, Schwarzkopf SR, Haas NP, et al. Isolated traumatic dislocation of the hip: Long-term results in 50 patients. J Bone Joint Surg Br. 1994;76-B:6-12.
18 Jaskulka RA, Fischer G, Fenzl G. Dislocation and fracture-dislocation of the hip. J Bone Joint Surg Br. 1991;73-B:465-469.
19 Bhandari M, Matta J, Ferguson T, et al. Predictors of clinical and radiological outcome in patients with fractures of the acetabulum and concomitant posterior dislocation of the hip. J Bone Joint Surg Br. 2006;88-B:1618-1624.
20 Letournel E, Judet R. Elson RA, editor. Fractures of the Acetabulum. New York: Springer-Verlag, 1993.