High Frequency Ventilation
A High frequency ventilation (HFV) is a form of mechanical ventilation that uses small tidal volumes (Vts approaching deadspace volume or less) and high respiratory rates (>120 breaths/min).
B Basically four different types of high frequency approaches to ventilation have been used.
1. High frequency positive-pressure ventilation (HFPPV): This approach uses conventional ventilators to provide HFV.
a. Respiratory rate ranges from 120 to 240 breaths/min.
c. Inspiratory-to-expiratory (I:E) ratios are set at approximately 1:2.
d. Positive end-expiratory pressure (PEEP) can be set at any level.
e. Technically HFPPV is applied via conventional ventilators or pneumatic valve systems.
2. High frequency jet ventilation (HFJV): This approach normally combines the use of a jet ventilator and a conventional ventilator.
a. Respiratory frequency ranges from 120 to 1200 breaths/min or 2 Hz to 20 Hz. One hertz (Hz) equals 60 breaths/min.
b. Vt is estimated to be approximately 2 to 5 ml/kg.
c. The I:E ratio is set at approximately 1:2.
d. PEEP can be set at any level.
e. All systems use a ventilator specifically designed for HFJV and a secondary gas source, commonly a conventional ventilator.
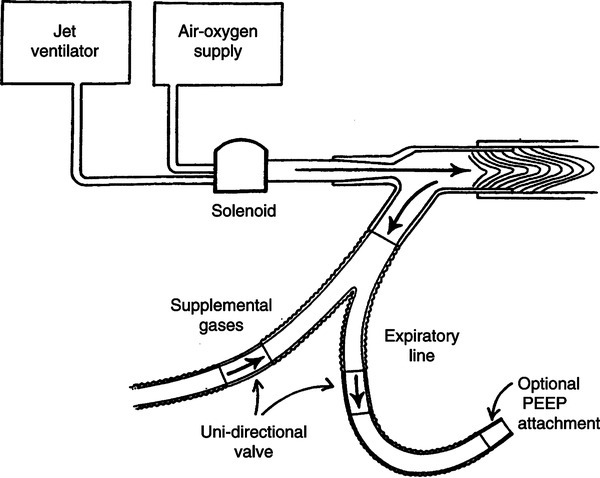
f. Each ventilation system uses a 14- to 18-gauge small-bore injector in which gas is periodically introduced at high pressure (15 to 50 pounds per square inch) into a specially designed endotracheal tube adapter (Figure 42-1). However, the small-bore injector can also be inserted directly into the cricothyroid membrane.
g. Gas is also entrained from a secondary source, mixing with the injector flow to establish Vt (see Figure 42-1).
h. Exhaled gas leaves via a separate route (see Figure 42-1).
i. Gas flow through the injector is interrupted at clinician-set intervals by pneumatic, fluidic, or electronically controlled solenoid valves.
j. With all systems exhalation is passive.
k. The jet flow is humidified by water dripped in front of the injector. The entrained gas is normally humidified.
3. High frequency oscillation (HFO)
a. The most common approach to HFV used today is HFO.
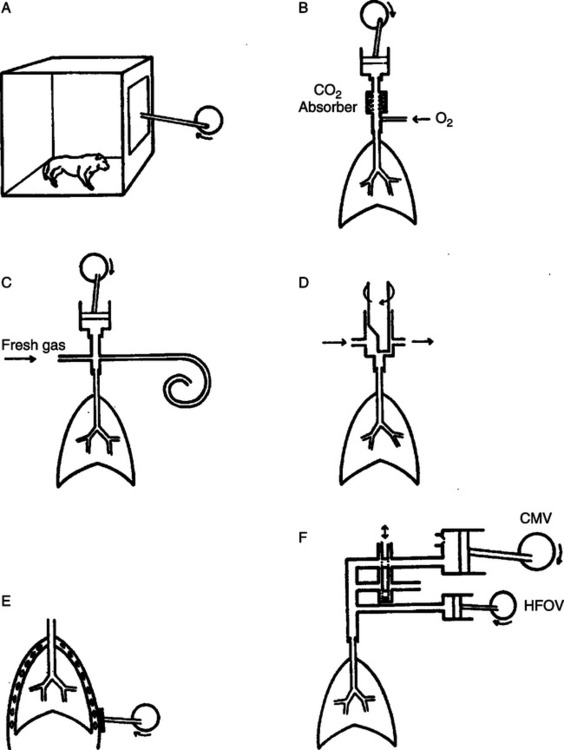
b. Requires a unique self-contained system to provide ventilation
c. Basically a bias flow of gas passes across the airway, exiting through a variable resistor.
d. A mechanism to oscillate the flow is included perpendicular to the bias flow (Figure 42-2).
e. The oscillation causes the inspiratory phase to be positive pressure and the expiratory phase to be negative pressure.
f. The force of the oscillation is referred to as the delta pressure: The total pressure change from inspiration to expiration. If the delta pressure is 60 cm H2O, +30 cm H2O is developed during inspiration and −30 cm H2O is developed during expiration. This is above and below the mean airway pressure.
g. The resistance to the bias flow and the total bias flow controls the mean airway pressure.
h. With some systems the I:E ratio can be adjusted from 1:1 to 1:2.
i. Frequency can vary with most HFO systems from 3 Hz to 20 Hz.
j. As with other ventilatory systems, FIO2 can be adjusted from 0.21 to 1.0.
k. PEEP is not set during HFO. However, during HFO especially at high frequency settings, the mean airway pressure is essentially equal to the PEEP level because the delta pressure is markedly decreased by the time it reaches the alveolar level.
l. High frequency flow interruption is a form of HFO that does not have a negative expiratory phase. The bias flow is simply interrupted to allow passive exhalation to occur.
4. High frequency percussive ventilation (HFPV)
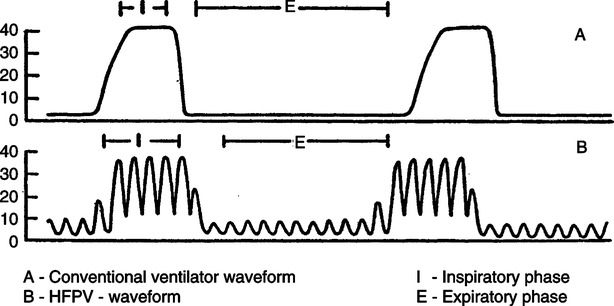
a. This approach to HFV is truly a combination of conventional ventilation and HFV.
b. As noted in Figure 42-3 gas is delivered as a pressure-limited conventional breath with oscillations superimposed on the breath.
c. Oscillations can be delivered either during inspiration only or during inspiration and expiration. Throughout the ventilatory cycle patients may breathe spontaneously in association with the conventional and high frequency breaths.
d. Thus the conventional gas delivery and high frequency approaches to ventilation can be adjusted.
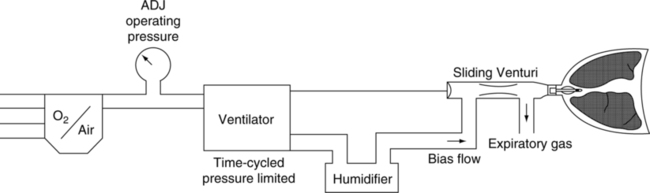
e. HFPV operates by using a high frequency injector that injects gas flow to operate a sliding Venturi valve used to entrain a secondary humidified flow of gas (Figure 42-4).
A During normal spontaneous breathing and conventional mechanical ventilation (CMV) the two factors responsible for gas exchange are
B Convection is primarily responsible for gas movement to the level of the terminal bronchioles and diffusion from the terminal bronchioles to the alveoli.
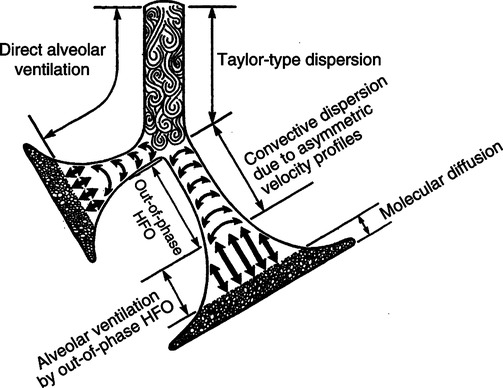
C During HFV many other factors come into play ensuring that CO2 elimination can be maintained despite Vt being equal to or smaller than deadspace volume (Figure 42-5).
D The following have been proposed as possible mechanisms for gas movement during HFV.
1. Pendelluft gas movement: Because neighboring gas units have varying compliance and resistance, filling of lung units is uneven (underventilation of some and overventilation of others); thus gas movement can occur from one lung unit to another that is convective movement within the lung.
2. Convective dispersion by asymmetric velocity profiles: Gas in the center of a column moves faster than gas at the periphery. As a result gas can move to a greater depth in the lung than predicted by the Vt delivered. There is also coaxial or bidirectional gas movement. At the center of the airway, gas (O2) moves into the lung, whereas at the periphery gas (CO2) moves to the mouth.
3. Taylor dispersion (augmented dispersion): High-velocity gas movement enhances the development of turbulence in the conducting airways, causing eddies and swirling gas movement. This movement encourages dispersion of gas laterally and centrally.
4. Cardiogenic oscillation: The oscillations of the circulatory system assist gas movement especially at very high ventilatory frequencies.
5. Out-of-phase HFO: If the oscillation is out of phase with the normal resonance frequency of the lung, lateral and distal gas movement is enhanced.
6. Convection in larger airways: Most gas movement is still by gross movement of gas from one place to another.
7. At the alveolar level molecular diffusion accounts for gas movement.
8. The lung may be considered in three zones with reference to HFV (see Figure 42-5).
a. Zone 1 is the large airways in which flow is turbulent. Here convection and Taylor dispersion are responsible primarily for gas movement.
b. Zone 2 is the lower airways, where flow is laminar. Here gas movement is primarily by coaxial flow and asymmetric velocity profiles.
c. Zone 3 is lung parenchyma, where no bulk movement occurs. Here gas movement is primarily by cardiac oscillations, pendelluft, and molecular diffusion.
9. Gas movement in the upper airway generally seems to be the major limiting factor in HFV.
III Ventilation and Oxygenation
A With HFPPV, HFJV, and HFPV, ventilation and oxygenation are linked as in conventional ventilation. However, with HFO most consider the two processes uncoupled.
B Ventilation during HFO depends on
C CO2 elimination is generally directly related to the delta pressure and the bias flow in HFO. Increasing both tends to increase Vt.
D However, CO2 elimination is inversely related to rate in HFO (i.e., as rate decreases, CO2 elimination increases). The reason for this is that a decrease in rate in HFO results in an increase in Vt.
1. A lower rate increases inspiratory time, allowing more time for Vt delivery.
2. This also means that less of the delta pressure dissipates in the larger airways. More pressure extends into the lower respiratory tract.
3. At low rates (3 Hz) and high delta pressures (90 cm H2O), as has been applied in adults, Vt with HFO approaches that of normal breathing approximately 5 to 6 ml/kg of ideal body weight.
4. At rapid rates as seen in neonates (8 to 15 Hz) Vt may be smaller than deadspace volume (≤1 ml/kg ideal body weight).
E Oxygenation in HFO depends on mean airway pressure.
1. The greater the mean airway pressure, the greater the functional residual capacity (FRC; or PEEP equivalent).
2. I:E affects mean airway pressure somewhat. The longer the inspiratory time, the greater the mean airway pressure.
3. Increasing the bias flow has a direct effect on mean airway pressure.
IV Respiratory and Cardiovascular Effects of HFV
A HFV when applied properly maintains the lung in a state of hyperinflation. This is more pronounced the greater the compliance of the lung. However, even with acute lung injury (acute respiratory distress syndrome [ARDS]), auto-PEEP develops with HFPPV, HFJV, and HFPV. Auto-PEEP is not developed during HFO.
B HFV does not appear to alter surfactant production to the same extent as conventional ventilation. Compliance decreases over time with conventional ventilation but does not seem to be altered with HFV.
C As long as PCO2 is maintained at a normal or below normal level, apnea is common with the use of HFV. Although spontaneous breathing develops during rapid eye movement sleep, it is believed that inhibition of phrenic activity via the vagus nerve and activation of mechanoreceptors inhibit breathing at other times during HFV in some patients.
D The frequency of barotrauma is equivalent to that of conventional ventilation.
E Hemodynamic compromise is similar to that with conventional ventilation.
F The other overall respiratory and cardiovascular effects of HFV are similar to conventional ventilation.
A Upper airway surgery and bronchoscopy
1. HFPPV and HFJV are preferred over conventional ventilation in these clinical settings.
2. Both are capable of providing more efficient gas exchange than conventional ventilation with an open airway.
1. Initially HFV was considered superior to conventional ventilation in the presence of a large air leak.
2. At least theoretically gas distribution with conventional ventilation depends primarily on compliance, whereas as rate increases, gas distribution depends more on airway resistance.
3. Recent data indicate conventional ventilation and HFV are equally capable of ventilating in the presence of a bronchopulmonary fistula if acute lung injury is also present.
4. With major air leaks without acute lung injury, HFV may ventilate more effectively.
1. In the adult population HFV provides no advantage over conventional ventilation. Based on currently available data they are equivalent.
2. In the neonatal population HFO has been used to treat any severely ill neonate and has been considered superior to conventional ventilation. However, the use of surfactant, lung protective ventilatory strategies, and nitric oxide during ventilation has resulted in no demonstrable benefit in recent clinical trials from HFO over conventional ventilation.
A Extreme care must be taken with the use of HFV systems because of the potential for tremendous increases in airway pressure in a short period.
B In addition to alarms, mechanisms to abort gas delivery must be included. This is of particular concern with HFJV.
A A major problem with HFJV is humidification. No efficient mechanism to appropriately humidify the 20 to 60 L of gas delivered per minute during HFJV is available.
B As a result of insufficient humidification, necrotizing tracheobronchitis and squamous metaplasia of the bronchial mucosa with submucosal inflammatory cell infiltration are common during HFJV.
C However, gas used during HFPPV, HFO, and HFPV can be easily humidified and causes no greater problems than conventional ventilation.
VIII The Use of HFO in Adult ARDS
1. FIO2 at or greater than that used during CMV
2. Rate: 3 to 8 Hz, generally started at 5 Hz
3. Delta pressure: 40 to 90 cm H2O, generally started at 60 cm H2O
4. I:E: 1:1 or 1:2, generally started at 1:1
6. Mean airway pressure: between 20 and 35 cm H2O initially
a. 3 to 5 cm H2O higher than that during CMV
b. Set at 35 to 40 cm H2O to recruit the lung then decrease to the lowest level maintaining oxygenation.
7. When mean airway pressure can be decreased to 20 cm H2O, patients are frequently converted to conventional ventilation at the same mean airway pressure then weaned as tolerated.