65
Herpes zoster (shingles)

The unilateral herpes zoster vesicles are typically confined to one or two dermatomes. This is a T4 distribution. The primary lesion is an umbilicated vesicle. Pain often precedes the eruption.

Herpes zoster vesicles turn cloudy; central umbilication evident. The grouped lesions are nearly confluent. The area may ultimately turn necrotic if there is underlying immunocompromise.
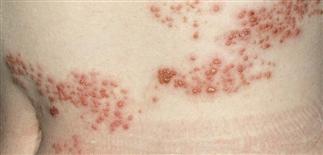
An obvious dermatomal distribution of vesicles on an erythematous base is classic of herpes zoster. The area may itch or be very painful or uncomfortable to even fine touch.

Involvement of the mandibular division of the fifth cranial nerve with vesicles along this distribution. Vesicles do not extend beyond the midline.
DESCRIPTION
Viral infection generally involving skin of single or adjacent dermatomes. Result of reactivation of varicella virus that entered cutaneous nerves during earlier chickenpox.
HISTORY
• Incidence increases with age. • Age, immunosuppressive drugs, lymphoma, fatigue, emotional upsets, and radiation therapy have been implicated in virus reactivation. • Elderly at greater risk for debilitating segmental pain, which can continue for months. • Pain may simulate pleurisy, myocardial infarction, abdominal disease, migraine. • Constitutional symptoms, headache, photophobia, and malaise may precede eruption by several days. Fever uncommon.
PHYSICAL FINDINGS
• Pain, itching, or burning may precede eruption by 4–5 days. • Eruption may involve one or two adjacent dermatomes. Non-contiguous multidermatomal lesions more common in immunosuppressed. • Begins with red swollen plaques of various sizes; spreads to involve part or all of dermatome. • Vesicles, varying in size, in clusters on erythematous base, become cloudy with purulent fluid by day 3 or 4. • Vesicles either umbilicate or rupture before crusting. • Elderly or debilitated patients may have a prolonged, difficult course, with hemorrhagic blisters, necrosis, secondary bacterial infection, extensive scarring. • Complications can include peripheral nerve palsies, encephalitis, myelitis, contralateral hemiparesis.
OPHTHALMIC ZOSTER
• Involvement of ophthalmic nerve. • Rash extends from eye level to skull vertex but does not cross midline. • Vesicles on nose side or tip (Hutchinson sign) associated with most serious ocular complications. • Of patients not treated with antiviral therapy, 50% will develop ocular complications (keratopathy, episcleritis, iritis). Oral antiviral therapy results in decreased frequency of late ocular complications. • Refer to an ophthalmologist.
TREATMENT
• Topical therapy may be soothing: cool tap water in a wet dressing, applied 20 min several times a day. • Oral steroids may decrease acute pain but have no effect on postherpetic neuralgia and can result in complications. • Oral antiviral drugs decrease acute pain, inflammation, vesicle formation, viral shedding. • May reduce duration and severity of postherpetic neuralgia by treating acute herpes zoster with valacyclovir or famciclovir. • Treatment most effective when started within first 48 h, but reasonable to consider antiviral therapy if all lesions not yet crusted. • Recommended oral dosage for adults: 7–10 days of acyclovir (Zovirax) 800 mg five times a day, valacyclovir (Valtrex) 1000 mg t.i.d., or famciclovir (Famvir) 500 mg t.i.d. All three drugs safe, well tolerated. Adjust dose for renal insufficiency. • Empiric treatment if older than 50, immunocompromised, or trigeminal zoster.







