Chapter Seventeen. Herbs that subdue the Liver-Yang and extinguish Liver-Wind
 |
1. What are the pathological changes and manifestations in the syndromes of Liver-Yang rising and Liver-Wind?
The syndrome of Liver-Yang rising is caused by Liver-Yin deficiency. It is often seen in people over 50 years old or who are suffering from certain chronic diseases that injure the Liver-Yin. As soon as the Liver-Yin fails to control the Liver-Yang, the Yang rises. The manifestations are dizziness with a slightly tight sensation in the head, headache, blurred vision and tinnitus. In a severe case, there is irritability, dream-disturbed sleep and a distending pain in the hypochondriac region and the patient prefers a quiet and relaxing environment. If the Liver-Yang and Heat disturb the Stomach, patients may have a red face, a dry and bitter taste in the mouth, nausea or belching. The tongue body is red, or red only on the border, and the coating is thin, dry and yellow. The pulse is thready and wiry, or thready, wiry and rapid. In clinical practice, this syndrome is often seen in hypertension, menopausal syndrome, neurotinnitus, nervous deafness and glaucoma.
If the Liver-Yang is not controlled with proper treatment, it may turn to Liver-Wind, especially in those with a Yang constitution, or in conditions of rage, high stress, eating too much spicy food or taking certain medications. At that moment, the Liver-Yang rises rapidly and stirs up the Wind. This is called ‘Liver-Yang stirs up the Wind’ or ‘Liver-Yang turns to Wind’. Since the Liver controls all the tendons, the symptoms of Liver-Wind are characterized by tremors or spasms of the limbs, severe dizziness, nausea, vomiting, tingling or numbness of the limbs, and loss of balance in standing or walking. In severe cases, Liver-Wind may disturb the normal circulation of Qi and Blood, and rebellious Qi and Blood, as well as Fire and Phlegm, attack the head, block the meridians and cover the Mind. The patient may suddenly lose consciousness and afterwards will have hemiplegia and deviation of the eyes and mouth. In this case, the tongue body is red, the coating is yellow and dry, or yellow and sticky, and the pulse is wiry, forceful and rapid. In clinical practice, this syndrome is often seen in epilepsy, convulsions in infectious disease, severe cases of hypertension and glaucoma, facial paralysis, facial spasms and cerebrovascular accident and its sequelae.
2. What are the treatment principles for the syndromes of Liver-Yang rising and Liver-Wind? What precautions should be observed in their treatment?
Since the syndrome of Liver-Yang rising is the result of Liver-Yin deficiency, one of the treatment principles is to nourish the Liver-Yin so as to control the Liver-Yang, and this is especially necessary in the mild, chronic cases of Liver-Yang rising. However, because the Liver-Yang has already left its original place, the Lower Jiao, it is not so easy to get it to return to its place quickly by means of nourishing the Yin. So a second principle of the treatment is to anchor the Yang and sedate the Liver so as to build up a new balance between the Liver-Yin and Liver-Yang, especially in acute cases. In a severe case of Liver-Yang rising, the procedure of anchoring the Yang should be carried out at once so as to stop the development of the pathological changes and prevent the occurrence of Liver-Wind syndrome.
If the Liver-Wind has already been stirred up by the suddenly rising Liver-Yang, the treatment principles mentioned above are not enough to handle the Wind, so methods that strongly direct the Liver-Yang to descend, pacify the Liver and extinguish Wind should be applied immediately.
In the treatment of Liver-Yang rising or Liver-Wind, it is important to make a clear differentiation of the stage of the disorder and the primary and secondary steps of treatment. If a patient has family history of hypertension, is over 50 years old and feels quite stressed, and the blood pressure is slightly higher than normal, treatment should be given to nourish the Liver-Yin and calm the Liver-Yang. If, at certain moments, such as in the springtime, when under high stress or in a rage, the patient’s blood pressure rises quickly, and there are all the obvious symptoms of Liver-Yang rising, then the treatment to anchor the Yang and sedate the Liver should be given immediately. If the patient not only has the symptoms of Liver-Yang rising, but also feels tingling in the fingers or limbs, and loses balance in walking, then treatment to extinguish Liver-Wind and anchor the Yang must be given immediately.
To treat patients with a syndrome of Liver-Yang rising and Liver Wind, it is also important to advise the patient to avoid all the factors that may contribute to the Liver-Yang rising, such as herbs that move upwards and outwards, alcohol, spicy food, stress and rage.
3. What are the characteristics of the substances that anchor the Liver-Yang and extinguish Liver-Wind? What precautions should be observed when these substances are prescribed?
The substances that sedate and anchor the Liver-Yang and extinguish Liver-Wind are used for acute and subacute conditions of Liver-Yang rising or Liver-Wind and they have the following characteristics.
Mineral substances
In TCM, mineral substances are considered to have a descending tendency because they are heavy in weight. They can direct the Liver-Yang downwards and are also able to bring down the Liver-Wind and rebellious Qi and Blood, which have been stirred up by the rapidly rising Liver-Yang. The commonly used substances are Shi Jue Ming ( Haliotidis concha), Long Gu ( Mastodi fossilium ossis), Mu Li ( Ostrea concha), Ci Shi ( Magnetitum), Zhen Zhu Mu ( Concha margaritifera usta) and Dai Zhe Shi ( Haematitum).
Sedating the Heart-Spirit and calming the Mind
Since the Liver is the mother organ of the Heart, Liver-Yang rising may cause Heart-Fire blazing. In most of the cases of Liver-Yang rising there are also symptoms of Heart-Fire disturbance, such as restlessness, anxiety, irritability, insomnia, a bitter taste in the mouth and a red face. The substances that bring down the Liver-Yang are also able to sedate the Heart-Spirit and calm the Mind—examples are Ci Shi, Long Gu, Mu Li and Zhen Zhu Mu.
Usage of worms for opening the collaterals and extinguishing Wind and relieving spasms
It is considered in TCM that worms are able to get into the small collaterals because they have the habit of drilling holes or passing through cracks. Worms that enter the Liver meridian can open meridians and collaterals so as to extinguish Wind and relieve spasms. The worms used are Di Long ( Pheretima), Jiang Can ( Bombyx batrycatus), Quan Xie ( Scorpio)* and Wu Gong ( Scolopendra)*.
In clinical practice, it is important to know the precautions and contraindications for the usage of these substances. Since the mineral substances are heavy in weight, they are also heavy on the Stomach. For patients who have a weakness in the Middle Jiao, the mineral substances should be used in a smaller dosage, shorter treatment course or combined with other herbs that protect the Stomach. Since they are heavy on the Stomach and can strongly direct the Liver-Yang downwards, they are used only in the acute and subacute conditions. In the syndrome of Liver-Yin deficiency with Liver-Yang rising, the treatment should be based on tonifying the Yin and pacifying the Liver-Yang. In addition, Dai Zhe Shi, Quan Xie and Wu Gong are poisonous substances, so the dosages should be controlled carefully. Lastly, these mineral substances should not be used by pregnant women.
4. Shi Jue Ming ( Haliotidis concha), Zhen Zhu Mu ( Concha margaritifera usta), Ci Shi ( Magnetitum), Long Gu ( Mastodi fossilium ossis) and Dai Zhe Shi ( Haematitum) can all be used for the syndromes of Liver-Yang rising and Liver-Wind. What are the differences between them?
These five herbs are all mineral substances and are commonly used for the syndrome of Kidney-Yin and Liver-Yin deficiency and Liver-Yang rising with Liver-Wind. However, there are some differences between their functions.
Shi Jue Ming is salty and slightly cold, and enters the Kidney and Liver meridians. Saltiness and Cold possess reducing and descending capacities and a heavy mineral substance is considered to have a downward-moving tendency. Shi Jue Ming is able to direct the Liver-Yang strongly downwards, clear the Liver-Fire and therefore extinguish the Liver-Wind. It is commonly used to treat the syndromes of Liver-Yang rising and Liver-Wind. In clinical practice, it can treat headache, dizziness, blurred vision, irritability, dream-disturbed sleep and tingling or numbness of the fingers and limbs, such as seen in hypertension. It is also able to brighten the eyes and treat disorders of the eyes due to Liver-Yang rising and Liver-Fire, such as blurred vision, hypopsia, asthenopia, optic atrophy, glaucoma, primary cataract, conjunctivitis and Bitot’s spot.
Zhen Zhu Mu is salty and cold, and enters the Heart and Liver meridians. Compared with Shi Jue Ming, it has the same function of descending the Liver-Yang and Liver-Wind, and it can be used for the same disorders, but the action of this substance is weaker. However, the strong point of this substance is that it can calm the Mind as it enters the Heart meridian and clear the Heat there. In clinical practice, if the patient complains of restless sleep, insomnia and palpitations, as well as the symptoms of Liver-Yang rising, then Zen Zhu Mu is the better choice.
Ci Shi is pungent, salty and cold, and enters the Liver and Kidney meridians. It is as strong as Shi Jue Ming in directing the Liver-Yang downwards, but is less strong in calming the Liver-Wind, so is less effective for treating headache, dizziness, tingling of the fingers or numbness of the limbs. However, Ci Shi is able to calm the Wind caused by Heart-Fire, such as seen in convulsions due to high fever in children. Meanwhile, it has a strong action in strengthening and stabilizing the Kidney-Qi and Essence, and is used for treating tinnitus, deafness and hypopsia, as well as shortness of breath. Compared with Zhen Zhu Mu, Ci Shi has a stronger action in calming the Mind, and settling and tranquilizing the Heart-Spirit, so is used not only in insomnia and restlessness, but also in phobia, anxiety and manic–depressive psychosis.
Long Gu is sweet, astringent and neutral, and enters the Heart, Liver and Kidney meridians. It is a very good substance for directing the Liver-Yang downwards and calming Liver-Wind. Since it is sweet and neutral, and is less irritating to the Stomach, it can be used for a longer period of time—for instance, in hypertension. It is also often combined with other substances that direct the Liver-Yang downwards, and which are very cold and heavy—for instance, Dai Zhe Shi and Ci Shi.
Long Gu makes the action of bringing down the Liver-Yang sufficient, so the dosages of the other substances that are too cold and salty can be reduced. Like Zhen Zhu Mu and Ci Shi, Long Gu can also be used to calm the Mind and control anxiety. Because it is an astringent substance, it is able to stabilize the Body Fluids and Essence, so is more suitable for treatment in menopause when the patient has hypertension, emotional disorders, sleep disorders, hot flushes and night sweating.
Dai Zhe Shi is bitter and cold, and enters the Liver and Pericardium meridians. It is an important substance for directing the Yang downwards. It is also the strongest of these five substances for bringing down the Liver-Yang and extinguishing the Wind. It can intensively and quickly direct the Yang, Wind, Fire, Phlegm, Qi and Blood downwards, so it is often used for acute situations—for instance, when the blood pressure rises rapidly, or the patient has a cerebrovascular accident or some severe infectious disease. Symptoms that may be present include severe headache with heavy and distending sensations, tinnitus, stiffness of the neck, dizziness and loss of balance in walking, belching, nausea, vomiting, stifling in the chest and fullness in the Stomach and hypochondriac region, nose bleeding or vomiting of Blood. However, since Dai Ze Shi is a heavy, cold and bitter substance, can easily injure the Stomach, and contains a tiny amount of arsenic, it cannot be used in large dosages or for a long period of time.
5. What are the differences between Tian Ma ( Gastrodiae rhizoma)** and Gou Teng ( Uncariae ramulus cum uncis) in the function of extinguishing Liver-Wind?
Tian Ma and Gou Teng both are sweet, enter the Liver meridian, and are able to pacify the Liver and extinguish the Liver-Wind. They are used to treat dizziness, headache, convulsions, tremor and spasm caused by Liver-Wind. They are often used together to accentuate each other’s therapeutic actions. However, they have some individual characteristics in both nature and function, so the clinical applications are also different.
Tian Ma is sweet and neutral, and has a moderate and moist nature. The characteristic of this herb is that it can extinguish internal Wind as well as expel external Wind. In clinical practice, it is good at treating dizziness and headache due to deficiency of the Liver-Yin and Blood. It is also used to treat dizziness with nausea and vomiting caused by disturbance of Wind-Phlegm. If it is combined with the herbs that cool the Liver, it is effective for calming spasm and convulsions from high fever; if it is used together with the herbs that promote Qi movement and Blood circulation, it can treat stiff, painful, numb and tingling limbs, such as seen in Bi syndrome or the sequelae of cerebrovascular accident. Since it is so often used in different types of Wind syndrome, it has acquired the name ‘grass of settling Wind’.
Gou Teng is sweet and cold. Although it is not so widely used as Tian Ma for treating various Wind syndromes, it has an obvious strong function of clearing and reducing Liver-Heat, no matter whether Excess-Heat or Empty-Heat; therefore it can calm Wind. It is used to treat dizziness, headache, tinnitus, irritability, and red and irritated eyes. Because it enters the Pericardium meridian, it is also very effective for treating convulsions in children when high fever is present that is caused by Liver-Fire and Heart-Fire.
6. Quan Xie ( Scorpio)*, Wu Gong ( Scolopendra)* and Di Long ( Pheretima) are all able to extinguish Liver-Wind, relieve spasms and control tremor. What are the differences between them?
Quan Xie, Wu Gong and Di Long are all able to extinguish Liver-Wind, relieve spasms, control tremor, open the meridians and stop pain. They are used in the treatment of convulsions, epilepsy, tetanus, hemiplegia, facial paralysis, facial spasm and chronic arthritis.
Quan Xie and Wu Gong are pungent and poisonous; both are able to extinguish Liver-Wind, release spasm, open the meridians and stop pain. The functions of these two substances are almost the same, but Wu Gong is the stronger. In clinical practice, Quan Xie is more suitable for treating tremor due to Liver-Wind and Heat. It is also effective in opening up the collaterals, relieving pain and reducing the speed of deformation and stiffness of the joints. Wu Gong is warm and more pungent, can intensively relieve spasms, and is more suitable for severe spasms with internal Cold. It can also remove the toxin from poisonous snakebites, sores and carbuncles. Although there are differences between Quan Xie and Wu Gong, they are often used together because these two substances can strongly enhance each other’s actions; therefore the dosage of each substance can be reduced as they are poisonous.
Di Long is salty and cold; its action in extinguishing the Wind is weaker than that of either Quan Xie or Wu Gong, but its effect in clearing Liver-Heat is the strongest of the three. In clinical practice, it is more suitable for treating convulsions, tremor with irritability or fever. When it is used together with Tian Ma ( Gastrodiae rhizoma)** and Quan Xie, it becomes more effective. Moreover, Di Long particularly enters the collaterals, and is able to break up obstructions, so is used for Bi syndrome and hemiplegia when the limbs are stiff, weak, numb and painful.
7. Di Long ( Pheretima) and Jiang Can ( Bombyx batrycatus) can both extinguish Wind and are used for facial paralysis and facial spasm. What are the differences between them?
Di Long and Jiang Can both can effectively open up collaterals and relieve spasms. In clinical practice, they are often used for facial paralysis and facial spasms. However, Di Long is salty and cold, and is good at clearing Heat, controlling Liver-Wind, relieving spasms and stopping pain, whereas Jiang Can is neutral and pungent, and is able to remove Phlegm obstruction from the collaterals so can relieve spasms, numbness and paralysis. Because they treat facial paralysis or spasms by different approaches, they are often used together in clinical practice.
8. Jiang Can ( Bombyx batrycatus), Bai Ji Li ( Tribuli fructus), Chan Tui ( Cicadae periostracum) and Jing Jie ( Schizonepetae herba) are all able to relieve itching and treat itchy skin lesions or rashes. What are the differences between them?
These four herbs are effective for relieving itching because they are pungent and light, and are able to expel Wind-Heat. They are often used for skin diseases such as urticaria, eczema, neurodermatitis and pruritus; they can be also used for treating some allergic disorders such as hay fever or some infectious diseases with pathological changes on the skin, such as chickenpox, rubella and measles.
Of these four substances, Chan Tui and Jing Jie are particularly often used in cases caused by external Wind, such as infectious diseases of children and allergies.
Jiang Can and Bai Ji Li are able not only to expel external Wind, but also to extinguish internal Wind, the Liver-Wind. They are more suitable for use when the patient has Liver-Yin and Blood deficiency, and disturbance of the Liver-Wind, such as seen in pruritus in elderly people, skin diseases starting or worsening in stressful situations, itchy rashes in the evening, in the night or after menstruation, and chronic skin diseases. Since external Wind and internal Wind often coexist—for instance, the itch may not only be worse in the above conditions, but also when the weather changes, after taking spicy food or during cold infections—therefore substances that expel external Wind and those that extinguish internal Wind can be used together.
Comparisons of strength and temperature in herbs that sedate the Liver-Yang and extinguish Liver-Wind
 |
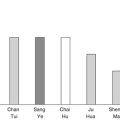
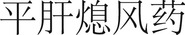
| Fig. 17.1. |
| Comparison of the substances that anchor the Liver-Yang. Dai Zhe Shi ( Haematitum), Shi Jue Ming ( Haliotidis concha), Zi Bei Chi ( Erosaria caputserpentis), Zhen Zhu Mu ( Concha margaritifera usta), Long Gu ( Mastodi fossilium ossis), Ci Shi ( Magnetitum), Mu Li ( Ostrea concha), Tian Ma ( Gastrodiae rhizoma)**. |
 |
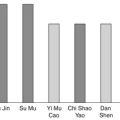
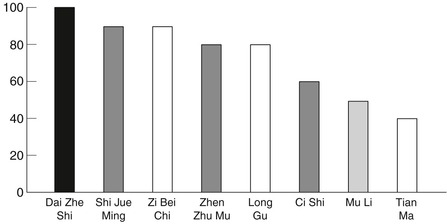
| Fig. 17.2. |
| Comparison of the herbs that extinguish Liver-Wind and subdue the Liver-Yang. Shi Jue Ming ( Haliotidis concha), Zi Bei Chi ( Erosaria caputserpentis), Long Gu ( Mastodi fossilium ossis) and Tian Ma ( Gastrodiae rhizoma)**. |
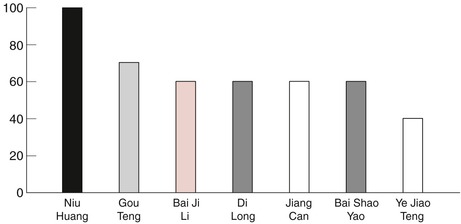 |
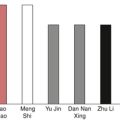
| Fig. 17.3. |
| Comparison of the herbs that cool the Liver or disperse Liver-Heat and extinguish Wind. Niu Huang ( Bovis calculus)**, Gou Teng ( Uncariae ramulus cum uncis), Bai Ji Li ( Tribuli fructus), Di Long ( Pheretima), Jiang Can ( Bombyx batrycatus), Bai Shao Yao ( Paeoniae radix lactiflora), Ye Jiao Teng ( Polygoni multiflori caulis). |
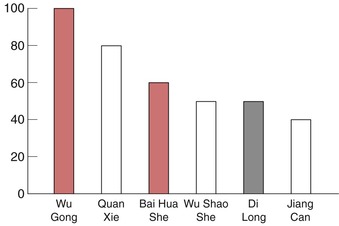 |
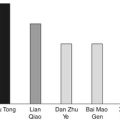
| Fig. 17.4. |
| Comparison of the substances that open the collaterals and extinguish Wind. Wu Gong ( Scolopendra)*, Quan Xie ( Scorpio)*, Bai Hua She ( Agkistrodon acutus)*, Wu Shao She ( Zaocys), Di Long ( Pheretima), Jiang Can ( Bombyx batrycatus). |