Hepatomegaly
Hepatomegaly is enlargement of the liver. The most common causes in the UK are cirrhosis, cardiac failure and secondary malignancy.
History
Hepatitis/infection
Predisposing factors include a history of contact with hepatitis, blood transfusion, drug abuse, homosexuals, haemophiliacs, health workers, the institutionalised (e.g. homes, prison) and travel abroad to endemic areas. Amoebiasis occurs worldwide, and hepatitis B is prevalent in the tropics and Mediterranean areas. Hydatid disease is more common in sheep-rearing countries, e.g. Australia, Africa, Wales. Leptospirosis can result from swimming in rat-infested waters. History of alcohol abuse predisposes to alcoholic cirrhosis. Chronic active hepatitis should be considered with a history of alcohol, hepatitis B or hepatitis C. In the majority of hepatitis/infection cases, the patient presents with general malaise, pyrexia, weight loss and jaundice.
Congestion
History of congestive cardiac failure may be evident and the patient often complains of upper abdominal pain caused by a tender liver due to stretching of the liver capsule. With constrictive pericarditis, there is often a history of TB but it may follow any cause of pericarditis, e.g. acute renal failure. Budd–Chiari syndrome is hepatic vein thrombosis. A history of taking the contraceptive pill may be contributory. Tumour may also cause Budd–Chiari syndrome. It presents insidiously with portal hypertension, jaundice and cirrhosis.
Infiltration
There is usually a history of alcohol abuse with fatty infiltration. Secondary amyloidosis follows chronic infection/inflammation, e.g. rheumatoid arthritis, bronchiectasis, inflammatory bowel disease.
Biliary tract disease
There may be a history of biliary tract obstruction, e.g. carcinoma of the pancreas or stricture of the common bile duct. Sclerosing cholangitis causes jaundice and fevers and is associated with inflammatory bowel disease. Primary biliary cirrhosis is of unknown aetiology. Some 90% of the patients are female. It presents with obstructive jaundice, pruritus and hepatosplenomegaly. The patient will complain of dark urine and pale stools.
Malignancy
The chief cause is metastases from a known malignancy, which may have been treated, e.g. gastrointestinal tract or bronchus. Hepatoma is rare. With hepatoma, there may be a past history of hepatitis B infection, use of the contraceptive pill, aflatoxin exposure, or use of anabolic steroids. Myeloproliferative disease presents with tiredness, lethargy and spontaneous bruising.
Metabolic
Glycogen storage disease is rare. There is usually hepatomegaly from birth. The early features of haemochromatosis include fatigue, arthralgia and hepatomegaly. Skin pigmentation, diabetes and cardiac failure occur later.
Examination
Remember that a liver edge that is palpable is not always enlarged and may have been pushed down by pulmonary hyperinflation, e.g. emphysema. The upper border of the liver should therefore be identified by percussion and is usually at the level of the eighth rib in the midaxillary line. The edge of the liver can be sharp or rounded and its surface smooth or nodular.
Regular generalised enlargement without jaundice
Regular generalised enlargement with jaundice
Irregular generalised enlargement without jaundice
General
Carry out a general examination of the patient. Look for signs of liver failure: jaundice, flapping tremor, ascites, spider naevi, liver palms, clubbing, gynaecomastia, testicular atrophy, caput medusae, peripheral oedema, leuconychia, Dupuytren’s contracture, xanthoma, mental changes, coma, bruising. Look for Kayser–Fleischer rings (Wilson’s disease).
Congestion
Signs of CCF. Peripheral oedema. Tense tender liver. JVP ↑. With Budd–Chiari syndrome, there will be acute ascites and right upper quadrant pain. In constrictive pericarditis, there will be right heart failure associated with ascites. The JVP rises paradoxically with inspiration. Pulsus paradoxus. Hypotension.
Biliary tract disease
Deep jaundice. There may be a palpable mass associated with the primary malignancy. The gall bladder may be palpable with carcinoma of the head of the pancreas (Courvoisier’s law). With primary biliary cirrhosis, there will be clubbing, xanthomata, arthralgia, hirsutism, portal hypertension and skin pigmentation.
Storage disease
With haemochromatosis, there will be signs of portal hypertension and skin pigmentation.
Malignancy
Jaundice and ascites may be present. There may be an abdominal mass representing the primary malignancy. With myeloproliferative disorders, in addition to hepatomegaly, there will be splenomegaly and lymphadenopathy.
General Investigations
■ FBC, ESR
Hb ↓ malignancy, myeloproliferative disorders. WCC ↑ infection, leukaemia. Platelets ↓ leukaemia. ESR ↑ infection and malignancy.
■ U&Es
Creatinine. Often deranged in liver failure. Renal failure may occur with amyloidosis.
■ LFTs
Liver enzymes deranged in hepatitis. Alkaline phosphatase grossly raised in obstruction. The pattern varies according to the cause of hepatomegaly.
Specific Investigations
■ Serum iron, TIBC and serum ferritin
Abnormal in haemochromatosis.
■ Blood, urine, CSF culture
Positive in leptospirosis.
■ Antibody screen
Antimicrosomal antibodies raised in primary biliary cirrhosis.
■ Bone marrow aspiration
Myelofibrosis. Leukaemia.
■ US
Cirrhosis. Secondaries. Amoebic abscess. Hydatid cyst. Riedel’s lobe.
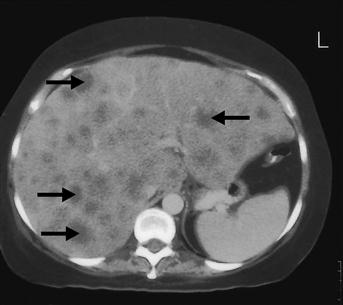
■ CT
Pancreatic lesions. Cirrhosis. Liver cysts.