Small tumors (< 3 cm without vascular invasion) are curable with resection, ablation, transplantation
IMAGING
General Features
CT Findings
• NECT
CLINICAL ISSUES
Presentation
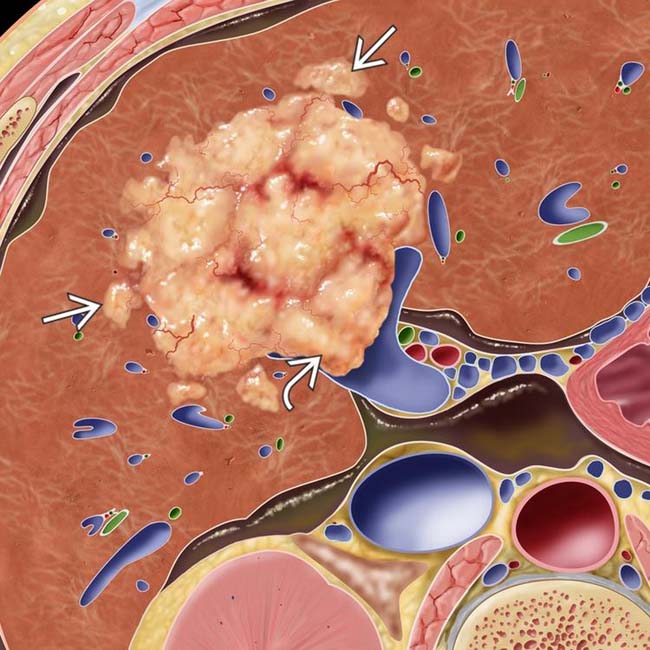
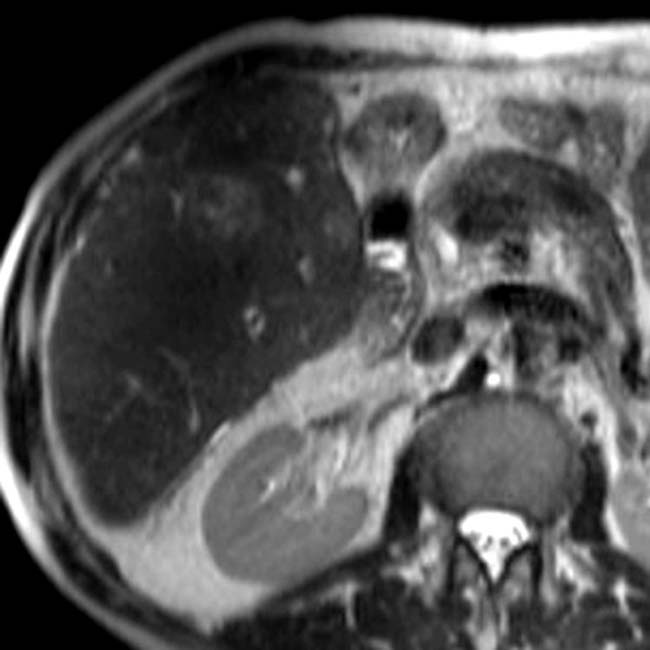
 . The surrounding liver is cirrhotic with a nodular contour, and there is ascites. Satellite nodules of HCC
. The surrounding liver is cirrhotic with a nodular contour, and there is ascites. Satellite nodules of HCC  surround the dominant mass.
surround the dominant mass.
 in a cirrhotic liver invading and occluding the posterior branch of the right portal vein
in a cirrhotic liver invading and occluding the posterior branch of the right portal vein  . Nonocclusive thrombus
. Nonocclusive thrombus  is present within the main portal vein. This HCC was hypervascular on arterial phase CECT.
is present within the main portal vein. This HCC was hypervascular on arterial phase CECT.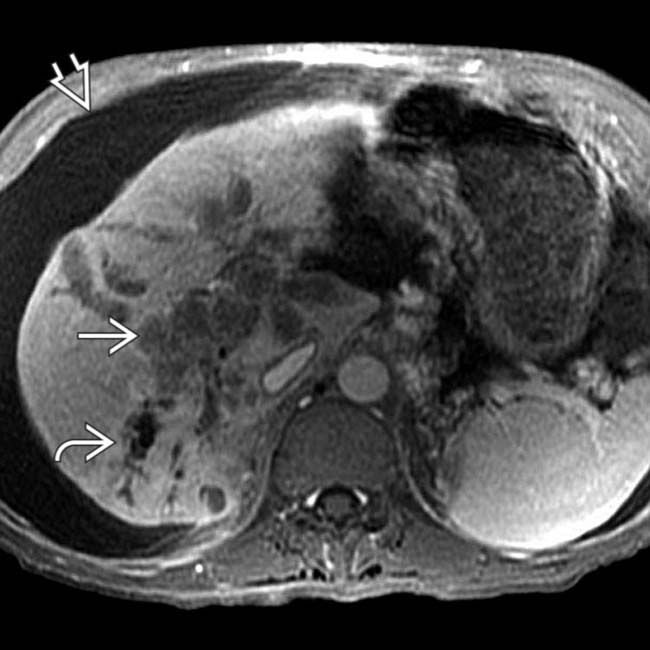
 that directly invades the portal vein and obstructs intrahepatic bile ducts
that directly invades the portal vein and obstructs intrahepatic bile ducts  . Note ascites
. Note ascites  and typical signs of cirrhosis.
and typical signs of cirrhosis.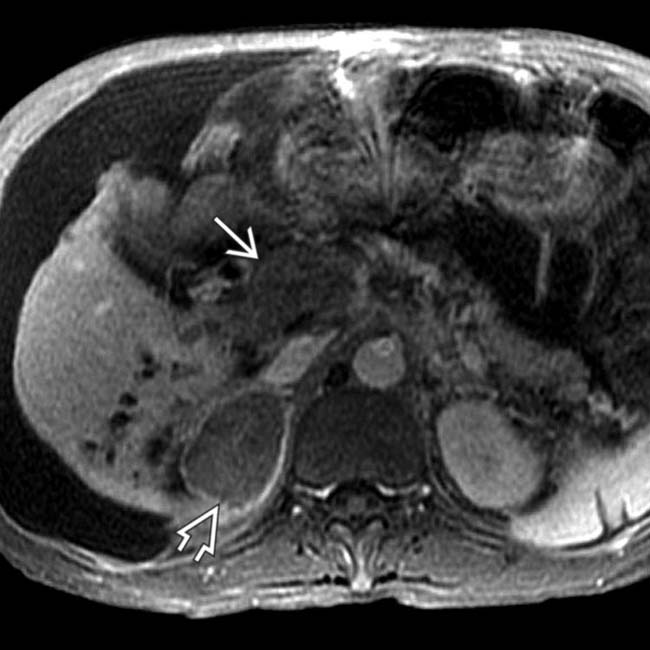
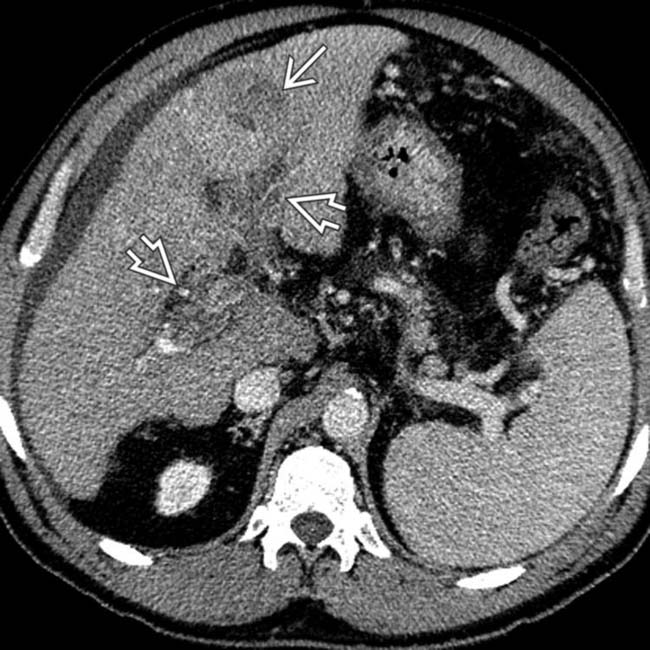
 , a metastasis that has a similar appearance to the tumor within the portal vein
, a metastasis that has a similar appearance to the tumor within the portal vein  . While extrahepatic metastases from HCC are uncommon, the adrenals are among the more common sites of these.
. While extrahepatic metastases from HCC are uncommon, the adrenals are among the more common sites of these.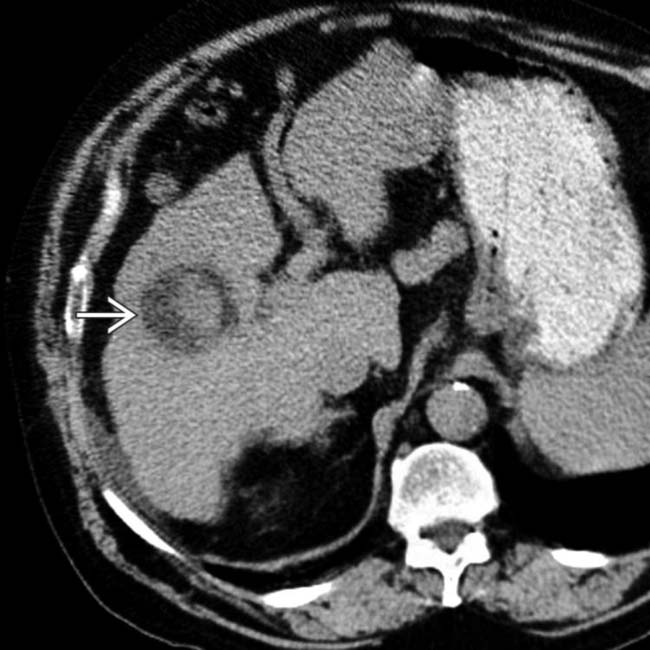
 with portions that are unusually hypodense due to the presence of fat within the tumor. The fatty elements within the HCC were still evident on portal venous phase CECT (not shown).
with portions that are unusually hypodense due to the presence of fat within the tumor. The fatty elements within the HCC were still evident on portal venous phase CECT (not shown).
 corresponding to the fatty foci within the HCC seen on CT. Macroscopic fat within a mass in a cirrhotic liver is very suggestive of HCC though it is present in only a minority of cases.
corresponding to the fatty foci within the HCC seen on CT. Macroscopic fat within a mass in a cirrhotic liver is very suggestive of HCC though it is present in only a minority of cases.
 and expansion of the left portal vein
and expansion of the left portal vein  by enhancing tumor thrombus.
by enhancing tumor thrombus.
 , as well as the portal vein tumor thrombus
, as well as the portal vein tumor thrombus  . The presence of the tumor thrombus is useful in distinguishing HCC from metastases, which rarely invade the portal vein.
. The presence of the tumor thrombus is useful in distinguishing HCC from metastases, which rarely invade the portal vein.
 . These are typical features of HCC that arise in a noncirrhotic liver, such as someone with chronic hepatitis B infection.
. These are typical features of HCC that arise in a noncirrhotic liver, such as someone with chronic hepatitis B infection.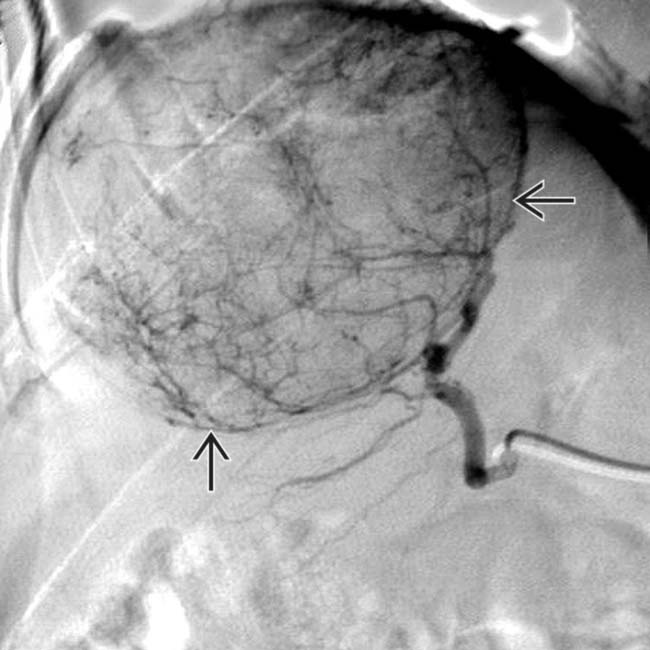
 along the periphery of the mass.
along the periphery of the mass.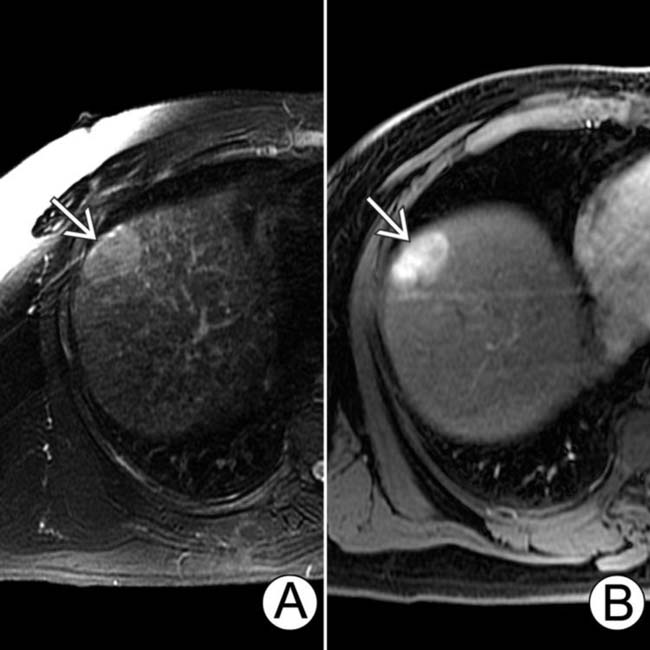
 that is slightly hyperintense to background liver. (B) The same lesion is hypervascular on arterial phase C+ T1WI.
that is slightly hyperintense to background liver. (B) The same lesion is hypervascular on arterial phase C+ T1WI.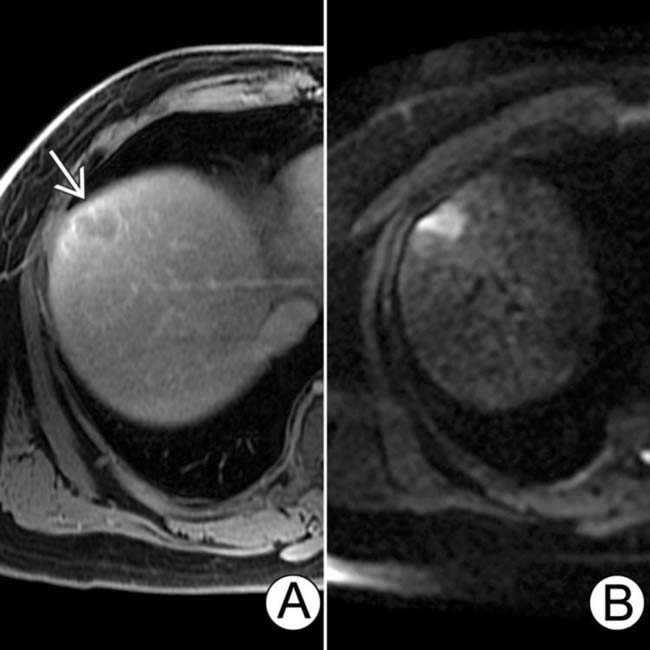
 demonstrates contrast washout and a capsule, very typical signs of HCC. Diffusion-weighted image (B) shows bright signal representing restricted diffusion, another typical feature of HCC.
demonstrates contrast washout and a capsule, very typical signs of HCC. Diffusion-weighted image (B) shows bright signal representing restricted diffusion, another typical feature of HCC.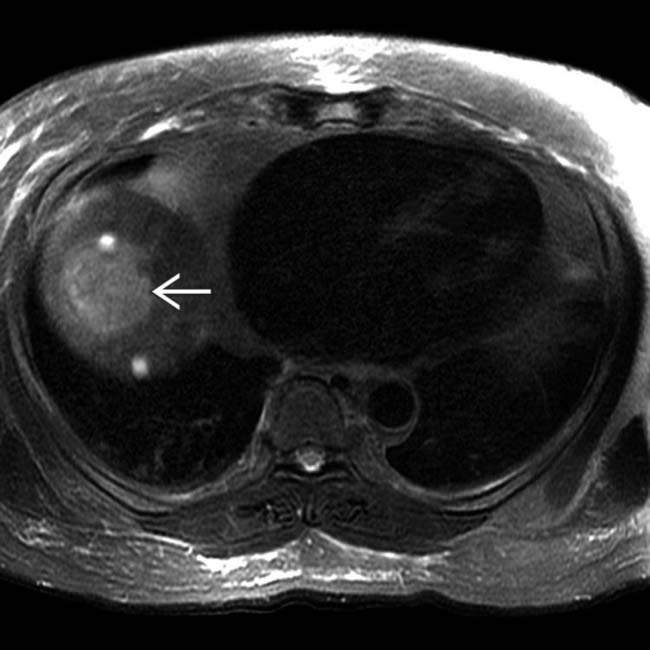
 in the hepatic dome, along with 2 smaller cysts.
in the hepatic dome, along with 2 smaller cysts.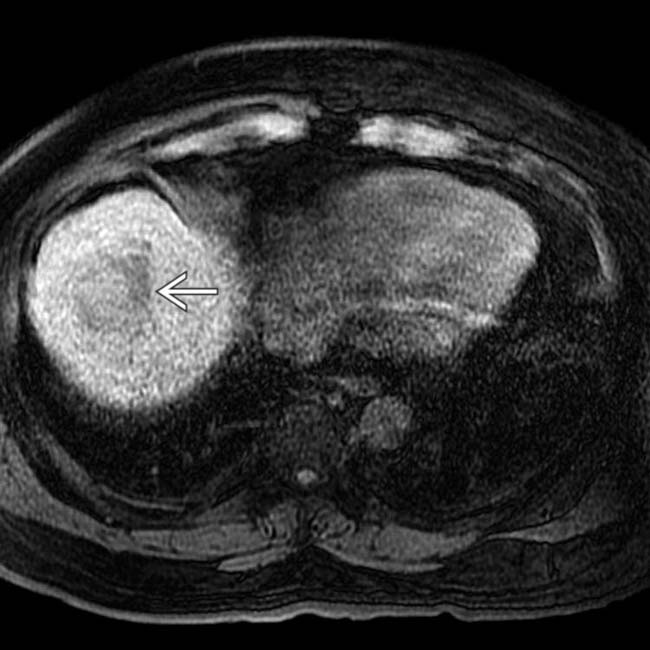
 as hypointense to surrounding liver.
as hypointense to surrounding liver.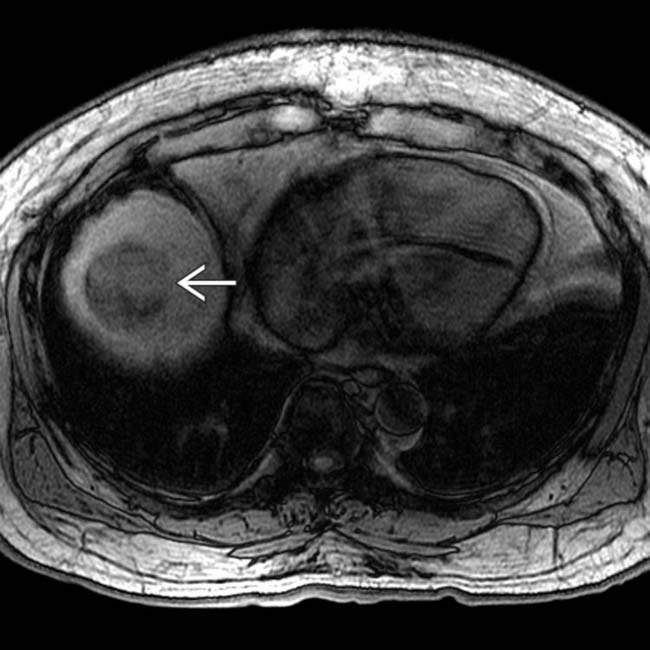
 , indicating lipid content. The presence of microscopic fat (as in this case) or macroscopic fat is a very suggestive sign of HCC in a mass within a cirrhotic liver.
, indicating lipid content. The presence of microscopic fat (as in this case) or macroscopic fat is a very suggestive sign of HCC in a mass within a cirrhotic liver.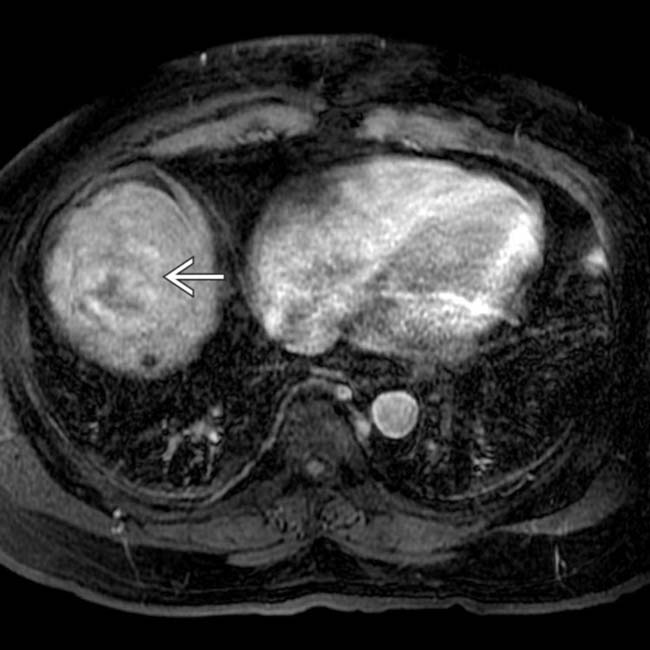
 , which is essentially diagnostic of HCC in this setting.
, which is essentially diagnostic of HCC in this setting.
 and a suggestion of a capsule
and a suggestion of a capsule  , another characteristic sign of HCC.
, another characteristic sign of HCC.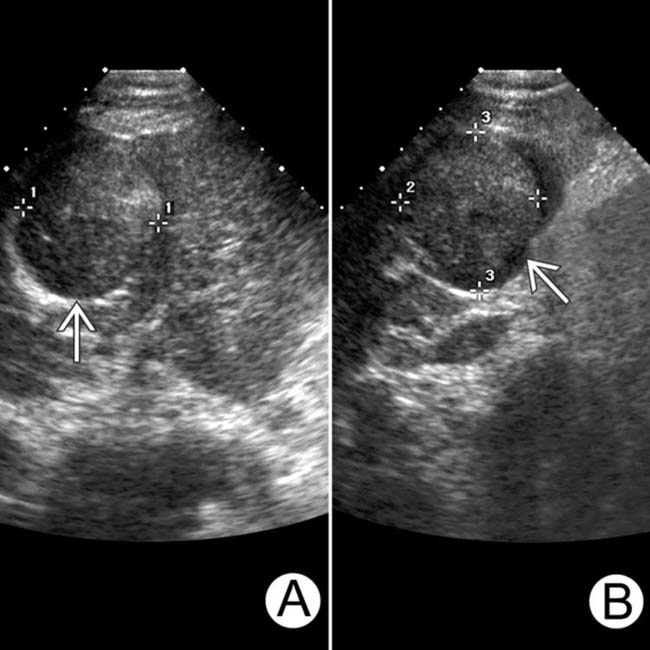
 that is solid, encapsulated, and nearly isoechoic to the background cirrhotic liver. This was interpreted as a solitary HCC.
that is solid, encapsulated, and nearly isoechoic to the background cirrhotic liver. This was interpreted as a solitary HCC.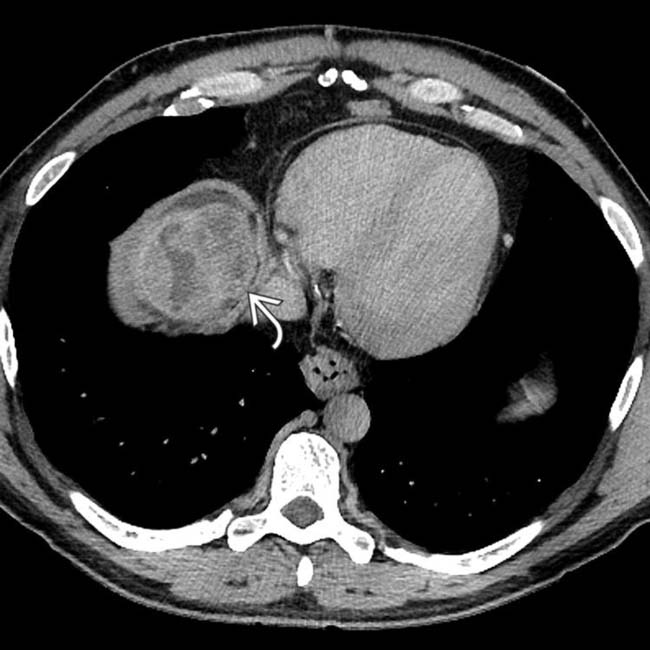
 in the hepatic dome, in addition to the mass identified at US, which was also seen on CT (not shown).
in the hepatic dome, in addition to the mass identified at US, which was also seen on CT (not shown).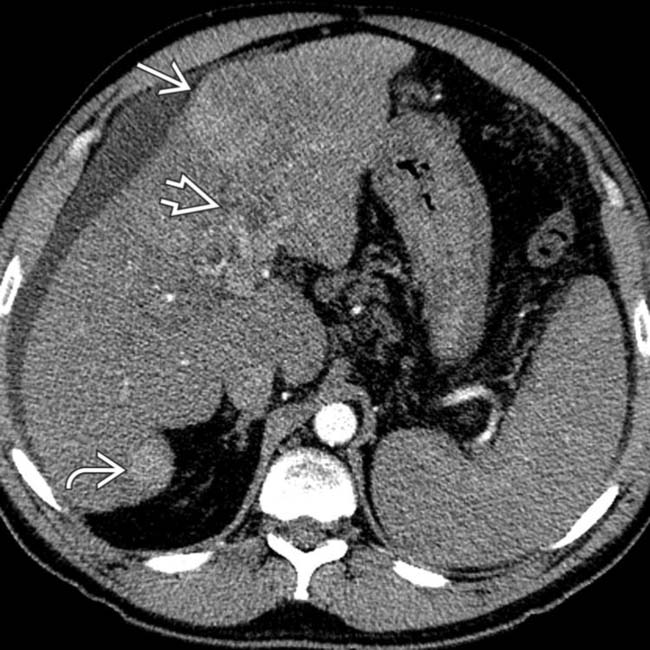
 seen on the sonogram as hypervascular to liver on this arterial phase image. In addition, a similar hypervascular HCC is identified in the posterior right lobe
seen on the sonogram as hypervascular to liver on this arterial phase image. In addition, a similar hypervascular HCC is identified in the posterior right lobe  , along with tumor thrombus in the portal vein
, along with tumor thrombus in the portal vein  .
.
 and tumor thrombus in the portal vein
and tumor thrombus in the portal vein  . These additional findings identified this patient as stage 4 HCC, limiting his therapeutic options.
. These additional findings identified this patient as stage 4 HCC, limiting his therapeutic options.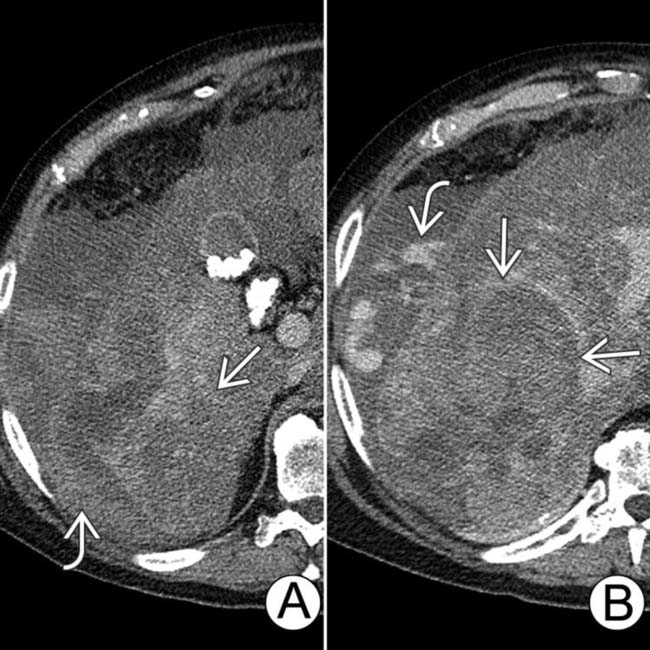
 . The source of the bleeding was an ruptured large HCC
. The source of the bleeding was an ruptured large HCC  . The liver is diffusely steatotic.
. The liver is diffusely steatotic.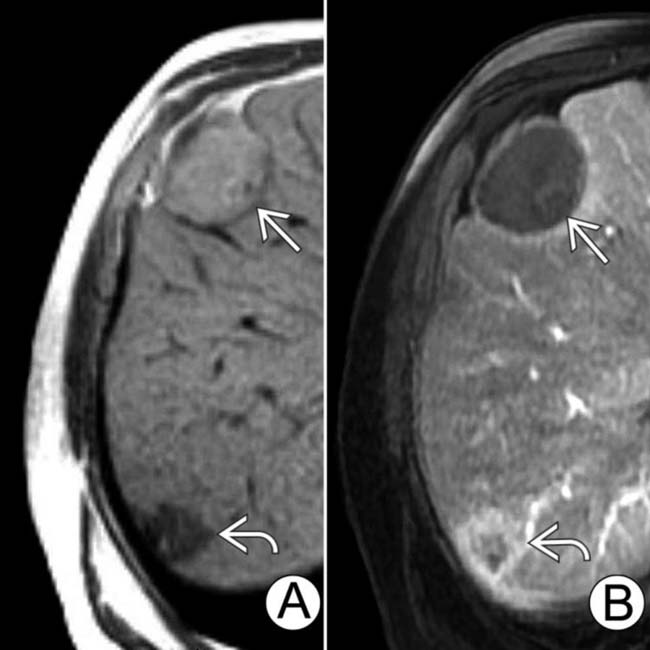
 that has typical features of a nonviable tumor, being hyperintense on T1WI, while a viable smaller tumor
that has typical features of a nonviable tumor, being hyperintense on T1WI, while a viable smaller tumor  is hypointense on T1WI. On the C+ T1WI (B) the viable lesion enhances
is hypointense on T1WI. On the C+ T1WI (B) the viable lesion enhances  , while the nonviable mass
, while the nonviable mass  does not.
does not.












































































































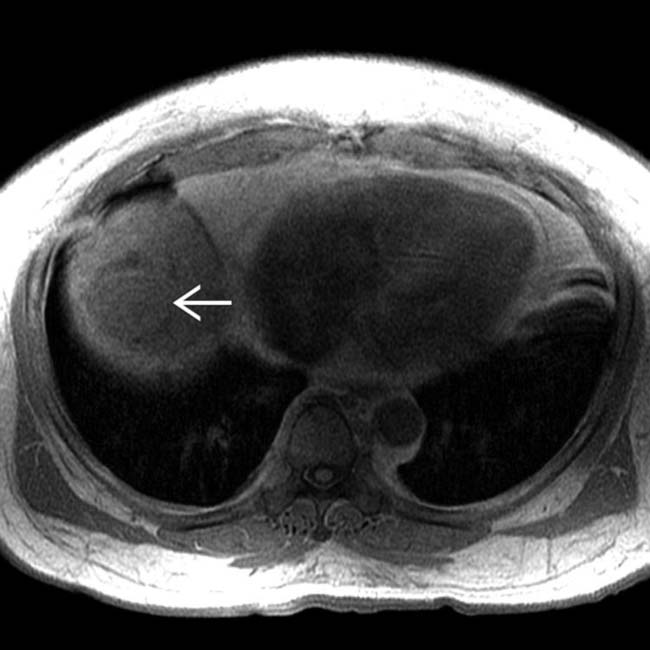
 as slightly hypointense to liver.
as slightly hypointense to liver.
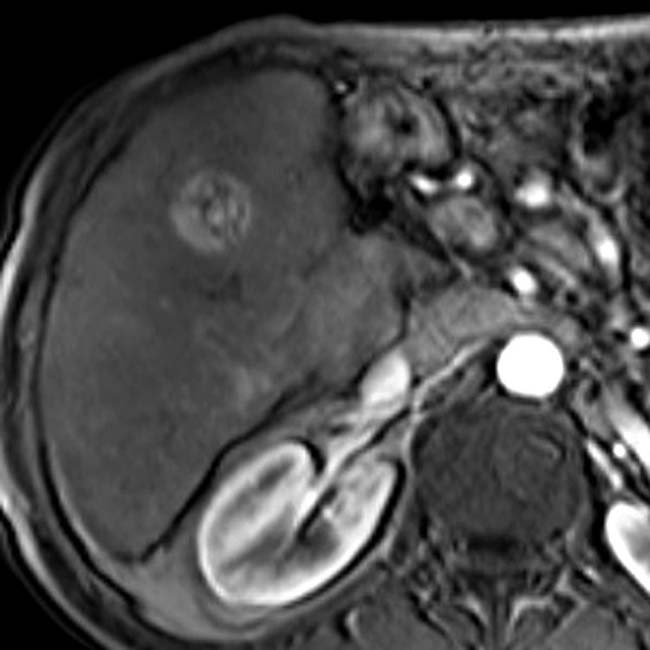

 and right hepatic vein. The liver mass had foci of fat most evident on NECT (not shown).
and right hepatic vein. The liver mass had foci of fat most evident on NECT (not shown).
 .
.

