CHAPTER 36 Hepatic Tumors
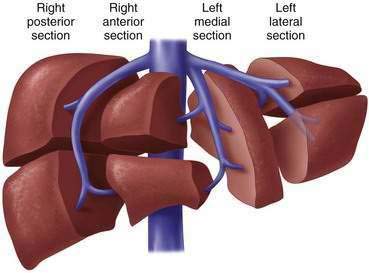
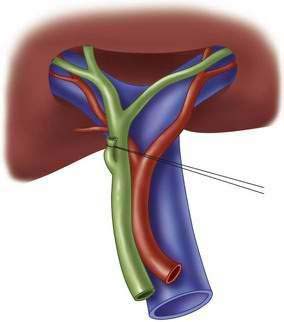
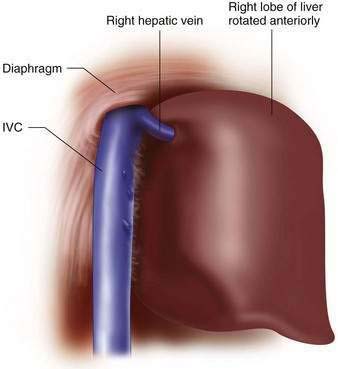
Step1: Surgical Anatomy
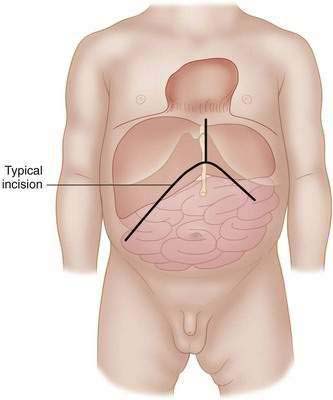
Step 2: Preoperative Considerations
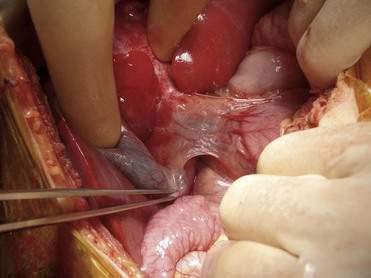
 A mechanical retractor such as a Thompson retractor (Thompson Surgical Instruments, Inc.) or a Buchwalter will simplify exposure, especially for suprahepatic vena cava and right hepatic resections.
A mechanical retractor such as a Thompson retractor (Thompson Surgical Instruments, Inc.) or a Buchwalter will simplify exposure, especially for suprahepatic vena cava and right hepatic resections. The ultrasonic dissector, water-jet dissector, electrocautery, and the argon-beam coagulator can all be useful during the parenchyma dissection. The dissectors can assist in exposure of the vessels and ducts within the substance of the liver so that these structures can be easily identified and ligated.
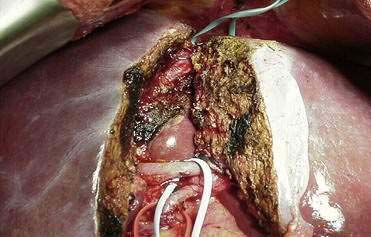
The ultrasonic dissector, water-jet dissector, electrocautery, and the argon-beam coagulator can all be useful during the parenchyma dissection. The dissectors can assist in exposure of the vessels and ducts within the substance of the liver so that these structures can be easily identified and ligated.Step 3: Operative Steps
Step 4: Postoperative Care
Step 5: Pearls and Pitfalls
Cho CS, Park J, Fong Y. Hepatic resection. In: ACS surgery: Principles and practice. WebMD; 2007.
De Ville de Goyet J, Otte J-B. Liver tumors and resections. In: Stinger MD, Oldham KT, Mouriquand PDE, editors. Pediatric surgery and urology: Long-term outcomes. 2nd ed. New York: Cambridge University Press; 2006:799-814.
Giuliante F, Nuzzo G, Ardito F, et al. Extraparenchymal control of hepatic veins during mesohepatectomy. J Am Coll Surg 206:496-502.
Gonzalez RJ, Barnett CBJr. A technique for safely teaching major hepatectomy to surgical residents. Am J Surg. 2008;195:521-525.
Poon RT. Current techniques of liver transection. HPB. 2007;9:166-173.
Poon RT. Recent advances in techniques of liver resection. Surg Technol Int. 2004;13:71-77.
Vollmer CM, Dixon E, Sahajpal A, et al. Water-jet dissection for parenchymal division during hepatectomy. HPB. 2006;8:377-385.
Yao P, Morris DL. Radiofrequency ablation-assisted liver resection: review of the literature and our experience. HPB. 2006;8:248-254.