Chapter 78 Hepatic and Biliary Disease
The pulmonary consequences of liver disorders can be classified according to whether they predominantly affect the pleural space, the lung parenchyma, or the pulmonary circulation. Unique pulmonary abnormalities occur in patients with severe alpha1-antitrypsin deficiency, primary biliary cirrhosis (PBC), and primary sclerosing cholangitis (PSC). The impact of hepatic dysfunction on the respiratory system during sleep has recently been appreciated (Table 78-1).
Table 78-1 Major Pulmonary Consequences of Portal Hypertension (with or Without Cirrhosis)
| Area/Disorder | Complications |
|---|---|
| Pleural space | |
| Pulmonary parenchyma | |
| Pulmonary circulation | |
| Sleep-disordered breathing |
HCV, hepatitis C virus; NSIP, nonspecific interstitial pneumonia; PBC, primary biliary cirrhosis; PSC, primary sclerosing cholangitis; SaO2, arterial oxygen saturation; UIP, usual interstitial pneumonia.
Pathophysiology
Hepatopulmonary Syndrome
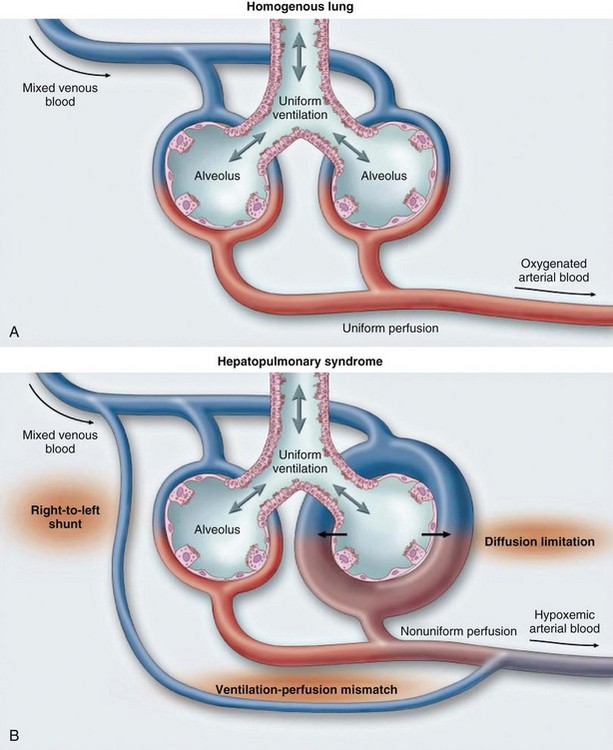
HPS is characterized by arterial hypoxemia caused by precapillary-capillary dilations or direct arteriovenous communications. Excess perfusion for a given area of ventilation, diffusion limitation, and true anatomic shunting contribute to the degree of abnormal arterial oxygenation (Figure 78-1). Increased concentrations of exhaled nitric oxide have been demonstrated in HPS. Animal models of HPS have found upregulation of endothelin B receptors causing vasodilation and evidence of angiogenesis.
Portopulmonary Hypertension
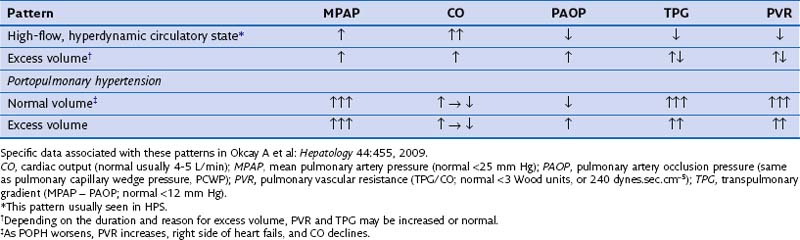
POPH results from vasoproliferation (endothelium and smooth muscle), along with in situ thrombosis, which causes an increased pulmonary vascular resistance (PVR) to arterial flow. It is important to note the various pulmonary hemodynamic patterns that may exist in the patient with advanced liver disease (Table 78-2).
Clinical Features
Diagnosis
Hepatopulmonary Syndrome
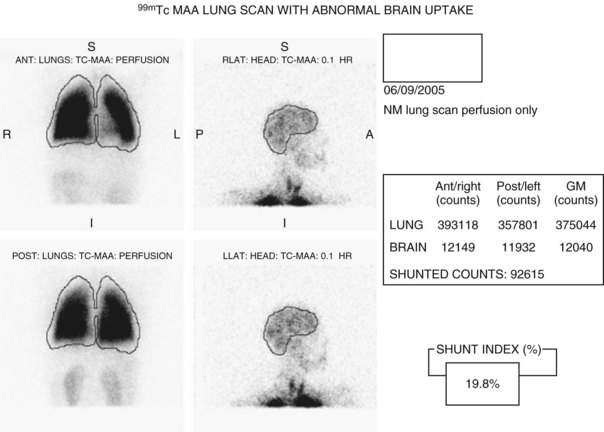
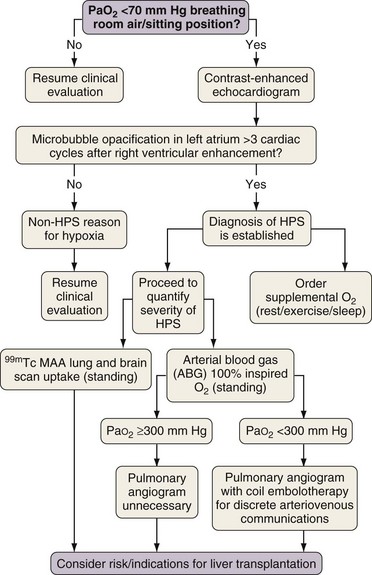
The HPS diagnosis is established by demonstrating pulmonary vascular dilation as the cause for hypoxemia. Hypoxemia is usually defined as PaO2 less than 80 mm Hg or alveolar-arterial oxygen gradient greater than 15 to 20 mm Hg. Two noninvasive methods are available to document abnormal pulmonary vascular dilation. Qualitatively, a positive contrast-enhanced transthoracic echocardiogram reflects the passage of microbubbles (usually absorbed during a first pass through normal lungs) through dilated pulmonary vessels, with subsequent detection in the left atrium. Quantitatively, an abnormal brain uptake of technetium-labeled macroaggregated albumin (99mTc MAA) (uptake > 6%) after lung perfusion reflects the passage of radiolabeled albumin aggregates through the lungs and subsequent uptake in the brain (Figure 78-2). Contrast echocardiography is more sensitive than 99mTc lung scanning to detect pulmonary vascular dilation. A lung biopsy is not necessary. Figure 78-3 provides a practical clinical algorithm for the evaluation of suspected HPS.
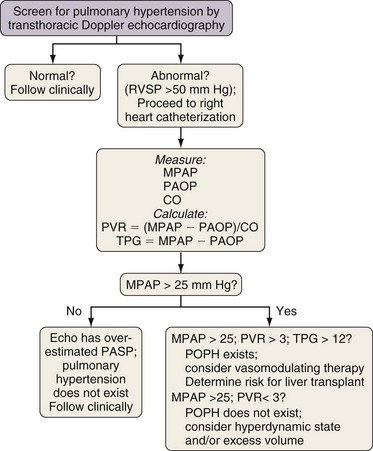
Portopulmonary Hypertension
Screening for pulmonary hypertension is accomplished by transthoracic Doppler echocardiography. Increased right ventricular systolic pressure (RVSP) greater than 50 mm Hg suggests but does not prove clinically significant POPH. A right-sided heart catheterization must be accomplished to establish the diagnosis. Figure 78-4 provides a screening algorithm used at the Mayo Clinic; clinicians may have other criteria to determine candidates for right-sided heart catheterization. Most centers adhere to the triad of mean pulmonary artery pressure (MPAP) greater than 25 mm Hg, normal pulmonary capillary wedge pressure (PCWP) less than 15 mm Hg, and increased pulmonary vascular resistance (PVR) greater than 240 dynes.sec.cm−5) as definitive criteria for POPH. A lung biopsy is neither necessary nor advised. Chronic pulmonary emboli should be excluded.
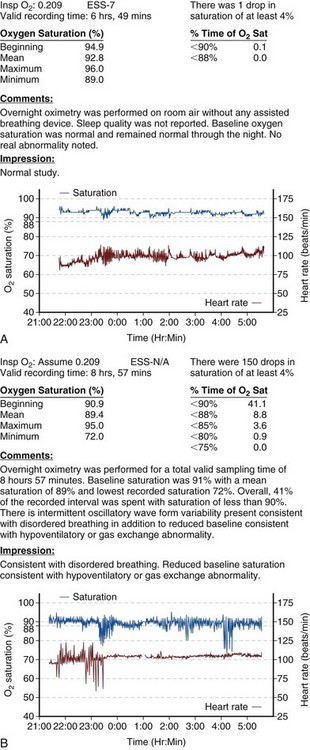
Sleep-Disordered Breathing
Overnight oximetry (OvOx) using finger pulse monitoring to screen for abnormal nocturnal oxygenation is inexpensive and clinically important. Abnormal OvOx abnormalities include frequent and severe hemoglobin desaturation (Figure 78-5). These abnormalities are common in LT candidates despite a lack of daytime somnolence. Abnormal OvOx is associated with massive ascites, encephalopathy, and increased baseline alveolar-arterial oxygen gradients. If OvOx is abnormal, formal polysomnography (PSG; overnight sleep study with multiple variable noninvasive monitoring) should be conducted. PSG is the “gold standard” to diagnose specific sleep-disordered breathing etiologies.
Treatment
Clinical Course
Hepatopulmonary Syndrome
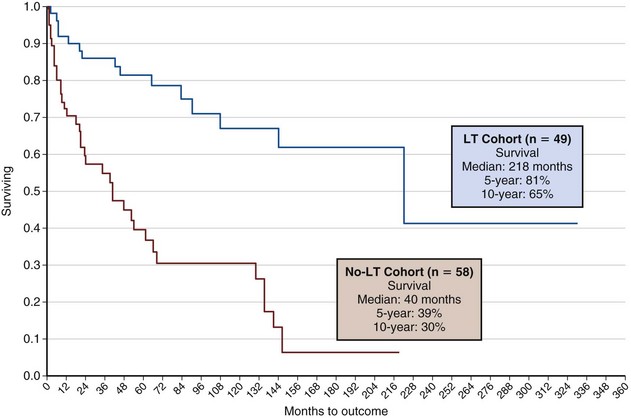
Few data exist to characterize the clinical course in HPS. In the largest series to date, 5-year survival associated with LT was 76% versus 23% in non-LT group (Figure 78-6). Complete resolution of HPS often follows LT; the time to resolution is directly related to the severity of hypoxemia and may take months. Mortality is rarely a direct consequence of hypoxemia.
Cartin-Ceba R, Swanson KL, Wiesner RH, Krowka MJ. Safety and efficacy of ambrisentan in portopulmonary hypertension. Chest. 2011;139:109–114.
Gupta S, Castel H, Rao RV, et al. Improved survival after liver transplantation in patients with hepatopulmonary syndrome. Am J Transplant. 2010;10:354–363.
Iyer V, Swanson KL, Cartin-Ceba R, Krowka MJ. Liver transplantation in hepatopulmonary syndrome: 5 and 10 year survivals. Liver Transpl. 2011;17:S130.
Kelly E, Grenne CM, Carroll TP, et al. Alpha-1 antitrypsin deficiency. Respir Med. 2010;104:763–772.
Kiafar C, Gilani N. Hepatic hydrothorax: current concepts of pathophysiology and treatment options. Ann Hepatol. 2008;7:313–320.
Krowka MJ, Miller D, Barst R, et al. Portopulmonary hypertension: results from the U.S. REVEAL registry. Chest. 2012;141:906–915.
Krowka MJ, Swanson KL, McGoon MD, et al. Portopulmonary hypertension: results of a 10-year screening algorithm. Hepatology. 2006;44:1140–1152.
Okcay A, Somers V, Caples S, Krowka MJ. Abnormal screening oximetry in liver transplant candidates (abstract). Hepatology. 2009;44:455.
Polito A. Pulmonary reactions to novel chemotherapeutic agents and biomolecules. In: Camus P, et al. Drug-induced and iatrogenic respiratory disease. London: Hodder Arnold, 2010.
Rodriguez-Roisin R, Krowka MJ. Hepatopulmonary syndrome: a liver-induced lung vascular disorder. N Engl J Med. 2008;358:2378–2387.
Singh C, Sager JS. Pulmonary complications of cirrhosis. Med Clin North Am. 2009;93:871–883.