Almost all in young women with high estrogen environment, including steatosis and oral contraceptive use

 in the right lobe of the liver. A lentiform heterogeneous collection of fluid indents the surface of the liver, and within this collection is a focus of higher density
in the right lobe of the liver. A lentiform heterogeneous collection of fluid indents the surface of the liver, and within this collection is a focus of higher density  likely representing a sentinel clot. A ruptured inflammatory hepatic adenoma was resected.
likely representing a sentinel clot. A ruptured inflammatory hepatic adenoma was resected.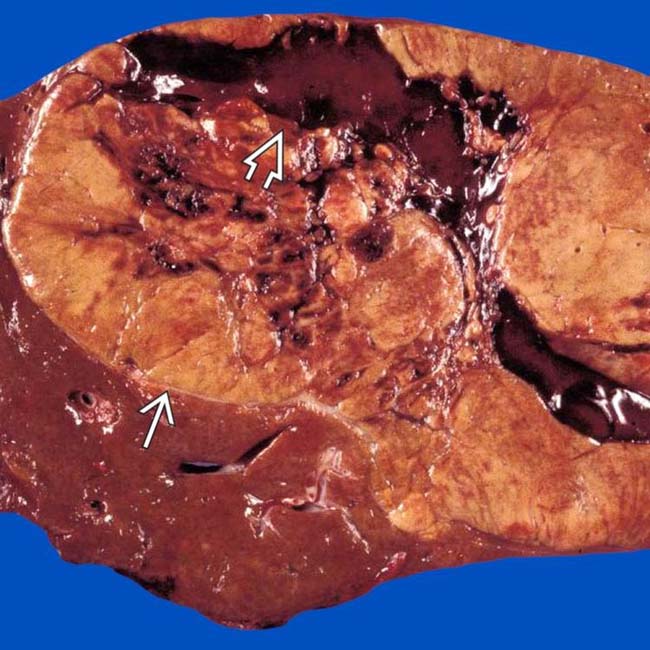
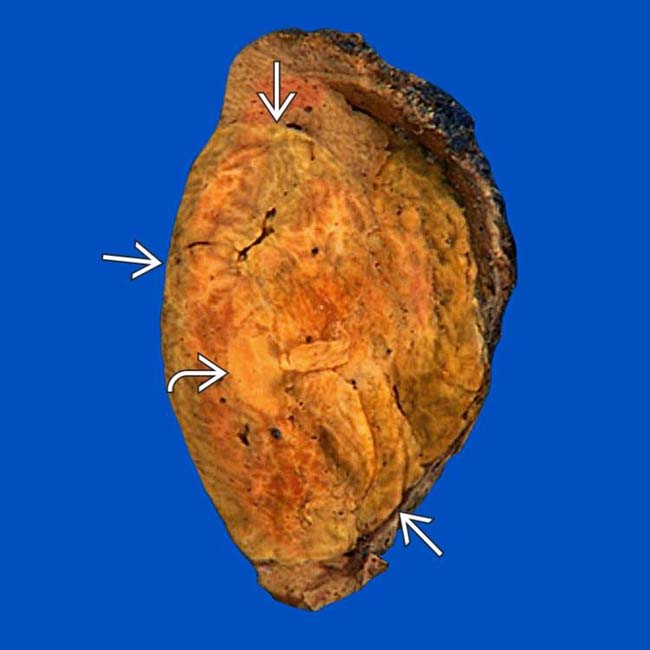
 with central areas of rupture and hemorrhage
with central areas of rupture and hemorrhage  . (Courtesy M. Yeh, MD, PhD.)
. (Courtesy M. Yeh, MD, PhD.)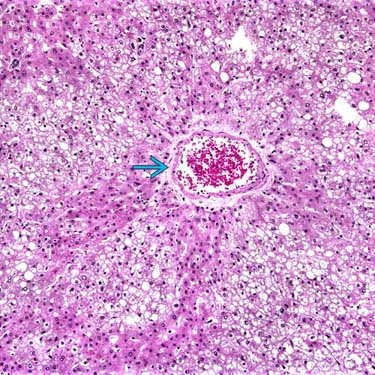
 surrounded by neoplastic hepatocytes with abundant steatosis. Imaging often reveals these features, directly or indirectly. (Courtesy M. Yeh, MD, PhD.)
surrounded by neoplastic hepatocytes with abundant steatosis. Imaging often reveals these features, directly or indirectly. (Courtesy M. Yeh, MD, PhD.)PATHOLOGY
General Features
Staging, Grading, & Classification
• 3 distinct subtypes
 Inflammatory HA
Inflammatory HA
 Inflammatory HA
Inflammatory HA

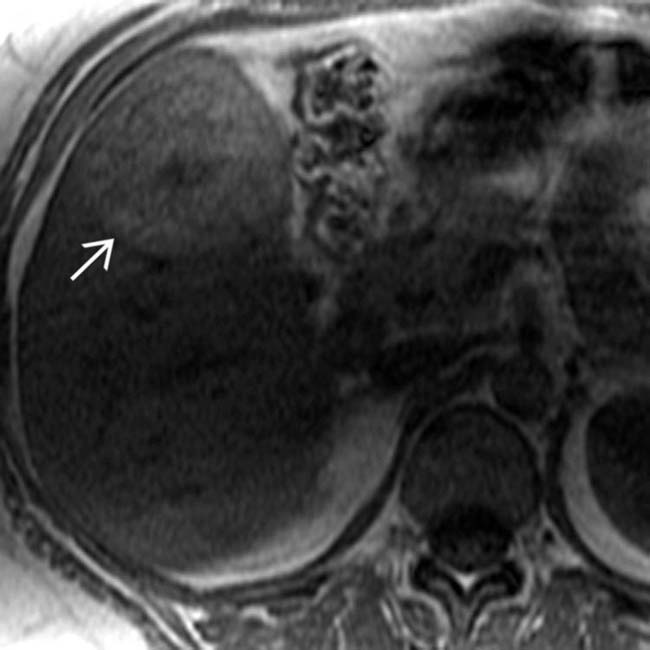
 that is not very vascular, a typical (but not diagnostic) feature of the HNF1A-mutated subtype of hepatic adenoma.
that is not very vascular, a typical (but not diagnostic) feature of the HNF1A-mutated subtype of hepatic adenoma.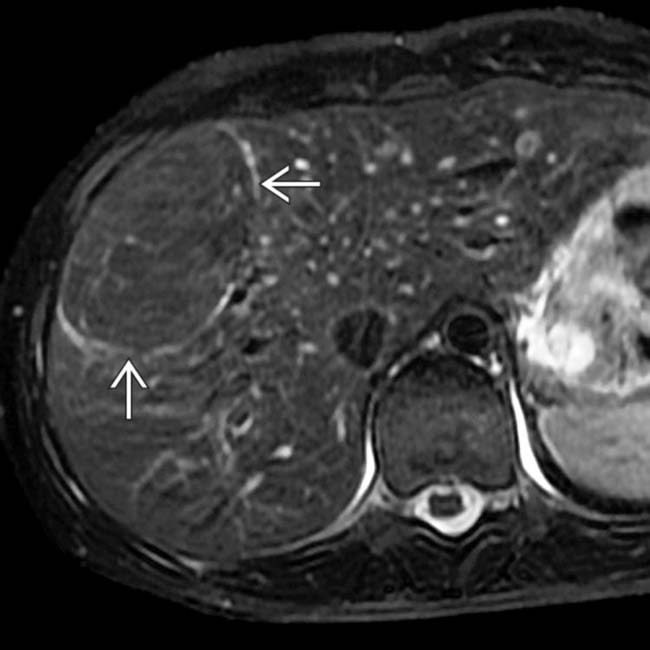
 , typical features of an HNF1A-mutated subtype of hepatic adenoma.
, typical features of an HNF1A-mutated subtype of hepatic adenoma.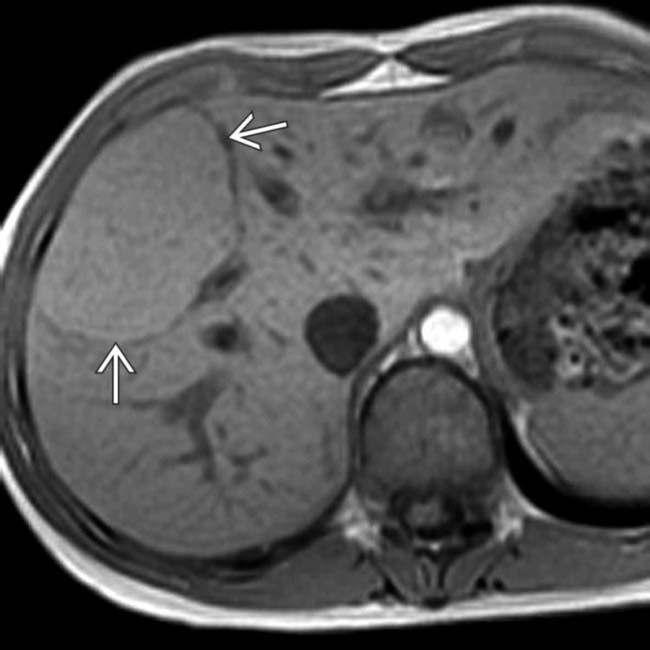
 .
.
 , which indicates the presence of diffuse lipid, another typical feature of this subtype of hepatic adenoma.
, which indicates the presence of diffuse lipid, another typical feature of this subtype of hepatic adenoma.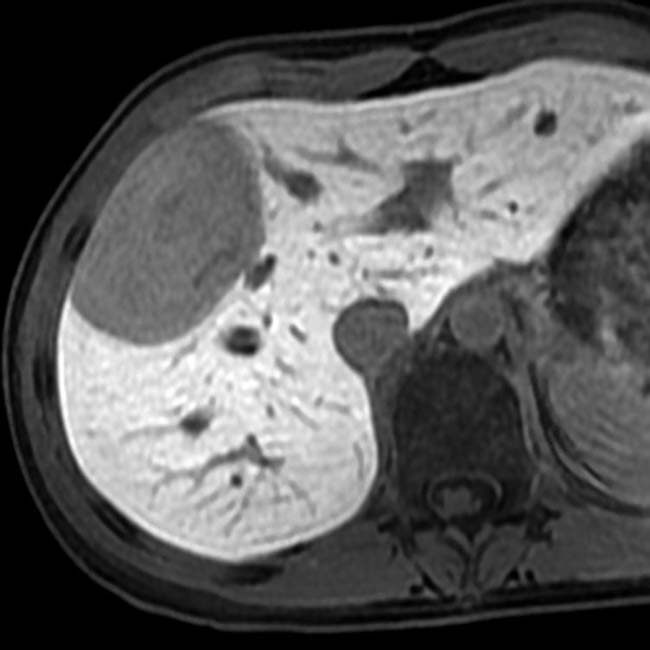
 with diffuse and focal lipid
with diffuse and focal lipid  .
.
 as slightly hyperintense to a normal-appearing liver. On opposed-phase GRE MR (not shown), there was no signal dropout from the lesion, indicating no lipid content.
as slightly hyperintense to a normal-appearing liver. On opposed-phase GRE MR (not shown), there was no signal dropout from the lesion, indicating no lipid content.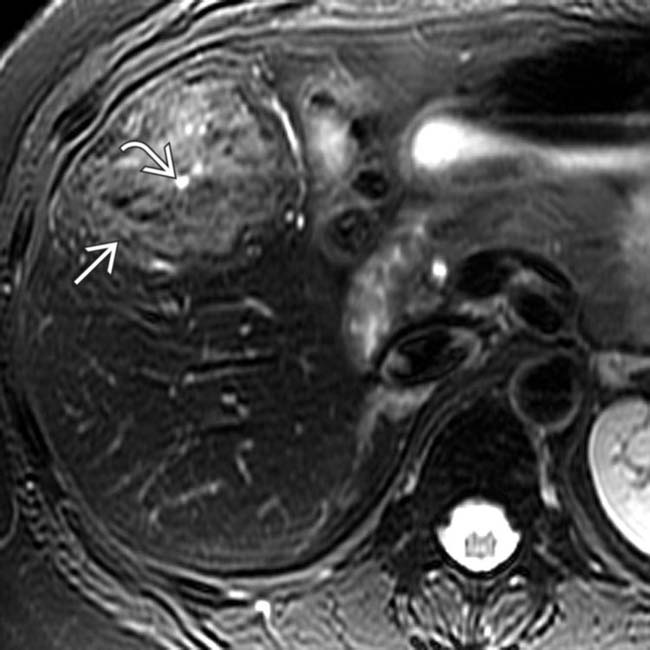
 is slightly hyperintense to the liver, and a central scar
is slightly hyperintense to the liver, and a central scar  is quite hyperintense.
is quite hyperintense.
 whereas the central scar is hypointense
whereas the central scar is hypointense  . The mass and central scar were nearly isointense on the venous phase images (not shown).
. The mass and central scar were nearly isointense on the venous phase images (not shown).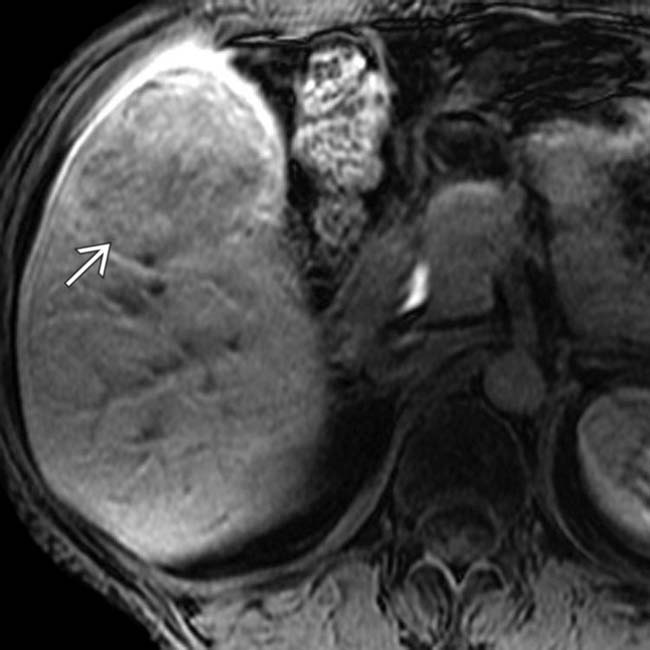
 retains less contrast material than normal liver. Because there was concern that the lesion was not a typical FNH, it was resected.
retains less contrast material than normal liver. Because there was concern that the lesion was not a typical FNH, it was resected.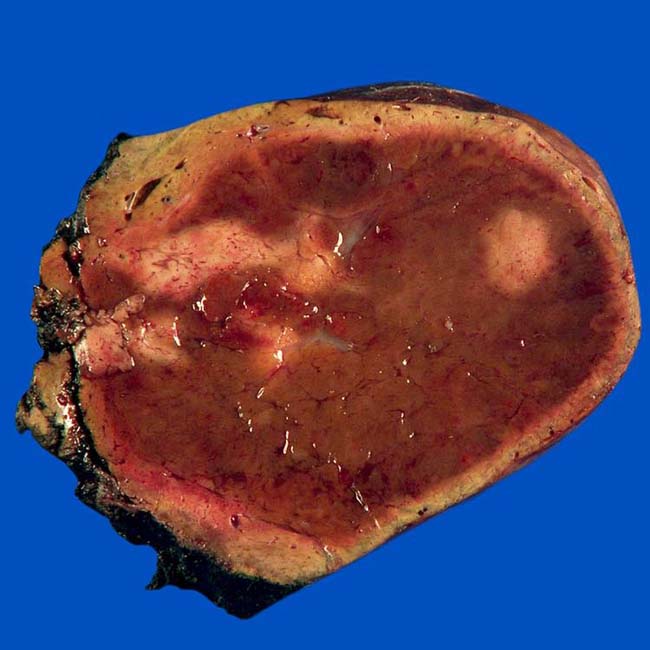
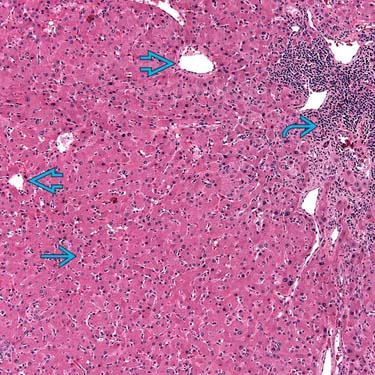
 with abundant eosinophilic nuclei on H&E staining, unpaired blood vessels
with abundant eosinophilic nuclei on H&E staining, unpaired blood vessels  distributed haphazardly throughout the lesion, and foci of chronic inflammation
distributed haphazardly throughout the lesion, and foci of chronic inflammation  . The final diagnosis was hepatic adenoma of the inflammatory subtype. (Courtesy T. Longacre, MD.)
. The final diagnosis was hepatic adenoma of the inflammatory subtype. (Courtesy T. Longacre, MD.)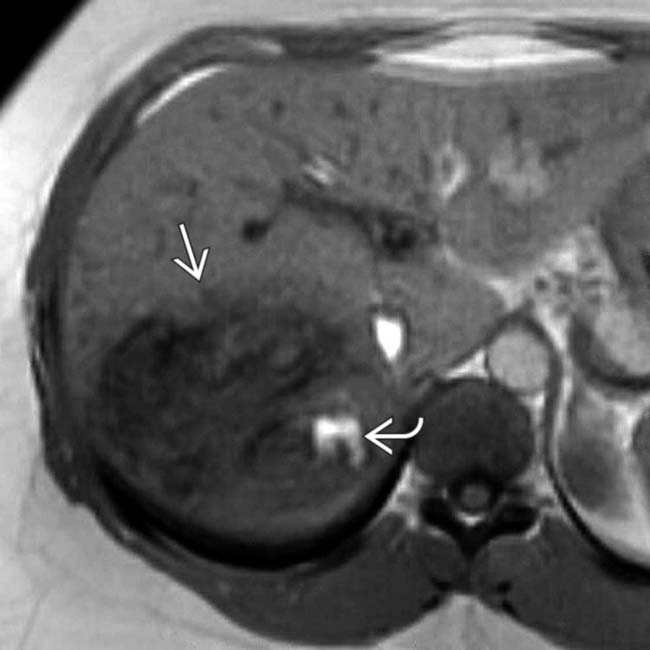
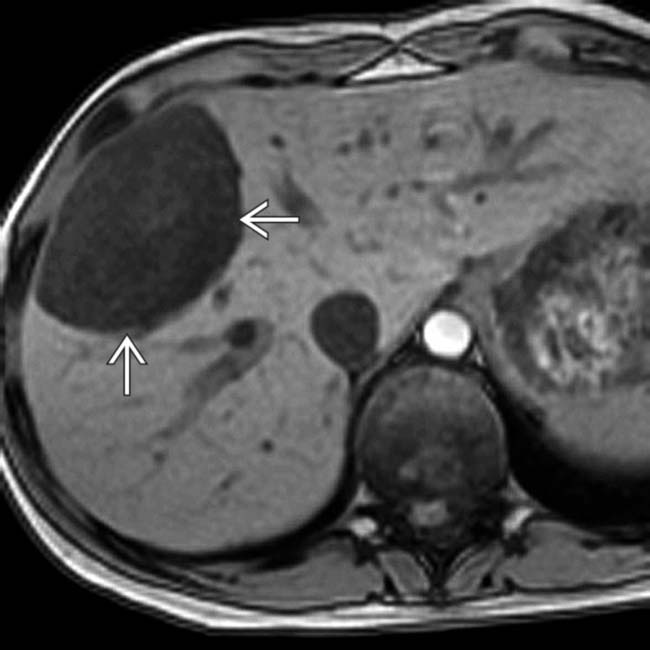
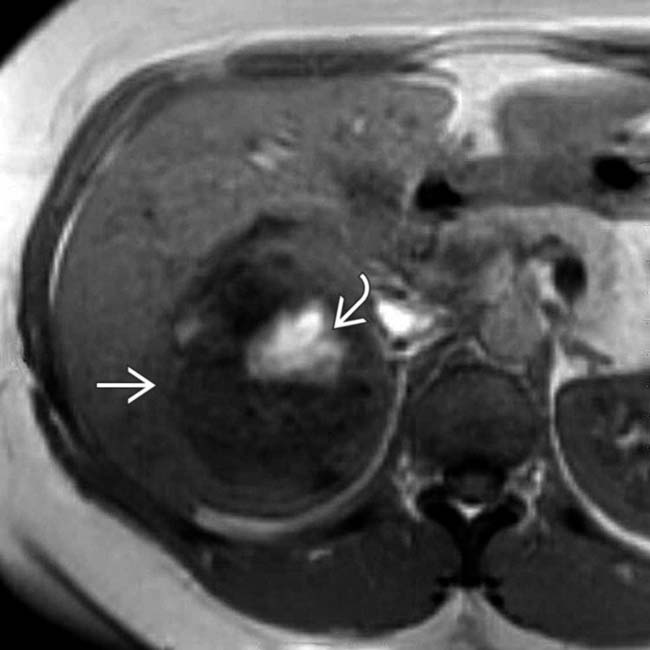
 containing several hyperintense foci
containing several hyperintense foci  that represent hemorrhage.
that represent hemorrhage.
 that represent lipid.
that represent lipid.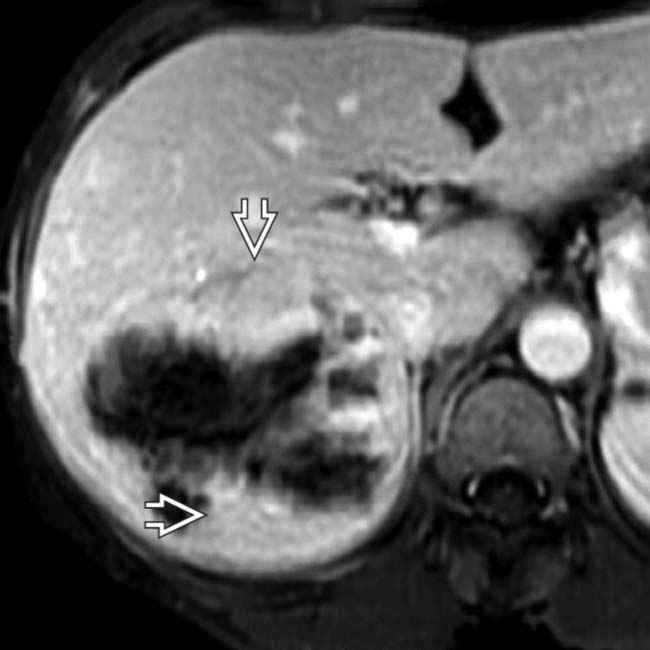
 in the nonnecrotic and nonhemorrhagic portions of the mass, typical features of the inflammatory subtype of hepatic adenoma, which was confirmed on resection.
in the nonnecrotic and nonhemorrhagic portions of the mass, typical features of the inflammatory subtype of hepatic adenoma, which was confirmed on resection.
 .
.
 . Hepatic adenomas of the inflammatory subtype are usually heterogeneously hypervascular and often encapsulated with focal hemorrhage, as in this patient.
. Hepatic adenomas of the inflammatory subtype are usually heterogeneously hypervascular and often encapsulated with focal hemorrhage, as in this patient.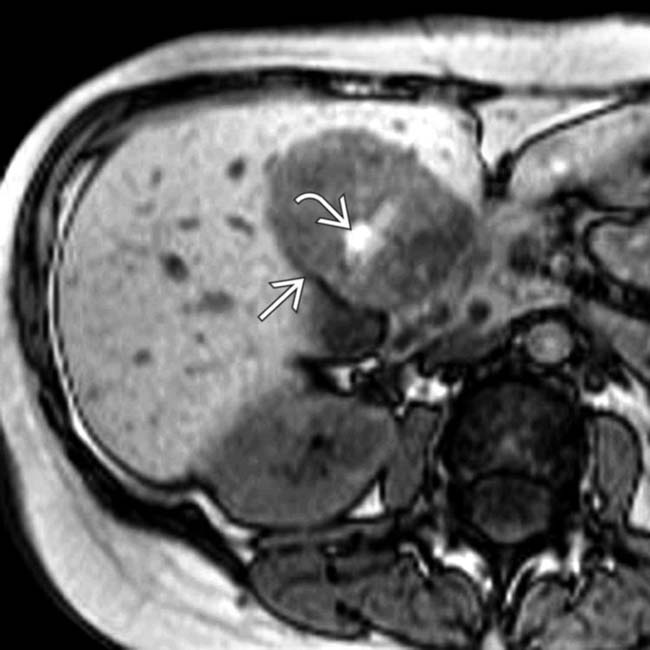
 with hyperintense foci
with hyperintense foci  representing hemorrhage or fat. The in-phase images showed increased signal within the mass.
representing hemorrhage or fat. The in-phase images showed increased signal within the mass.
 (hemorrhage). Fat content would have shown signal dropout on this sequence. A capsule or pseudocapsule is seen in ∼ 20% of adenomas.
(hemorrhage). Fat content would have shown signal dropout on this sequence. A capsule or pseudocapsule is seen in ∼ 20% of adenomas.
 with a focal calcification
with a focal calcification  , the latter being a less common feature of adenomas.
, the latter being a less common feature of adenomas.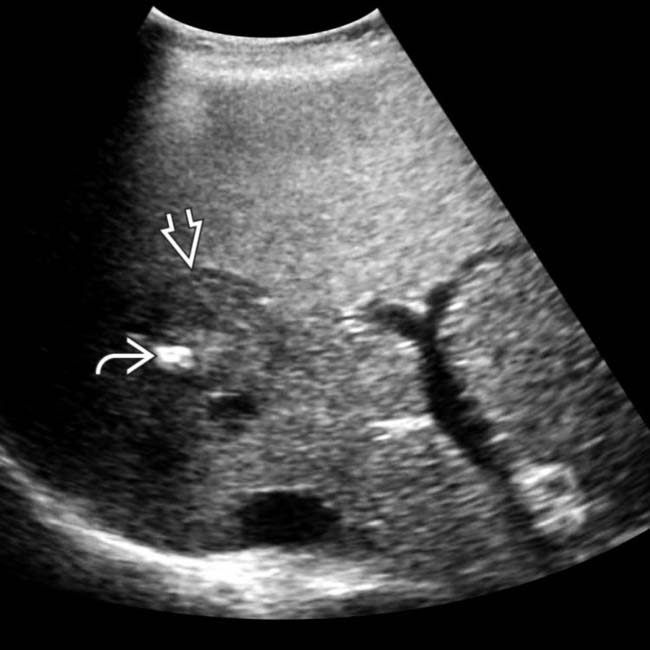
 and shows a capsule
and shows a capsule  around the mass. The capsule is a common feature and the focal calcification a less common feature of adenomas, as was proven in this case.
around the mass. The capsule is a common feature and the focal calcification a less common feature of adenomas, as was proven in this case.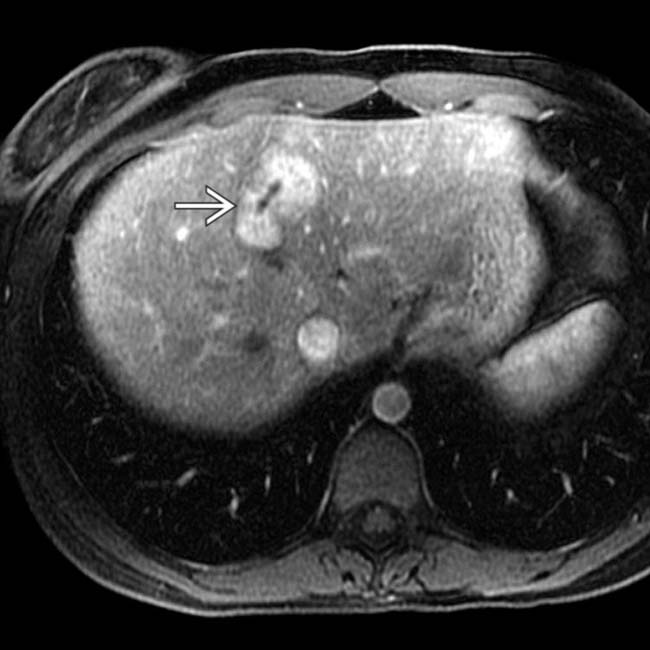
 .
.
 are seen on this section. In the absence of chronic liver disease or a known malignancy, these findings were considered diagnostic of adenomas. Following cessation of oral contraceptive use, these adenomas decreased in size and number within 4 months.
are seen on this section. In the absence of chronic liver disease or a known malignancy, these findings were considered diagnostic of adenomas. Following cessation of oral contraceptive use, these adenomas decreased in size and number within 4 months.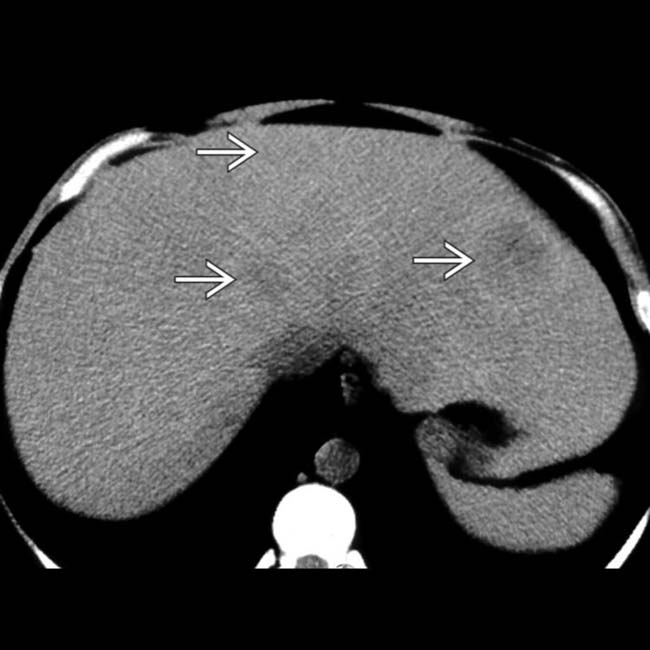
 within the liver. The low attenuation is due to intratumoral lipid. These are foci of the CTNNB1-mutated subtype of hepatic adenoma.
within the liver. The low attenuation is due to intratumoral lipid. These are foci of the CTNNB1-mutated subtype of hepatic adenoma.
 whereas others show heterogeneous enhancement
whereas others show heterogeneous enhancement  .
.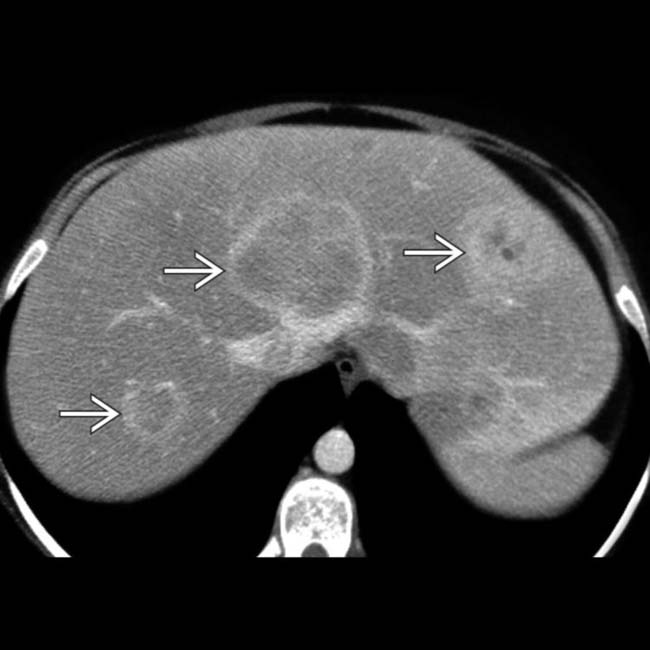
 . Adenomas are usually multiple in the setting of type I or III glycogen storage disease and carry a high risk of malignant degeneration, especially those > 5 cm in diameter and those in men.
. Adenomas are usually multiple in the setting of type I or III glycogen storage disease and carry a high risk of malignant degeneration, especially those > 5 cm in diameter and those in men.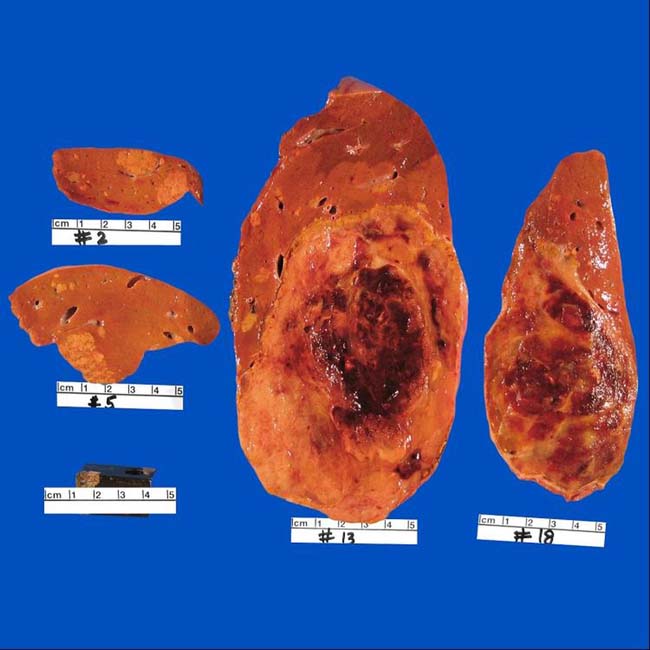









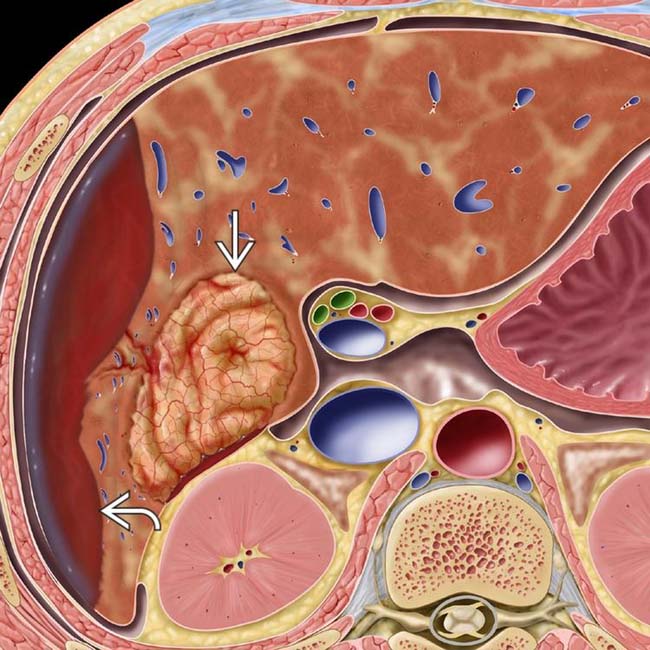
 in the right lobe and spontaneous subcapsular bleeding
in the right lobe and spontaneous subcapsular bleeding  .
.














































































 of hemorrhage within the hypointense mass
of hemorrhage within the hypointense mass  .
.
 measuring less than water attenuation, indicating fat content. Also noted are foci of calcification
measuring less than water attenuation, indicating fat content. Also noted are foci of calcification  . Serial CT scans had shown slow growth of the mass over 7 years.
. Serial CT scans had shown slow growth of the mass over 7 years.
 and hemorrhage
and hemorrhage  . Histology revealed foci of HCC within this adenoma, which had the CTNNB1 mutation, as did the foci of HCC.
. Histology revealed foci of HCC within this adenoma, which had the CTNNB1 mutation, as did the foci of HCC.


