Chapter 20 Hemoptysis
Differential Diagnosis
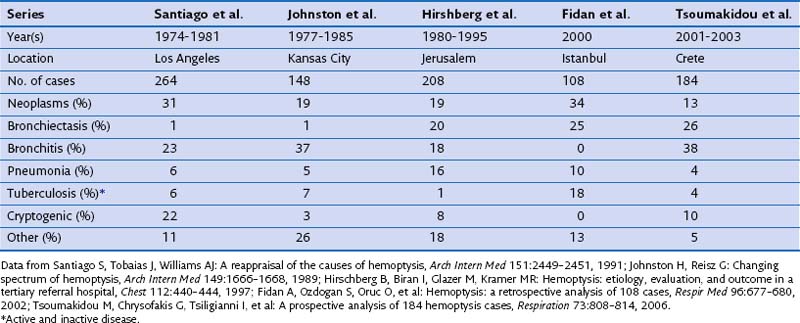
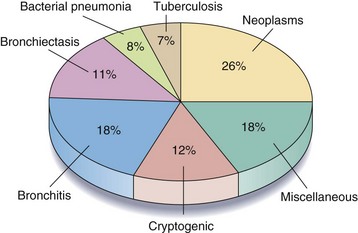
A large number of disorders have been reported to cause hemoptysis, and the most important are listed in Box 20-1. Of these, bronchogenic carcinoma, bronchiectasis, bronchitis, and bacterial pneumonia are responsible for most cases. Table 20-1 shows the relative frequency of disorders causing hemoptysis in major series published since 1980. The significant variability, especially in the frequency of bronchiectasis, bronchitis, and tuberculosis, probably reflects differences in the time of publication, the patient population studied, and the diagnostic tests and criteria used. Figure 20-1 illustrates the percentage of patients with each diagnosis on the basis of pooled data from these studies.
Box 20-1
Causes of Hemoptysis
Cryptogenic Hemoptysis
In almost all reported series, the cause of hemoptysis remains unknown in a significant percentage of patients. As shown in Table 20-1, the frequency of cryptogenic hemoptysis has varied widely, and this variability presumably is due to differences in diagnostic criteria and the extent of evaluation.
Patient Evaluation
Initial Evaluation
Important symptoms, signs, and historical details that suggest one or more disorders are listed in Table 20-2. In some patients, such as those with pulmonary embolism, left ventricular failure, mitral stenosis, and traumatic or iatrogenic lung injury, the history and physical examination may provide the most important clues to the diagnosis.
Table 20-2 Important Clinical Features in Patients with Hemoptysis
| Category | Feature(s) | Disorder(s) |
|---|---|---|
| Historical |
As shown in Table 20-3, the chest radiograph also may yield important information about the underlying cause of hemoptysis. The chest film, however, is “localizing”—that is, it demonstrates a mass, cavity, infiltrate, lobar atelectasis, or other finding that is likely to be directly related to the cause of hemoptysis—in less than 40% of patients. In the remainder, the chest radiograph is either normal in appearance or demonstrates abnormal but nonspecific findings such as emphysema, interstitial fibrosis, minor atelectasis, or pleural thickening—a category referred to as “nonlocalizing.” This radiographic classification has important diagnostic and prognostic implications. Malignancy is found in almost 40% of patients with hemoptysis associated with localizing findings on the chest radiograph. On the other hand, cancer is diagnosed in only 6% to 10% of patients with normal-appearing or nonlocalizing chest radiographs.
Table 20-3 Important Radiographic Findings in Patients with Hemoptysis
| Radiographic Finding | Associated Disorder(s) |
|---|---|
| Nodule(s) or mass(es) | Bronchogenic carcinoma or other neoplasm, lung abscess, fungal infection, vasculitis |
| Atelectasis | Bronchogenic carcinoma or other endobronchial neoplasm, broncholithiasis, foreign body |
| Hilar/mediastinal adenopathy | Bronchogenic carcinoma or other neoplasm, mycobacterial or fungal infection, sarcoidosis |
| Dilated peripheral airways | Bronchiectasis |
| Air space consolidation | Pneumonia, alveolar hemorrhage, pulmonary contusion |
| Reticulonodular densities | Sarcoidosis, lymphangitic carcinoma |
| Cavity—single or multiple | Mycobacterial or fungal infection, mycetoma, lung abscess, bronchogenic carcinoma |
| Hilar/mediastinal calcification | Previous mycobacterial or fungal infection, broncholithiasis |
Computed Tomography
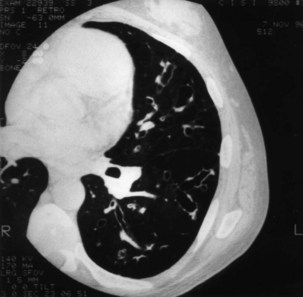
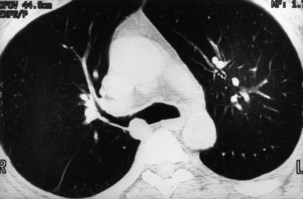
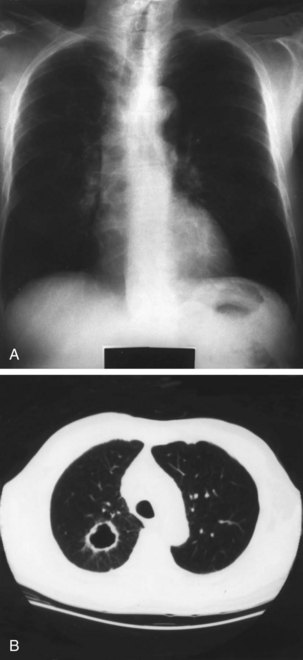
Compared with conventional chest radiography, CT is clearly superior for imaging the peripheral and central airways, mediastinum, and lung parenchyma. Thus, it is not surprising that CT has been shown to be very useful in the evaluation of patients with hemoptysis. In the presence of a normal-appearing or nonlocalizing chest radiograph, CT reveals an unsuspected cause of hemoptysis, most commonly bronchiectasis, in approximately one third of patients (Figure 20-2). CT also may demonstrate an endobronchial lesion (Figure 20-3) or an unsuspected parenchymal mass, nodule, or cavity (Figure 20-4). CT also is useful in more than half of all patients whose chest radiograph is localizing, either by revealing a new source of hemoptysis or by providing additional information about a previously recognized abnormality.
Fiberoptic Bronchoscopy
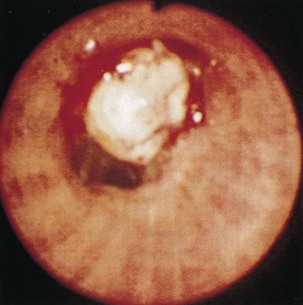
Since becoming widely available in the early 1970s, fiberoptic bronchoscopy (FOB) has been used almost routinely in the evaluation of patients with hemoptysis. By combining endoscopic examination with brushings, washings, endobronchial and transbronchial biopsy techniques, and transtracheal needle aspiration, FOB may be used both to identify the site of bleeding and to obtain a definitive diagnosis. FOB is most useful for diagnosing bronchogenic carcinoma and other endobronchial neoplasms (Figure 20-5); it is far less effective at detecting other causes of hemoptysis. The most common non-neoplastic diagnosis made by FOB is acute bronchitis, which is based on the presence of mucosal hyperemia and edema and purulent-appearing secretions. As previously discussed, however, these findings are nonspecific and often are unrelated to the actual cause of hemoptysis. When this diagnosis is excluded, a specific, non-neoplastic cause of hemoptysis is found by FOB in less than 10% of cases.
Diagnostic Algorithm
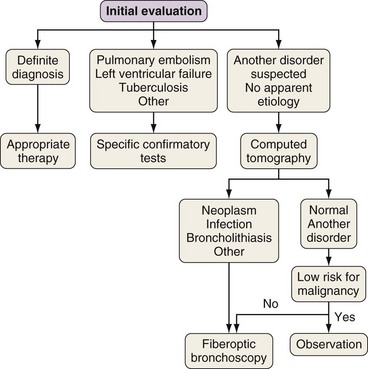
A suggested approach to the patient with hemoptysis that is based on the preceding information is shown in Figure 20-6. If the initial evaluation yields a firm diagnosis, such as bacterial pneumonia or iatrogenic or traumatic lung injury, appropriate therapy is instituted. Alternatively, the initial evaluation may suggest a cause of hemoptysis that requires investigation using one or more specific tests. For example, an echocardiogram may confirm the presence of left ventricular failure or mitral stenosis, pulmonary embolism may be diagnosed by means of a CT angiogram, and sputum cultures may be diagnostic in patients with tuberculosis. In all other patients, CT is the most appropriate next step in the diagnostic evaluation. As discussed previously, CT often identifies an unsuspected cause of hemoptysis, even in patients whose chest radiograph is normal in appearance or nonlocalizing, and may provide important information in patients who already have a presumptive diagnosis. For example, in patients with suspected bronchogenic carcinoma, CT adds vital information for staging and also provides a “road map” for bronchoscopy by defining the exact location of a parenchymal mass and enlarged mediastinal lymph nodes.
Massive Hemoptysis
Massive hemoptysis is relatively uncommon and occurs in fewer than 5% of patients with lower respiratory tract bleeding. Although any of the disorders listed in Box 20-1 may potentially give rise to life-threatening hemorrhage, massive hemoptysis most commonly is caused by bronchiectasis, bronchogenic carcinoma, mycetoma, lung abscess, and tuberculosis (active or inactive). Overall, the risk of death from massive hemoptysis is approximately 20%, although reported mortality rates vary widely, ranging between 0 and 75%.
Once bleeding has resolved, either spontaneously or after embolization therapy, its cause, if not already identified, must be determined (see Figure 20-6). Specific treatment, such as antibacterial or antituberculosis therapy, often prevents further episodes of hemoptysis. When effective therapy is not available, recurrent and often life-threatening hemorrhage occurs with a frequency as high as 50%. Recurrent bleeding is especially likely in patients with bronchiectasis, a mycetoma, or pulmonary malignancy, and surgical resection should be considered in these cases. For patients who are not surgical candidates, repeat embolization therapy often is successful if bleeding recurs.
Chun JY, Morgan R, Belli AM. Radiological management of hemoptysis: a comprehensive review of diagnostic imaging and bronchial arterial embolization. Cardiovasc Intervent Radiol. 2010;33:240–250.
Khalil A, Fartoukh M, Parrot A, et al. Impact of MDCT angiography on the management of patients with hemoptysis. AJR Am J Roentgenol. 2010;195:772–778.
Lee KS, Boiselle PM. Update on multidetector computed tomography imaging of the airways. J Thorac Imaging. 2010;25:112–124.
Thirumaran M, Sundar R, Sutcliffe IM, et al. Is investigation of patients with haemoptysis and normal chest radiograph justified? Thorax. 2009;64:854–856.
Tsoumakidou M, Chrysofakis G, Tsiligianni I, et al. A prospective analysis of 184 hemoptysis cases—diagnostic impact of chest x-ray, computed tomography, bronchoscopy. Respiration. 2006;73:808–814.