Chapter 25 Hemoptysis
1 What is hemoptysis?
 Scant hemoptysis refers to expectoration of sputa that are tinged or streaked with blood.
Scant hemoptysis refers to expectoration of sputa that are tinged or streaked with blood.
 Frank hemoptysis is characterized by sputa that are grossly bloody but of a low volume (less than 100-200 mL in 24 hours).
Frank hemoptysis is characterized by sputa that are grossly bloody but of a low volume (less than 100-200 mL in 24 hours).
 Massive hemoptysis refers to bleeding that is potentially acutely life threatening. It is inconsistently defined but generally describes expectoration of at least 200 mL of blood within a 24-hour period. Most authors limit the definition of massive hemoptysis to expectoration of more than 600 mL of blood in 24 hours.
Massive hemoptysis refers to bleeding that is potentially acutely life threatening. It is inconsistently defined but generally describes expectoration of at least 200 mL of blood within a 24-hour period. Most authors limit the definition of massive hemoptysis to expectoration of more than 600 mL of blood in 24 hours.
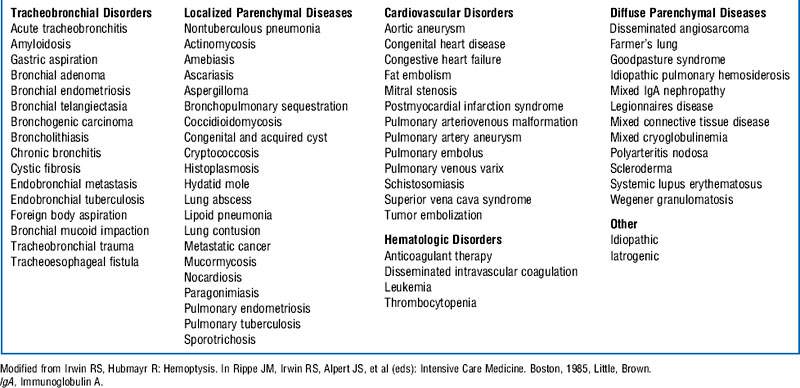
3 Describe the differential diagnosis of hemoptysis
The differential diagnosis of hemoptysis is based on the site of bleeding. Hemoptysis in general results from either a focal or a diffuse tracheobronchial (airway) or pulmonary parenchymal process (Box 25-1). Occasionally nonpulmonary processes, in particular cardiac, vascular, or hematologic disorders, may result in bleeding in the lungs. The frequency with which hemoptysis is associated with these conditions is determined by the age of the patient, the population being studied (e.g., surgical vs. medical, veterans hospital vs. city or county indigent hospital), and the amount of expectorated blood. Approximately 30% of cases are cryptogenic, and no explanation for hemoptysis is determined despite extensive evaluation.
8 What is the initial approach to the evaluation of a patient with hemoptysis in the intensive care unit?
11 Describe the immediate management of massive hemoptysis
The goals of immediate management of patients with massive hemoptysis are as follows:
12 What specific therapies may be useful to stop ongoing hemorrhage?
 Balloon tamponade with a Fogarty catheter placed under bronchoscopic guidance
Balloon tamponade with a Fogarty catheter placed under bronchoscopic guidance
 Bronchoscopy-guided topical hemostatic tamponade therapy with use of either oxidized regenerated cellulose mesh or infusions of thrombin alone or fibrinogen with thrombin
Bronchoscopy-guided topical hemostatic tamponade therapy with use of either oxidized regenerated cellulose mesh or infusions of thrombin alone or fibrinogen with thrombin
 Iced normal saline lavage of hemorrhaging lung segments
Iced normal saline lavage of hemorrhaging lung segments
 Regional instillation of vasoconstrictor agents such as epinephrine
Regional instillation of vasoconstrictor agents such as epinephrine
 If a focal airway lesion is the source of bleeding, electrocautery, laser photocoagulation, and cryotherapy
If a focal airway lesion is the source of bleeding, electrocautery, laser photocoagulation, and cryotherapy
Controversy
18 Should fiberoptic bronchoscopy be performed before bronchial artery embolization in patients with massive hemoptysis?
 Is important in guiding bronchial artery embolization by identifying the site of bleeding
Is important in guiding bronchial artery embolization by identifying the site of bleeding
 Is complementary to chest computed tomography in identifying the cause of hemoptysis, allowing the institution of specific therapy aimed at the underlying lung pathologic condition
Is complementary to chest computed tomography in identifying the cause of hemoptysis, allowing the institution of specific therapy aimed at the underlying lung pathologic condition
 Facilitates the use of a number of techniques that can control bleeding
Facilitates the use of a number of techniques that can control bleeding
 A study of 29 patients who underwent bronchial artery embolization to control massive hemoptysis revealed that the site of bleeding could be identified in 80% of patients by chest radiograph alone. Bronchoscopy was essential to localizing the site of hemorrhage in only 10% of patients.
A study of 29 patients who underwent bronchial artery embolization to control massive hemoptysis revealed that the site of bleeding could be identified in 80% of patients by chest radiograph alone. Bronchoscopy was essential to localizing the site of hemorrhage in only 10% of patients.
 The site of embolization is generally identified by angiography at the time of bronchial catheterization.
The site of embolization is generally identified by angiography at the time of bronchial catheterization.
 Emergent bronchoscopy results in unnecessary delays before performance of bronchial artery embolization.
Emergent bronchoscopy results in unnecessary delays before performance of bronchial artery embolization.
 Endobronchial tamponade is inferior to embolization as a temporary measure to control hemorrhage before the institution of more specific therapy and should be reserved for patients with contraindications to embolization.
Endobronchial tamponade is inferior to embolization as a temporary measure to control hemorrhage before the institution of more specific therapy and should be reserved for patients with contraindications to embolization.
1 Bussières J.S. Iatrogenic pulmonary artery rupture. Curr Opin Anaesthesiol. 2007;20:48–52.
2 Chun J.Y., Morgan R., Belli A.M. Radiological management of hemoptysis: a comprehensive review of diagnostic imaging and bronchial arterial embolization. Cardiovasc Intervent Radiol. 2010;33:240–250.
3 Hsiao E.I., Kirsch C.M., Kagawaa F.T., et al. Utility of fiberoptic bronchoscopy before bronchial artery embolization for massive hemoptysis. Am J Roentgenol. 2001;177:861–867.
4 Ibrahim W.H. Massive haemoptysis: the definition should be revised. Eur Respir J. 2008;32:1131–1132.
5 Jean-Baptiste E. Clinical assessment and management of massive hemoptysis. Crit Care Med. 2000;28:1642–1647.
6 Johnson J.L. Manifestations of hemoptysis: how to manage minor, moderate, and massive bleeding. Postgrad Med. 2002;112:101–113.
7 Jougon J., Ballester M., Delcambre F., et al. Massive hemoptysis: what place for medical and surgical treatment. Eur J Cardiothorac Surg. 2002;22:345–351.
8 Kalva S.P. Bronchial artery embolization. Tech Vasc Interv Radiol. 2009;12:130–138.
9 Lordan J.L., Gascoigne A., Corris P.A. The pulmonary physician in critical care: illustrative case 7: assessment and management of massive haemoptysis. Thorax. 2003;58:814–819.
10 Menchini L., Remy-Jardin M., Faivre J.B., et al. Cryptogenic haemoptysis in smokers: angiography and results of embolisation in 35 patients. Eur Respir J. 2009;34:1031–1039.
11 Praveen C.V., Martin A. A rare case of fatal haemorrhage after tracheostomy. Ann R Coll Surg Engl. 2007;89(8):1–3.
12 Sakr L., Dutau H. Massive hemoptysis: an update on the role of bronchoscopy in diagnosis and management. Respiration. 2010;80:38–58.
13 Savale L., Parrot A., Khalil A., et al. Cryptogenic hemoptysis: from a benign to a life-threatening pathologic vascular condition. Am J Respir Crit Care Med. 2007;175:1181–1185.
14 Shigemura N., Wan I.Y., Yu S.C., et al. Multidisciplinary management of life-threatening massive hemoptysis: a 10-year experience. Ann Thorac Surg. 2009;87:849–853.
15 Valipour A., Kreuzer A., Koller H., et al. Bronchoscopy-guided topical hemostatic tamponade therapy for the management of life-threatening hemoptysis. Chest. 2005;127:2113–2118.
16 Wang G.R., Ensor J.E., Gupta S., et al. Bronchial artery embolization for the management of hemoptysis in oncology patients: utility and prognostic factors. Vasc Interv Radiol. 2009;20:722–729.
17 Yoon W., Kim J.K., Kim Y.H., et al. Bronchial and nonbronchial systemic artery embolization for lifethreatening hemoptysis: a comprehensive review. Radiographics. 2002;22:1395–1409.