Chapter 458 Hemolytic Anemias Resulting from Extracellular Factors—Immune Hemolytic Anemias
Autoimmune Hemolytic Anemias
A number of extrinsic agents and disorders may lead to premature destruction of red blood cells (RBCs) (Table 458-1). Among the most clearly defined are antibodies associated with immune hemolytic anemias. The hallmark of this group of diseases is the positive result of the direct antiglobulin (Coombs) test, which detects a coating of immunoglobulin or components of complement on the RBC surface. The most important immune hemolytic disorder in pediatric practice is hemolytic disease of the newborn (erythroblastosis fetalis), caused by transplacental transfer of maternal antibody active against the RBCs of the fetus, that is, isoimmune hemolytic anemia (Chapter 97.2). Various other immune hemolytic anemias are autoimmune (see Table 458-1) and may be idiopathic or related to various infections (Epstein-Barr virus, rarely HIV, cytomegalovirus, and mycoplasma), immunologic diseases (systemic lupus erythematosus [SLE], rheumatoid arthritis), immunodeficiency diseases (agammaglobulinemia, autoimmune lymphoproliferative disorder, dysgammaglobulinemias), neoplasms (lymphoma, leukemia, and Hodgkin disease), or drugs (methyldopa, L-dopa). Other drugs (penicillins, cephalosporins) cause hemolysis by means of “drug-dependent antibodies—that is antibodies directed toward the drug and in some cases toward an RBC membrane antigen as well.
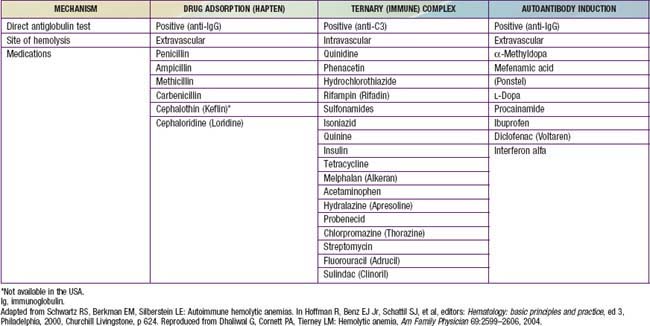
Table 458-1 DISEASES CHARACTERIZED BY IMMUNE-MEDIATED RED BLOOD CELL DESTRUCTION
AUTOIMMUNE HEMOLYTIC ANEMIA DUE TO WARM REACTIVE AUTOANTIBODIES
AUTOIMMUNE HEMOLYTIC ANEMIA DUE TO COLD REACTIVE AUTOANTIBODIES (CRYOPATHIC HEMOLYTIC SYNDROMES)
DRUG-INDUCED IMMUNE HEMOLYTIC ANEMIA (see Table 458-2)
Modified from Packman CH: Autoimmune hemolytic anemias. In Rakel R, editor: Conn’s current therapy, Philadelphia, 1995, WB Saunders, p 305.
Autoimmune Hemolytic Anemias Associated With “Warm” Antibodies
Etiology
In most instances of warm antibody hemolysis, no underlying cause can be found; this is the primary or idiopathic type (see Table 458-1). If the autoimmune hemolysis is associated with an underlying disease, such as a lymphoproliferative disorder, SLE, or immunodeficiency, it is secondary. In as many as 20% of cases of immune hemolysis, drugs may be implicated (Table 458-2).
Drugs (penicillin or sometimes cephalosporins) that cause hemolysis via the “hapten” mechanism (immune but not autoimmune) bind tightly to the RBC membrane (see Table 458-1). Antibodies to the drug, either newly or previously formed, bind to the drug molecules on RBCs, mediating their destruction in the spleen. In other cases, certain drugs, such as quinine and quinidine, do not bind to RBCs but, rather, form part of a “ternary complex,” consisting of the drug, an RBC membrane antigen, and an antibody that recognizes both (see Table 458-1). Methyldopa and sometimes cephalosporins may, by unknown mechanisms, incite true autoantibodies to RBC membrane antigens, so that the presence of the drug is not required to cause hemolysis.
Autoimmune Hemolytic Anemias Associated with “Cold” Antibodies
Berentsen S, Ulvestad E, Gjertsen BT, et al. Rituximab for primary cold agglutinin disease: a prospective study of 37 courses of therapy in 27 patients. Blood. 2004;103:2925-2928.
Flores G, Cunningham-Rundles C, Newland AC, et al. Efficacy of intravenous immunoglobulin in the treatment of autoimmune hemolytic anemia: results in 73 patients. Am J Hematol. 1993;44:237-242.
Gehrs BC, Friedberg RC. Autoimmune hemolytic anemia. Am J Hematol. 2002;69:258-271.
King KE, Ness PM. Treatment of hemolytic anemia. Semin Hematol. 2005;42:131-136.
Packman CH. Hemolytic anemia resulting from immune injury. In: Kanshansky K, Lichtman MA, Beutler E, et al, editors. Williams hematology. ed 8. New York: McGraw-Hill; 2010:777-798.
Petz L. Treatment of autoimmune hemolytic anemias. Curr Opin Hematol. 2001;8:411-416.
Sève P, Bourdillon L, Sarrot-Reynauld F, et al. Autoimmune hemolytic anemia and common variable immunodeficiency. Medicine. 2008;87:177-184.
Sparling TG, Andricevic M, Wass H. Remission of cold hemagglutinin disease induced by rituximab therapy. CMAJ. 2001;164:1405.
Zecca M, Nobili B, Ramenghi U, et al. Rituximab for the treatment of refractory autoimmune hemolytic anemia in children. Blood. 2003;101:3857.