Hemo-dynamo Doc
Christopher J. Gallagher
The crew of Apollo 13 solved their problems.
Go through these problems, and you, too, can be a Hemodynamo-Doc.
Case 1
Your job, should you decide to accept it, is to calculate:
Area of a circle, you recall from 8th grade or so, is pi × radius squared. Since pi is 3.14 and since radius = diameter divided by 2, then the area equation can be simplified to area = 3.14 × diameter squared/2 squared, or 3.14 × diameter squared/4. Crank out a little division and you come up with:
So let’s wander back to the stroke volume thing.
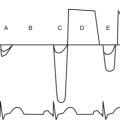
As you do these problems, pay attention to two things:
I wouldn’t sell such a person life insurance.
Do your problem, then step back. Look at the units. Use common sense.
Calculation of Peak Right Ventricular Systolic Pressure
Sorry, the free ride is over, you’ll have to put your thinking cap back on for this one.
For this, you’ll need two things, one mathematical, and one commonsensical/visual.
The Mathematical
The Bernoulli equation will appear a million times in any discussion of TEE. The complicated form of this equation takes Sir Isaac Newton to decipher, but the simplified version comes to us as the digestible.
Calculation of Peak Aortic Valve Area
Here the continuity equation comes home to roost. At first baffling, the continuity equation makes sense: it’s just a question of cross multiplying and dividing, and shouldn’t make you lose much sleep.
Ah, grasshopper, things are not so simple as they seem.
Continuity Equation Idea: flow through one area of the heart equals flow through another area of the heart.
So, if you can measure flow through one area, then that should equal flow in another area.
Flow here = flow there. The essence of the continuity equation.
We know we want to know the aortic valve area, so where can we find another place to measure stuff?
You have the diameter of the LVOT, 2.2 cm, so use the area formula:
Cross multiply and divide, solving for the area of the aortic valve, and, voila!
Does this pass the units test? Yes. Aortic valve areas are measured in cm squared.
No, really, look back up there, don’t take this on faith.
So, here we go with the second way to calculate the area of the aortic valve.
Cross multiply and divide, and gee whiz golly, the aortic valve area is still 1.1 cm squared.
That shouldn’t surprise you, as this patient hasn’t aged much during this problem.
Calculation of Peak Aortic Valve Gradient
A little less Sturm und Drang here. Just use the Bernoulli equation:
(Keep in mind, you need that velocity in m/sec to get a pressure in mmHg!)
Case 2
• Mitral annular diameter: 3.5 cm
• TVI mitral annular diameter: 11 cm
• PISA alias velocity: 34 cm/sec
Before you regurgitate yourself at all this stuff, a few pointers.
PISA’s area is a hemisphere, so that’s a little different.
PISA’s area is affected by its angle to the valve, so that’s a little different.
PISA implies you know what the hell aliasing is, so that’s a little different.
Alright, so PISA is a pain in the ass, what can I tell you? I didn’t make up the exam!
Calculation of LVOT Stroke Volume
Whew, this is review. If you got the karma of the first case, this should be cake. I’ll go through it just as slowly, though, so we jam this stuff into your sulci but good.
Next, we look at the LVOT, make our area calculation, then multiply it by the length (the TVI):
Calculation of MV Stroke Volume
Danger! Danger, Will Robinson! Remember, when you measure these, to measure both the diameter and the TVI at the same place. In this problem, be sure to measure both the diameter of the mitral valve and the TVI of the mitral valve at the annulus. If you measure the diameter at the annulus and the TVI at, say, the tips of the mitral valve, then you would get an inaccurate result.
So once again, we are invoking a “cylinder of blood flow”.
Confused? Pause for a moment and think about what’s happening.
So, in review, the units check and the common sense also checks, once you think about what is happening and when it is happening.
Calculation of MV Regurgitant Volume
Now it starts to come together.
Calculation of MV Regurgitant Fraction
No rocket science here.
or, in percentage terms, regurgitant percentage = 40%.
Calculation of Regurgitant Orifice Area
This is a little hypothetical, as the regurgitant orifice area is not a fixed thing that instantly appears, then instantly disappears. In reality, it’s more like a door that is closed, opens at a certain speed, stays open for a length of time, and then closes at a certain speed. This calculation looks at the “door all the way open” and ignores the reality of the “opening period” and the “closing period”.
But you’re not here to think. Just do the calculation and keep your trap shut.
Go back to our cylinder of blood and start calculating.
Cross multiply and divide, you busy little hemodynamic beavers.
PISA Calculations
Hunker down, cowboys and cowgirls, it’s not so bad as you think. Before we go into the actual calculations in this case, let’s go over the main aspects of PISAtology.
Look at the words that make up PISA, and draw pictures to illustrate the point.
Proximal! On the near side of the choke point, that is, in the left atrium.
Again, a radius on the far side of the choke point doesn’t make sense.
Think of water going toward a narrow sluice gate. The velocities are all over the map, until you get real close; then the pressure bearing down on the water is all the same. The velocities “organize” as the water gets closer to the sluice gate, and you get a hemisphere of water all going the same speed toward that narrow opening. That is why you get a hemisphere of “isovelocity-ness” that appears on the TEE screen.
Calculation of Regurgitant Flow Rate by PISA
Just as in other valve calculations, invent the idea of a cylinder of blood flowing along with a certain area and a certain length. This requires a little mind bending, as you are used to looking at the area of a circle and multiplying it by the length. Here, with PISA calling the shots, you make an area of a hemisphere and multiply it by the length.
Try not to think about it too much, you might pop an aneurysm. Just go with the flow.
Wait, wait! Where did that aliasing velocity come from again?
Units OK? Check. (Again, you get Brownie points if you got nervous about the aliasing velocity not being the same as the TVI.) Common sense? Yes.
Calculation of Regurgitant Orifice Area by PISA
Here we’ll keep an especially close eye on the units.
Cross multiply and divide and you get ERO = 0.24 cm squared.
Case 3
Calculation of Stroke Volume
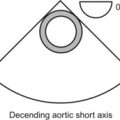
Find an area, find a TVI, and create your cylinder of blood flow to give you your volume. No problem, we’ve done it before.
SCREEEEEEEEEEEEEEEEEEEEEEEEEEEEEEEECH!
But! But! What about the tricuspid regurg? Doesn’t that “undo” the continuity equation?
If no flow goes backward from the pulmonary artery on out (that is, the pulmonary artery itself is not regurgitant), then the continuity equation says, “the flow will flow”.
So, now that we’ve settled that, then we can calculate our stroke volume:
Calculation of Peak Right Ventricular Systolic Pressure
Here again a picture will keep your signs straight. Whether on the right side or the left side of the heart, think of what’s going on (here, systolic flow from the right ventricle into the right atrium through the “choke point” of the regurgitant tricuspid valve), think of where the highest pressure should be (here, the right ventricle), the place where the gradient will occur (the tricuspid valve), and the low-pressure place (the right atrium). So, the equation will say:
How to measure the “choke point”? We have a velocity (which TEE can measure). Plug in Bernoulli:
Units check? Yes. Common sense? Yes.
It all fits. The numbers match the clinical reality. Isn’t science wonderful?
Calculation of Aortic Valve Area
Back to the continuity equation (didn’t I tell you you just keep doing the same stuff over and over again?).
In days of yore, we did this with the LVOT, remember?
Plug in: Area PA × TVI PA = area AV (the unknown) × TVI AV
Cross multiply and divide, you get AV area = 2 cm squared.
Go back to Case 1. Remember how we worked out the AV area another way?
Case 4
60-yo male with acute aortic dissection and aortic insufficiency.
Calculation of LVOT Stroke Volume
Some things never change, ain’t it grand.
It’s worth reminding yourself where you get all these numbers from. You measure the LVOT about 5 to 10 mm proximal to the annulus of the aortic valve. You measure the LVOT velocity (around which you draw your cursor to get the TVI) at the EXACT SAME PLACE, using… well, you tell me. Do you use continuous-wave Doppler or pulsed-wave Doppler?
(Play the theme from Jeopardy here.)
Right, pulsed-wave Doppler. Pulsed wave gives you a specific velocity at a specific place, unlike continuous wave, which gives you ALL velocities along a line. (If this is still a mystery to you, review the difference between continuous wave and pulsed wave in Chapter 2; you need to know this ice cold.)
Calculation of Mitral Valve Stroke Volume
Same deal here. Create your cylinder of blood, get an area, get a length, and you’re in business. Again, we’ll “round out” the “what is really oval” mitral valve.
Let’s step outside the numbers again to make sure we got the numbers from the right place.
You measured the mitral valve, where, the annulus or the tips of the leaflets?
Where do you measure the velocity?
Same place. Get the stuff at the same place, not different places!
Which kind of Doppler did you use?
Pulsed wave, because we wanted a specific velocity at a specific place.
Calculation of Aortic Regurgitant Volume
Note well, young budding TEE’ogists. To calculate the aortic regurgitant volume, you must assume there is no mitral regurgitation going on either. Again, you need one equation, one unknown. Put in one equation and two unknowns, it won’t work.
Calculation of Aortic Regurgitant Fraction
What amount of the total ejected blood ends up going backward?
Regurgitant volume aortic insufficiency/forward volume through LVOT = regurgitant fraction
Units check? (Do it every time) Yes. Common sense check? Yes.
Calculation of Aortic Regurgitant Orifice Area
Back to the cylinder of blood moving around. Get an area, multiply it by a length, and that gives you the volume of your cylinder of blood. Make sure the area and the velocity (recall that the velocity, when outlined, yields your TVI, or, length), are measured at the same place.
Units? Good. Common sense? Um. That’s pretty tiny for an aortic valve, but wait, this is the area where regurgitation is occurring, not the entire valve area. You can picture that this patient has an aortic dissection, so the aortic root is stretched, making the aortic valves not able to completely reach each other, and leaving a small area “uncovered” in the middle. Through that, 23 mL of blood per beat flows back into the heart. Then, yes, the aortic regurgitant orifice area of 0.14 cm squared makes sense.
Calculation of Cardiac Output
You are interested in what goes forward here. Regurgitant flow is not really output, it’s “backward-put”. So to calculate cardiac output, you need a real, live stroke volume that actually gets “out there,” and as well you need a heart rate.
Look at flow in a different way to convince yourself that the continuity equation holds.
Case 5
70-yo male with worsening dyspnea on exertion.
Calculation of Mitral Valve Area by Pressure Half-time
Where the hell did pressure half-time come from?
The quantitative equation has been empirically worked out:
How? Doppler half-times were compared to cath lab studies, and this magic number appeared.
So, back to the problem, what is the mitral valve area by PHT?
Calculation of Mitral Valve Area by Continuity Equation
So, we have a cylinder of blood in which we can measure the flow through our old friend, the LVOT:
Calculation of Pulmonary Artery Diastolic Pressure
Remember, we’re in diastole. Know where the high-pressure area, the choke point (where we’ll get a gradient), and the low-pressure area with its “leftover” pressure are.
Uh, er…Where is the RV EDP? Have we got one equation, two unknowns? I cry foul!
Satisfy yourself that the units and the common sense hold true.
Case 6
Calculation of Area of PISA
PISA area = 2 × pi × radius squared when the PISA hemisphere is flush and flat against the mitral valve. But when the PISA is at an angle to the mitral valve annulus plane, then the PISA area is less. The area of the PISA is then
Consider 90 degrees. That looks like, and does, cut the area off by half.
Calculation of Mitral Valve Area Using PISA
Um. Wait a minute here. Time and again, we’ve used the cylinder idea. You have an area; multiply it by a length (the TVI), and you get your stroke volume. The units work out right, common sense usually prevails, Ford’s in his flivver, and all’s right with the world.
To review, then, this problem yields:
Cross multiply and divide and you get:
Holy consistency, Batman, the area turns out the same, even after all that work!
Calculation of Mitral Valve Regurgitant Volume
Hubbada bubbada, what do we need to get this one? This does not jump off the page and drip obviousness.
Now, what paths do we have OUT of the ventricle?
A ventricle filled with 55 mL divides its two exit pathways into two:
Calculation of Mitral Valve Regurgitant Fraction
Nothing earth-shattering here:
Units, common sense? Yeah, yeah, yeah. When will this chapter ever end?
Case 7
56-yo man presents for AV surgery.
Calculation of LVOT Stroke Volume
Move the cylinder, move the cylinder, move the cylinder of blood.
which makes sense in terms of both units and normal physiology.
Calculation of Cardiac Output and Index
Puh-leeze! After jumping through the flaming hoops of PISA alpha angles, this is downright pedestrian.
That’s more like it. That unit makes sense, and an output of 7.3 L/min you’ve seen before in the OR.
Calculation of Pulmonary Artery Systolic Pressure
Go with the concept of finding the high-pressure area, finding the choke point where you lose pressure across a gradient, and the leftover low-pressure area.
That’s, sort of, going the wrong way. Hmm. Think, think, think, like Winnie the Pooh does.
That’s a start. The pulmonary artery systolic pressure will be the right ventricular systolic pressure. Can we figure that out?
You CAN figure these things out, even when it’s not super obvious!
Case 8
Calculation of Aortic Valve Area
What’s with the side schtick? I got the cylinder thing down like nuthin’, and now we got, what, Euclidean geometry, come on!
Chill. Like Avril Lavigne says in her song, “It’s all been done before”.
Just when you had it all figured out, they throw in a normal one to screw you up.
Case 9
Calculation of Cardiac Output
Remember the anatomy; you can do the simple:
Calculation of Peak Right Ventricular Systolic Pressure
Where is the high-pressure chamber? The left ventricle. Since there is no aortic stenosis, the systolic pressure in the left ventricle is all conveyed to the aorta. So we can take the systemic pressure as our left ventricular pressure.
Where is the low-pressure point? The right ventricle. (Our unknown.)
And that, in so many words, is that. You are now a bona fide Hemodynamo-Doc.