Heat Illness
Definitions
1. Environmental temperature exceeding 35° C (95° F) with humidity level greater than 80%
2. Dehydration (one indicator in the field is dark yellow urine)
Disorders
Heat Syncope
Treatment
1. Perform a full secondary assessment after the primary survey to assess for any trauma that may have occurred because of a fall.
2. Place the patient in the Trendelenburg position.
3. Cool the patient, and administer oral fluids when he or she is awake and alert. The body can absorb a carbohydrate-containing beverage, such as Gatorade, faster than plain water. The concentration of carbohydrates in such a beverage should not exceed 6%; otherwise, gastric emptying and fluid absorption by the intestines may be delayed. Responders should target an intake for the patient of 1 to 2 L (1.1 to 2.1 qt) over the first hour.
4. Patients with heat syncope usually recover rapidly with treatment. If the patient does not improve or worsens, he or she should be evaluated for heatstroke or other potential cause of syncope and transported to a hospital immediately.
Heat Exhaustion
Treatment
1. Stop all exertion, and move the patient to a cool and shaded environment.
2. Remove restrictive clothing.
3. Administer oral fluids (see Heat Cramps, earlier).
4. Cool the patient by placing ice or cold packs on the neck, chest wall, axillae, and groin. Do not place ice directly against skin to avoid frostbite injury. Fanning the patient, while spraying with tepid water, is also an effective cooling method.
5. Generally patients recover rapidly, and hospitalization is not necessary.
Heatstroke
Signs and Symptoms
Treatment
1. Cool the patient rapidly. Prognosis is a function of the magnitude and duration of hyperthermia. The faster cooling is accomplished, the lower the morbidity and mortality.
a. Place ice or cold packs on the neck, axillae, chest wall, and groin. Take care to avoid creating a frostbite injury.
b. Wet the patient with tepid (not cold) water, then fan rapidly to facilitate evaporative cooling.
2. Protect the airway, and do not give anything by mouth because of the risk for vomiting and aspiration.
3. Administer fluid intravenously (1 to 2 L of normal saline solution as an initial bolus in adults and 20 to 40 mL/kg in children).
4. Treat seizures and combative behavior with a benzodiazepine (diazepam 0.1 to 0.3 mg/kg IV or IM adult dose; midazolam 0.2 mg/kg IV or IM adult dose).
5. Suppress shivering by administering a benzodiazepine (diazepam 5 to 10 mg IV adult dose) or chlorpromazine (25 to 50 mg IM or IV adult dose).
6. Evacuate the patient immediately to the nearest medical facility. Continue to cool the patient during transport until his or her core body temperature has fallen to 38° to 39° C (100.4° to 102.2° F).
Prevention
The best indicator of environmental heat stress is the wet bulb globe temperature (WBGT). Whereas a regular thermometer measures the dry-air temperature, a wet bulb thermometer (WBT) measures the effect of humidity as well as temperature. The standard dry bulb thermometer temperature by itself is a poor predictor of heat stress because humidity is such an important factor in heat dissipation accomplished by sweating. Because the WBGT is complex and 70% of the value is derived from the WBT, a simple alternative in the field is to use a sling psychrometer. This instrument has a thermometer with a wick surrounding the bulb attached to an aluminum frame with a hinged handle. After the wick is moistened, the psychrometer is slung over the head for approximately 2 minutes. Air passing over the wetted thermometer bulb cools the bulb in inverse proportion to the humidity. The WBGT can be used as a guide for recommended activity levels (Table 5-1).
Table 5-1
Wet Bulb Globe Temperature and Recommended Activity Levels
| °C | °F | RECOMMENDATIONS |
| 15.5 | 60 | No precautions necessary |
| 16.1-21.1 | 61-70 | No precautions if adequate hydration maintained |
| 21.7-23.8 | 71-75 | Unacclimatized: curtail exercise |
| Acclimatized: exercise with caution; rest periods and water breaks every 20 to 30 minutes | ||
| 24.4-26.6 | 76-80 | Unacclimatized: avoid hiking or sports or sun exposure |
| Acclimatized: heavy to moderate work with caution | ||
| 27.2-29.4 | 81-85 | Limited brief activity for acclimatized, fit persons only |
| 31 | 88 | Avoid activity and sun exposure |
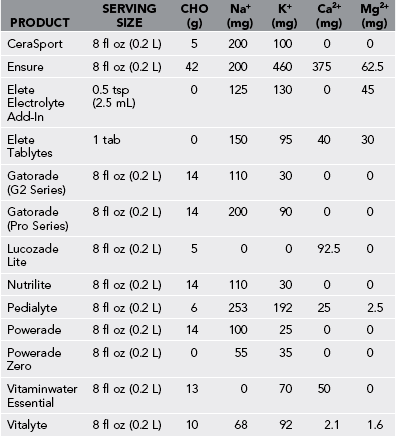
The Institute of Medicine provides general guidance for composition of “sports beverages” for persons performing prolonged physical activity in hot weather. They recommend that fluid replacement beverages contain approximately 20 to 30 mEq/L sodium (chloride as the anion), approximately 2 to 5 mEq/L potassium, and approximately 6% carbohydrate. The sodium and potassium are used to help replace sweat electrolyte losses, while sodium also helps to stimulate thirst, and carbohydrate provides energy and facilitates intestinal absorption. These components can also be consumed using nonfluid sources such as gels, energy bars, and other foods. Drinks containing sodium, such as sports beverages, may be helpful, but many foods can supply the needed electrolytes. A little extra salt may be added to meals and recovery fluids when sweat sodium losses are high. Table 5-2 presents the electrolyte contents of common sport drinks, tablets, and powdered additives that can be used to help replace electrolytes lost during activity or exercise.