HEAD INJURY
Victims of head injury can be divided into two groups, according to whether or not they have lost consciousness. Always be aware that the dazed or unconscious victim cannot protect his airway; you must be vigilant in your observation. The most common complication of head injury is obstruction of the airway with the tongue, blood, or vomitus. The most common associated serious injury is a broken neck.
LOSS OF CONSCIOUSNESS
1. Protect the airway (see page 22) and cervical spine (see page 37).
2. If the victim wakes up after no more than a minute or two and quickly regains his normal mental status and physical abilities, he has probably suffered a minor injury—so long as there is no relapse into unconsciousness or persistent lethargy, nausea or vomiting, or severe headache. If the victim is far from help, he should undertake no vigorous activity and be kept under close observation for at least 24 hours. It is commonly taught that after someone has sustained a head injury with loss of consciousness (implying a concussion), he or she should be kept awake. It is also taught that if the victim falls asleep, he should be awakened regularly, presumably to demonstrate that he can be woken up, and has not worsened or lapsed into a coma. However, be aware that sleeping in and of itself has no influence on the progression of the head injury. Furthermore, some persons who have suffered a concussion (or worse) become sleepy. If they fall asleep, they will not worsen because they fall asleep. If they worsen, it is part of the progression of the head injury, not related in any way to sleep. You cannot keep someone awake forever, because they need sleep in order to rest.
3. Confusion or amnesia for the event that caused the blackout is not uncommon and not necessarily serious, so long as the confusion does not persist for more than 30 to 45 minutes. Because a serious brain injury may not become apparent for hours, the wilderness traveler who has been knocked out should not venture farther from civilization for 24 hours. If headache or nausea persists beyond 2 to 3 hours, the victim should begin to make his way (assisted by rescuers) to medical care.
4. If the victim wakes up and is at first completely normal, only to become drowsy or disoriented, or to lapse back into unconsciousness (typically, after 30 to 60 minutes of normal behavior), he should be evacuated and rushed to a hospital. This may indicate bleeding from an artery inside the skull, causing an expanding blood clot (epidural hematoma) that compresses the brain. Frequently, the unconscious victim with an epidural hematoma will be noted to have one pupil significantly larger than the other (Figure 36).
5. If the victim awakens but has a severe headache, bleeding from the ears or nose with no obvious external injury to those organs, clear fluid draining from the ear or nose, unequal-sized or poorly reactive (do not constrict promptly on exposure to bright light) pupils, weakness, bruising behind the ears or under the eyes, vomiting, or persistent drowsiness, he might have a skull fracture. Such signs mandate immediate evacuation to a medical facility.
6. If the victim suffers a seizure (see page 68) after a head injury, no matter how brief, he should be transported to a medical facility.
7. If the victim does not wake up promptly after a head injury (unconscious for more than 10 minutes), has bleeding from an ear, has unequal or nonreactive (do not constrict to bright light) pupils, has clear fluid from the nose, has a profound headache, is weak in an arm or leg, is disoriented, or has a fluctuating level of consciousness (normal one minute, drowsy the next), he may have suffered a significant brain injury and should be immediately rushed to a medical facility. Because there is a high incidence of associated neck injuries, any person with a serious head injury should have his cervical spine immobilized (see page 37). Head injuries often cause vomiting. Therefore, be prepared to turn the victim on his side so that he doesn’t choke (see page 24).
8. Glasgow Coma Scale (GCS). This scale is used by medical professionals as a guide to the presence of head injury and to follow the progress of a head-injured victim.
| Eye Opening | Spontaneous | 4 |
| To voice | 3 | |
| To pain | 2 | |
| None | 1 | |
| Best Verbal Response | Oriented | 5 |
| Confused | 4 | |
| Inappropriate | 3 | |
| Incomprehensible | 2 | |
| None | 1 | |
| Best Motor Response | Obeys commands | 6 |
| Localizes pain | 5 | |
| Withdraws from pain | 4 | |
| Flexes the limbs | 3 | |
| Extends the limbs | 2 | |
| None | ||
| Total Score | 3 to 15 |
13 to 14 is mild brain injury
9 to 12 is moderate brain injury
3 to 8 is severe brain injury
Even persons with a GCS score of 15 can deteriorate if they have suffered apparently minor head injuries. Warning signs for persons who might have a serious problem include vomiting, restlessness, observed decrease in GCS score, severe headache, confusion, and a focal blow to the side of the head. So, if a person appears normal, but has suffered any one of these, he or she is perhaps at a greater risk for having a serious brain injury. This person therefore should be watched very closely. If you are far from medical attention, you should make plans for a prompt evacuation.
LACERATIONS OF THE SCALP
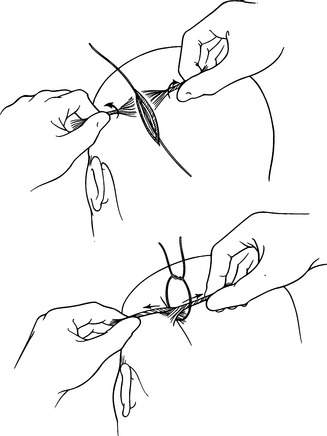
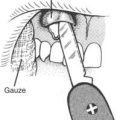
Cuts of the scalp tend to bleed freely, because the blood vessels are positioned in the thick skin in such a way that they cannot go into spasm and seal off after they are severed. For this reason, it is important to apply prolonged firm pressure to any head wound, and to seek care as soon as possible. If possible, any closure method should be preceded by a quick, vigorous rinse of the wound to remove any large pieces of dirt, gravel, or other debris. One way to keep the edges of the wound together is to first lay a long piece of string or dental floss along and beyond the length of the wound. Next, twirl hair on direct opposite sides of the wound to form strands, and then pull these strands toward each other to pull the skin together. Then, use the string to tie the hair strands together (Figure 37). Repeat this process as necessary to account for the entire open length of the wound. If the wound is large and you do not have any string, you may be able to bring the edges together by tying hair taken from opposite sides of the wound, but this is often quite difficult.
For information regarding wound repair and bandaging, see pages 260 and 276.