Chapter 23. Head injuries
The central nervous system has no stores of oxygen or glucose; if the blood supply is interrupted, depriving the brain of oxygen, consciousness is lost within 15–20 seconds. The brain cells will then die within 3–4 minutes.
Because the skull is a rigid box, tissue swelling or bleeding within it will lead to an increase in pressure. As the pressure rises, the brain is pushed down, impacting on rigid structures such as the tentorium and the foramen magnum. This leads to reduced consciousness and eventually causes death by coning, the compression of cardiorespiratory centres within the brainstem.
Any head injury should raise the suspicion of associated c-spine injury.
Risk factors for head injury include:
• Alcohol abuse
• Drug abuse
• Anticoagulants
• Blood clotting disorders
• Other drugs including tranquillisers
• The elderly especially with dementia.
The key to the optimal management of head-injured patients is the prevention of secondary brain damage by appropriate attention to the airway, breathing and circulation.
Primary and secondary brain injury
Definitions: The brain injury sustained at the time of the accident is known as the primary injury and cannot be reduced once it has occurred
Secondary brain injury is a combination of factors that lead to additional brain injury and cell death following the primary injury
Any episode of hypoxia or hypotension will significantly worsen the patient’s outcome from head injury. As hypoxia affects the brain as a whole there is generalised swelling – cerebral oedema – which results in raised intracranial pressure (ICP). When the intracranial pressure approaches the arterial pressure, blood cannot flow through the brain and so cells will die.
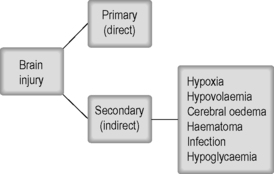 |
| Figure 23.1. |
| Primary and secondary brain injury. |
The important blood pressure for the brain is not the mean arterial pressure (MAP) alone, but the perfusion pressure (PP). The cerebral perfusion pressure is the mean arterial pressure minus the mean intracranial pressure (MICP): PP = MAP − MICP.
Both a fall in mean arterial pressure and a rise in intracranial pressure may therefore reduce cerebral perfusion pressure and produce secondary brain injury.
Treatment should aim to maintain the cerebral perfusion pressure and keep the patient’s arterial pressure near normal limits and above 100 mmHg in the adult. Raised central venous pressure also leads to increased ICP. Anything that increases central venous pressure, for example a tension pneumothorax, must also be treated.
Signs of raised intracranial pressure:
• Decreasing level of consciousness
• Increasing blood pressure (late)
• Falling pulse rate (late)
• Decreasing respiratory rate (late)
• Pupillary dilation (late).
Generalised brain injury
Generalised or diffuse injuries represent a spectrum of injury from mild concussion with rapid and complete recovery to diffuse axonal injury (DAI) which is the principal cause of long-standing coma following head injury. Coma may last days or weeks or may be permanent.
Focal brain injuries
Localised or focal brain injuries consist of:
• Cerebral contusion
• Intracranial haemorrhages
• Lacerations and penetrating injuries.
Intracranial haemorrhage
Intracranial haemorrhage may be:
• Extradural bleeding: <1% of injuries, may be fatal but complete recovery is possible if treated within 2 hours
• Subdural bleeding: 30% of injuries, good recovery if treated within 2 hours but some residual disability is common
• Intracerebral bleeding: this is within the brain tissue itself
• Subarachnoid bleeding: within the subarachnoid space, produces headache and decreasing consciousness.
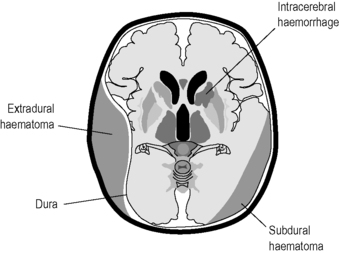 |
| Figure 23.2. |
| Anatomy of intracranial bleeding. |
Extradural haematoma – a history of rising intracranial pressure
An extradural haematoma is bleeding within the skull. Although the initial injury to the brain is liable to have caused concussion, the patient often recovers temporarily (a lucid interval) before deteriorating. As the size of the haematoma increases, intracranial pressure increases and the conscious level deteriorates.
As the pressure increases on one side of the brain, part of the temporal lobe herniates into the small space between the brain stem and the tentorium cerebelli. In this space is the third cranial nerve and as this is compressed, the pupil on the same side dilates.
As intracranial pressure continues to rise the herniating temporal lobe forces the brainstem against the opposite fold of tentorium, causing the opposite pupil to dilate and paralysis of the arm and leg of the opposite side of the body to the haematoma. This is a pre-terminal sign.
An alternative site of herniation is the foramen magnum. This is known as coning and results in the late development of bradycardia, hypertension and hypoventilation.
Classical clinical features of extradural haematoma:
• Loss of consciousness (initial concussion), followed by recovery
• Then increasing headache
• Then declining conscious level
• Weakness on the opposite side of the body to the head injury
• Dilated and fixed pupil on the same side as the injury.
Diagnosis can be difficult. The definitive investigation is a computed tomography (CT) scan. Patients with a significant period of unconsciousness (2–3 minutes or more) should be taken to a hospital that has 24-hour CT scanning facilities.
Penetrating injury
Brain haemorrhage can also be caused by penetrating trauma, inflicted by a low-velocity implement such as a knife, or by impalement in an industrial or traffic accident. The severity of the injury and any long-term disability is determined by the area of the brain which is injured. If the patient is unconscious after the penetrating injury the prognosis is exceedingly poor. Patients who are conscious and talking after such an injury can survive.
Skull fractures
Damage to the brain is demonstrated by an altered conscious level.
The clinical significance of a skull fracture is its potential relation to intracranial bleeding. The combination of a fracture of the skull and alteration of consciousness increases the chance of intracranial bleeding from 1 in 5000 to 1 in 4.
Linear skull fractures require no specific treatment. The emphasis is on the underlying brain injury, but when the skull fracture is depressed, and pressing on the brain tissue, urgent neurosurgical intervention is required.
Signs of a base of skull fracture may not appear until several hours after the injury and rarely develop before the patient arrives in hospital. Signs of basal skull fracture include:
• CSF leakage from nose (rhinorrhoea)
• CSF leakage from ear (otorrhoea)
• Panda (raccoon) eyes
• Battle’s sign
• Bleeding from the ears.
Very severe open injuries may expose the brain. Moist non-adherent dressings are needed to cover the area and to stop the brain tissue drying out. Scalp wounds should not be probed with a finger in the prehospital environment. They should be covered and left alone.
Patient assessment
The priorities in management are to protect the airway and ensure the delivery of oxygen to the brain
To achieve this there must be:
• an adequate airway (A)
• uncompromised breathing (B)
• adequate cerebral perfusion (C).
Assessment of the head-injured patient assumes the primary survey has been carried out, with appropriate management for the airway and protection of the cervical spine in every patient who is concussed or who has an altered conscious level. The level of consciousness should be assessed using the AVPU scale or the GCS.
Loss of consciousness and amnesia
Many patients cannot tell you whether they have been knocked out and certainly cannot reliably judge the period of unconsciousness.
Patients cannot remember the duration of coma.
Patients will say they lack memory of an event. This lack of memory is known as amnesia which can be post-traumatic or retrograde. Post-traumatic or anterograde amnesia is common. The duration of amnesia should be recorded. Retrograde amnesia (with memory loss of events prior to the head injury) is usually a sign of more significant injury.
‘Minor’ head injuries, where the patient has been knocked out for 1–2 seconds but then makes a full recovery, are extremely common, large numbers of these patients are admitted to hospital for head injury observation.
Symptoms attributed to head injury are known as concussion.
Any patient who has undergone loss of consciousness should be taken to hospital.
Patients who have prolonged post-traumatic amnesia of 5 minutes or more should also be assessed in hospital.
Always exclude head injury in:
• Epilepsy (post-ictal state)
• Alcohol abuse
• Drugs
• Dementia.
The above should never be simply accepted as the cause of an altered conscious level.
Lateralising signs
Assessment of upper and lower limb movement and sensation should be carried out. Loss of movement on one side of the body suggests an intracranial bleed – these are known as lateralising signs.
Pupils
Assessment of pupil function, documenting the size of the pupils and their response to light is an essential part of the primary survey.
Vital signs
The patient’s vital signs are of great significance, as they provide direct assessments of brain function. These signs include pulse rate, blood pressure, respiratory rate and temperature.
Blood glucose
Hypoglycaemia contributes to secondary brain injury and must be corrected. Recording of blood glucose levels by paramedics should be routine not only in diabetic patients but also in patients with major head injury.
Management
Effective and rapid management of the airway, breathing and circulation will effectively manage disability and head injury. There are additional details which can improve the management of the head injured patient.
Airway
• If the patient is irritable, aggressive and has a gag reflex, adequate airway maintenance can be one of the most difficult prehospital problems
• Use stepped airway management to establish a patent airway
• Insert an OP or nasal airway if tolerated, apply oxygen if tolerated. Otherwise evacuate immediately
• Patients with a GCS score of 8 or less (AVPU rating P or U) will require formal intubation to protect their airway
• Intubating without the use of paralysing drugs will likely increase the patient’s ICP. A careful ‘neuroprotective’ anaesthetic will be needed. This can only be carried out by a team trained in anaesthesia
• If the patient is trapped or cannot be transported to hospital within 15 minutes, the paramedic must consider calling medical help to the scene.
Breathing
• A normal respiratory rate is 10–18 breaths per minute in an adult, any respiratory rate above 18 breaths per minute should be assumed to be a sign of hypoxia, indicating that the patient requires oxygen
• Slow respiratory rates may be caused by drugs or by significant head injury
• A major aggravating factor in head injury is a tension pneumothorax As the pressure builds up in the chest cavity there is an increase of central venous pressure, resulting in a further increase in the intracranial pressure and precipitating further cerebral oedema. Relief of a tension pneumothorax as soon as possible by needle thoracocentesis can have a dramatic effect in reducing high cerebral pressures as well as improving ventilation.
Circulation
• Head injuries themselves do not cause low blood pressure, however, infants may lose a significant percentage of their blood volume into a scalp haematoma. This is less of a problem in adults although scalp lacerations can bleed heavily
• In the multiply injured patient the policy of maintaining a palpable radial pulse is appropriate
• This is less than ideal physiologically for the brain, as it may reduce cerebral perfusion, and a higher blood pressure endpoint is acceptable if there is definite isolated head injury.
Disability
• If possible, the patient should be transported at a slight ‘head-up’ angle of about 15°. This is only possible with some designs of stretcher trolley. This helps to maintain correct intracranial pressure.
Environment and exposure
• The unconscious patient will lose heat rapidly so keep them warm
• Blood glucose (BM Stix) should be checked and hypoglycaemia treated as low blood sugar will also lead to secondary brain injury.
Transfer to hospital
Ideally the assessment of a patient should be completed within 5 minutes, as longer on-scene times will be detrimental. Once the airway and cervical spine and breathing are stabilised, the patient should be rapidly transported to the nearest appropriate hospital. Obtaining IV access is best attempted in transit. At this stage a GCS score can be accurately assessed and can be continually monitored during the journey.
An appropriate hospital is one that has a 24-hour accident and emergency department and access to an available and working CT scanner. It is best to transfer the patients with serious head injuries to a hospital that has trained trauma teams and rapidly available neurosurgeons.
It is not efficient to treat patients by transferring them to the nearest hospital where they may be assessed over a period of 1–2 hours and then require a secondary transfer to a neurosurgical unit. The critical time for surgery may have passed, leading to increased mortality and morbidity rates.
For further information, see Ch. 23 in Emergency Care: A Textbook for Paramedics.