CHAPTER 25 Head and neck: overview and surface anatomy
This chapter contains an overview of the topographical anatomy of the head and neck described in detail in Chapters 26–34 Chapter 27 Chapter 28 Chapter 29 Chapter 30 Chapter 31 Chapter 32 Chapter 33 Chapter 34, and an account of the clinically relevant surface anatomy.
SKIN AND FASCIA
NECK
The superficial cervical fascia contains a variable amount of adipose tissue and platysma. The deep cervical fascia is conventionally subdivided into three sheets (investing, pretracheal and prevertebral layers) that surround the muscles and viscera of the neck to varying degrees, and the carotid sheath, a condensation of deep fascia around the common and internal carotid arteries, internal jugular vein, vagus and ansa cervicalis (see Ch. 28). The fascial layers of the neck define a number of potential tissue ‘spaces’ above and below the hyoid bone. In health, the tissues within these spaces are either closely applied to each other or are filled with relatively loose connective tissue. However, they offer potential routes by which unchecked infection may spread within the head and neck, and between the tissue spaces of the face and the mediastinum. They also offer convenient planes for intraoperative dissection during surgery.
BONES AND JOINTS
SKULL AND MANDIBLE
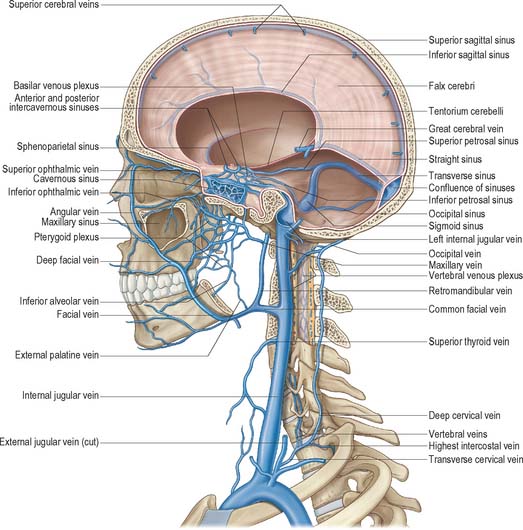
The skull is composed of 28 separate bones, most of them paired (Ch. 26). It can be divided into a robust calvarium that surrounds and protects the brain, and a delicate facial skeleton composed mainly of thin-walled bones, some of which contain air-filled cavities known collectively as the paranasal sinuses. The cranial cavity contains the brain and the intracranial portions of the cranial and spinal nerves; the blood vessels that supply and drain the brain and the haemopoietic marrow of the overlying bones; the meninges (dura, arachnoid and pia mater) and the cerebrospinal fluid (Ch. 27). The cavity is incompletely divided by dural partitions, notably the falx cerebri, lying between the cerebral hemispheres, and the tentorium cerebelli, lying between the cerebellum and occipital lobes. Almost all of the venous blood from the brain and cranial bones drains via sinuses lying between the endosteal and meningeal layers of the dura mater into the internal jugular vein (Ch. 27). Internally, the cranial base is divided into anterior, middle and posterior cranial fossae, which contain the frontal and temporal lobes of the cerebral hemispheres and the cerebellum respectively. Foramina in the bones of the skull base and facial skeleton transmit neurovascular bundles which may be compromised at these sites by pathology or trauma.
The skull provides attachments for numerous muscles. The craniofacial muscles arise from the bones of the facial skeleton, whereas the extrinsic muscles of the tongue, the muscles that act on the temporomandibular joint, the superior constrictor of the pharynx and the muscles of the soft palate all arise from sites on the cranial base. Movements of the mandible, which typically occur during mastication and articulation, take place at the temporomandibular joints (see Ch. 31). Movements of the skull on the cervical vertebrae occur at the atlanto-occipital joints (see Ch. 42).
CERVICAL VERTEBRAE
There are seven cervical vertebrae (see Ch. 42). They are the smallest of the movable vertebrae, and are characterized by a foramen in each transverse process, the foramen transversarium, and a disproportionately large vertebral canal. The first (atlas), second (axis) and seventh (vertebra prominens) cervical vertebrae are atypical.
HYOID BONE AND LARYNGEAL CARTILAGES
The hyoid bone (see Ch. 28) lies in the midline at the front of the neck at the level of the third cervical vertebra. It is suspended from the styloid processes by the stylohyoid ligaments and gives attachment to the supra- and infra-hyoid groups of muscles. The skeletal framework of the larynx is formed by a series of cartilages interconnected by ligaments and fibrous membranes, and moved by a number of muscles (Ch. 34). The laryngeal cartilages are the single cricoid, thyroid and epiglottic cartilages, and the paired arytenoid, cuneiform, corniculate and tritiate cartilages.
MUSCLES
The striated muscles of the head and neck produce the movements of the facial soft tissues that animate so many aspects of communication (Ch. 29); the movements at the temporomandibular joint that occur during mastication and speech (Ch. 31); the conjugate movements of the eyeballs (Ch. 39); and the co-ordinated movements that occur during activities such as swallowing, speaking and turning the head in response to visual and/or auditory stimuli. The ‘extrinsic’ muscles that run between the axial skeleton and upper limb act on the scapula and humerus (Ch. 46).
Smooth muscle occurs in the superior tarsal muscle, the sphincter and dilator pupillae and the ciliary muscle (Chs 39 and 40).
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
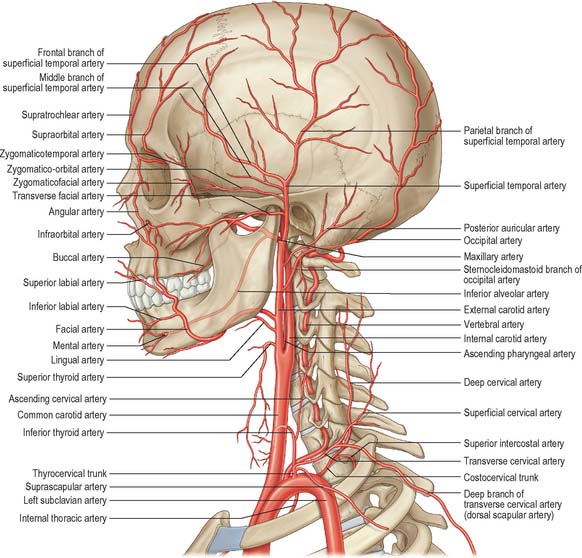
ARTERIAL SUPPLY
The main arterial supply of the head and neck is derived from branches of the carotid and subclavian arteries (Figs 25.1, 25.2). Branches of the internal carotid and vertebral arteries anastomose in the circle of Willis within the interpeduncular cistern on the ventral aspect of the brain (see Ch. 17).
Carotid system
The cervical portion of the common carotid artery is similar on both sides. Each lies within the carotid sheath of deep cervical fascia, together with the internal jugular vein and vagus nerve. In the lower part of the neck the arteries are separated by a narrow gap which contains the trachea, and higher up they are separated by the thyroid gland, larynx and pharynx. At the level of the upper border of the thyroid cartilage (C4), the common carotid artery bifurcates into external and internal carotid arteries (see below). The external carotid artery passes upwards on either side of the neck, inclined at first slightly forwards and then backwards and a little laterally. It usually gives off the ascending pharyngeal, superior thyroid, lingual, facial, occipital and posterior auricular arteries, and then enters the parotid salivary gland where it divides into its terminal branches, the superficial temporal and maxillary arteries. The branches of the external carotid artery supply the face, scalp, tongue, upper and lower teeth and gingivae, palatine tonsil, paranasal sinuses and nasopharyngeal tube, external and middle ears, pharynx, larynx and superior pole of the thyroid gland. They also anastomose with branches of the internal carotid arteries on the scalp, forehead and face, and in the orbit, nasopharynx and nasal cavity, and with branches of the subclavian artery in the pharynx, larynx and thyroid glands.
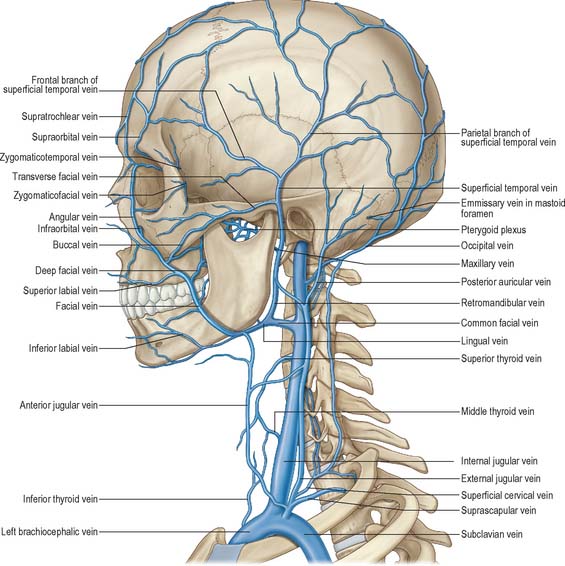
VENOUS DRAINAGE
Veins of the neck lie superficial or deep to the deep investing fascia. Superficial veins ultimately drain into either the external, anterior or posterior external jugular veins, and drain a much smaller volume of tissue than the deep veins. Deep veins tend to drain into either the internal jugular vein or the subclavian vein. The internal jugular vein drains blood from the skull, brain, superficial face and much of the neck. It descends in the neck within the carotid sheath and unites with the subclavian vein behind the sternal end of the clavicle to form the brachiocephalic vein (Figs 25.3, 25.4). At its junction with the internal jugular vein, the left subclavian vein usually receives the thoracic duct and the right subclavian vein receives the right lymphatic duct.
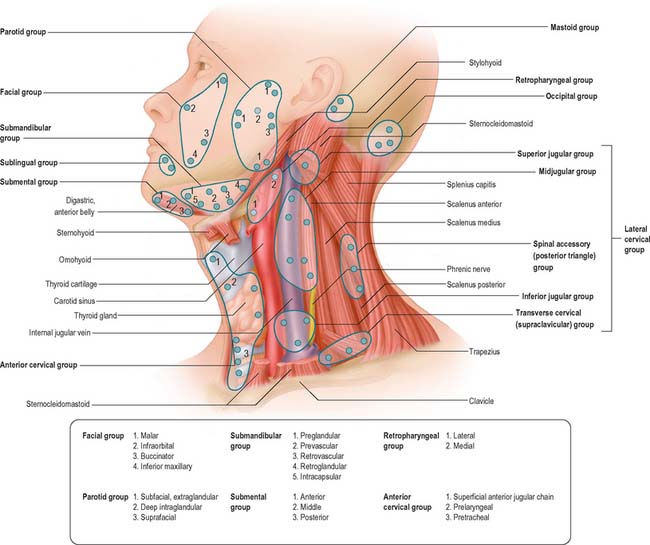
LYMPHATIC DRAINAGE
Lymph nodes in the head and neck are arranged in two horizontal rings and two vertical chains on either side of the neck (Fig. 25.5). The outer, superficial, ring consists of the occipital, preauricular (parotid), submandibular and submental nodes, and the inner, deep, ring is formed by clumps of mucosa associated lymphoid tissue (MALT) located primarily in the naso- and oro-pharynx (Waldeyer’s ring). The vertical chain consists of superior and inferior groups of nodes related to the carotid sheath. All lymph vessels of the head and neck drain into the deep cervical nodes, either directly from the tissues or indirectly via nodes in outlying groups. Lymph is returned to the systemic venous circulation via either the right lymphatic duct or the thoracic duct.
INNERVATION
CRANIAL NERVES
There are 12 pairs of cranial nerves. They are individually named and numbered (using Roman numerals) in a rostrocaudal sequence (see Table 15.1). Some are functionally mixed, others are either purely motor or purely sensory, and some also carry pre- or post-ganglionic parasympathetic fibres that are secretomotor to the salivary and lacrimal glands or motor to some of the smooth muscle within the eyeball. Branches of the oculomotor, trochlear, trigeminal, abducens, facial, glossopharyngeal, vagus, accessory and hypoglossal nerves supply muscle groups within the eyeball, face, pharynx, larynx and tongue. Branches of the trigeminal, glossopharyngeal and vagus nerves transmit general sensory information from the skin of the face and part of the scalp; the epithelium lining the oral and nasal cavities, the paranasal sinuses, middle ear, pharynx and larynx, and the dorsal surface of the tongue and the cornea; the intracranial meninges; the periosteum and bones of the skull. Branches of the trigeminal nerve innervate the temporomandibular joint. The olfactory, optic, trigeminal, facial, vestibulocochlear and vagus contain axons that transmit the special sensations of olfaction, vision, hearing, balance, and taste. The olfactory nerve is the only sensory cranial nerve that projects directly to the cerebral cortex rather than indirectly via the thalamus. The optic nerve terminates in the thalamus. The other ten pairs of cranial nerves are attached to the brainstem; their component fibres arise from or terminate in named cranial nerve nuclei (Ch. 19). The cranial nerves pass through named foramina in the skull, often with named vessels.
Reflexes
A number of reflexes involving structures in the head and neck are mediated by sensory and motor branches of certain of the cranial nerves, co-ordinated via appropriate nuclei in the brain stem. They include swallowing, gagging, retching and vomiting (Fig. 19.12); sneezing and coughing (Fig. 19.13); lacrimation (Fig. 39.25); jaw jerk (Fig. 19.17); visual reflexes (pupillary light reflex and accommodation) (see Ch. 40); corneal ‘blink’ reflex (Fig. 19.15); stapedial reflex (see p. 628, Ch. 36). Reflexes that involve energetic exhalation, e.g. sneezing and coughing, also involve the recruitment of cervical and thoracic spinal neurones to mediate the co-ordinated contraction of intercostal and abdominal wall muscles this activity requires.
SPINAL NERVES
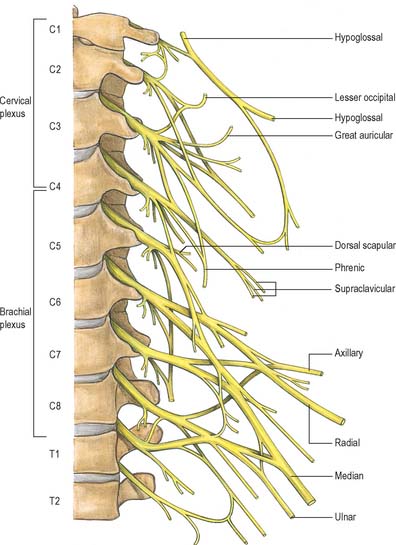
There are eight pairs of cervical spinal nerves (Fig. 25.6). Cutaneous branches of the dorsal rami of the second, third, fourth and fifth cervical nerves innervate the scalp and the skin over the back of the neck, and motor branches of all of the cervical dorsal rami supply cervical postvertebral muscles. All of the cervical ventral rami supply anterior and lateral groups of prevertebral muscles. The upper four cervical ventral rami form the cervical plexus whose branches collectively innervate the infrahyoid strap muscles and the diaphragm, and the skin covering the lateral and anterior parts of the neck, and the angle of the mandible. The lower four cervical ventral rami, together with most of the first thoracic ventral ramus, form the brachial plexus.
PARASYMPATHETIC NERVES
There are four pairs of parasympathetic ganglia in the head, named ciliary, pterygopalatine, otic and submandibular (Fig. 25.7).
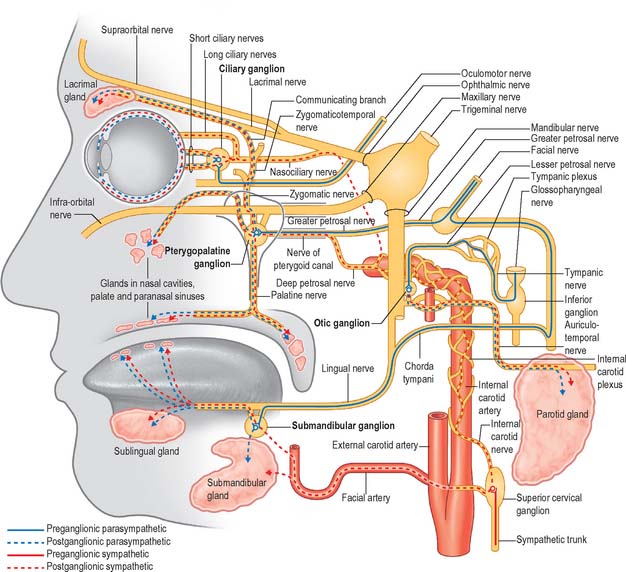
Fig. 25.7 Overview of the visceral efferent pathways in the head.
(Adapted from Drake, Vogl, Mitchell et al 2007.)
Submandibular ganglion
Preganglionic axons originate in the superior salivatory nucleus. They emerge from the brain stem in the nervus intermedius and leave the main facial nerve trunk in the middle ear to join the chorda tympani, which subsequently joins the lingual nerve. In this way, they reach the submandibular ganglion, where they synapse. Postganglionic fibres innervate the submandibular and sublingual salivary glands and are said to travel in the lingual nerve. Some preganglionic fibres may synapse around cells in the hilum of the submandibular gland. Stimulation of the chorda tympani dilates the arterioles in both glands as well as having a direct secretomotor effect.
SYMPATHETIC SYSTEM
In the neck the sympathetic trunk lies behind and medial to the carotid sheath and anterior to the transverse processes of the cervical vertebrae and the prevertebral muscles. There are usually three cervical ganglia on each side, superior, middle and inferior (cervicothoracic); they may be connected by a solid trunk or by two or three fibrous strands. The ganglia receive preganglionic fibres from neurones whose cell bodies lie in the intermediolateral column of the upper thoracic spinal cord: there is no preganglionic output from the cervical spinal cord. Postganglionic fibres reach their target tissues in the head and neck via the cervical spinal nerves and perivascular nerve plexuses distributed along the carotid and vertebral arteries (Fig. 25.7).
SURFACE ANATOMY
SURFACE ANATOMY OF THE HEAD
Skeletal landmarks
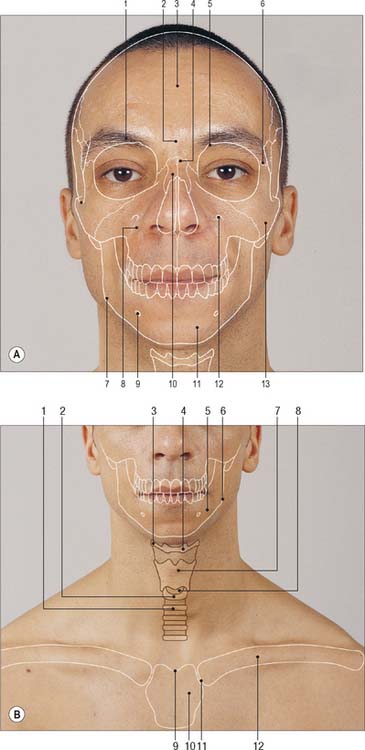
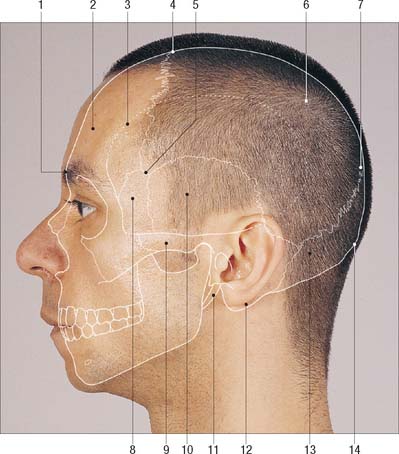
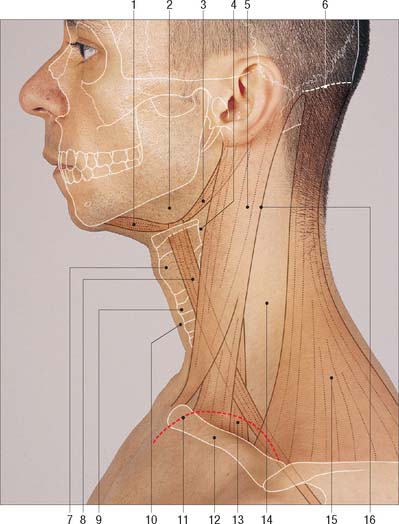
The palpable bony landmarks of the head can be examined from the back, sides and front (Figs 25.8, 25.9).
Skull and mandible
Calvarial landmarks are visible in bald people but more commonly they have to be palpated through the hair. The anterior fontanelle, at the junction of the coronal and sagittal sutures, may be palpated until approximately 18 months after birth (Ch. 26).
The ramus of the mandible, although largely covered by masseter, is easily palpable. Its posterior border may be palpated up to the neck of the condylar process, which lies just under the lobule of the ear. As the mouth is opened, the coronoid process can be felt to move from its resting position under the zygomatic arch. A finger probing inwards just behind the condylar process enters the small retromandibular fossa which is bordered anteriorly by the mandibular neck and superiorly by the inferior wall of the external acoustic meatus (Ch. 30). The latter is bounded anteriorly by the tragus, a small curved flap of cartilage, covered by skin, that partly projects over the orifice of the meatus. Articulation at the temporomandibular joint may be appreciated by palpating anterior to the tragus for the head of the condyle during mouth opening and closure.
Face
The lateral aspect of the face, from above downwards, consists of the temporal region, cheek and lower jaw (Ch. 29). The temporal region lies in front of the external ear and above the zygomatic arch. It is demarcated superiorly by the superior and inferior temporal lines, and inferiorly and laterally by the zygomatic arch. (The arch is formed by the zygomatic process of the temporal bone posteriorly and the temporal process of the zygomatic bone anteriorly, the two bones articulating at the zygomaticotemporal suture.) The variable prominence of the ‘cheekbone’ (zygoma) is largely attributable to the shape of the body of the underlying zygomatic bone. If the sharp posterior margin of the frontal process of the zygomatic bone is followed upwards, its fusion with the zygomatic process of the frontal bone at the zygomaticofrontal suture may be detected. Continuing posteriorly, in the line of a gentle arch, the temporal lines may be palpated. The lower temporal line terminates by curving downwards and forwards to end just above the root of the mastoid process as the supramastoid crest on the squamous part of the temporal bone. The suprameatal triangle, which lies above and behind the external acoustic meatus, overlies the lateral wall of the mastoid (tympanic) antrum. It is bounded above by the supramastoid crest, in front by the posterosuperior margin of the meatus, and behind by a vertical tangent to the posterior border of the meatus. The pterion is a small circular area within the temporal fossa which contains the junction of the frontal, sphenoid, parietal and temporal sutures. It usually lies 4 cm above the zygomatic arch and 3.5 cm behind the frontozygomatic suture, and marks the anterior (frontal) branch of the middle meningeal artery (Ch. 27) and the Sylvian point of the brain. Its position can be estimated roughly by a shallow palpable hollow, approximately 3.5 cm above the centre of the zygomatic bone. A knowledge of the surface anatomy of the middle meningeal artery is important for accurate positioning of burr-holes to evacuate extradural haematomas. The posterior (parietal) branch runs backwards and parallel with the upper border of the zygomatic arch and is usually exposed vertically above the mastoid process on a level horizontal with the upper margin of the orbit. The asterion is a craniometric point at the site of the postero-lateral, or mastoid, fontanelle. It is found at the junction of the lambdoid, occipitomastoid and parietomastoid sutures, and has been used as a landmark in lateral approaches to the posterior fossa. However, its reliability is questionable: burr holes placed at the asterion may often open the bone directly over the transverse-sigmoid sinus complex (Day & Tschabitscher 1998).
The forehead extends from the hair margin of the scalp to the eyebrows. The rounded frontal tuberosity may be felt approximately 3 cm above the midpoint of each supraorbital margin. The superciliary arch is usually palpable above the orbit and is better marked in the male than the female. The glabella, a small horizontal ridge, is easily palpable between the superciliary arches. Below the glabella the nasal bones meet the frontal bone in a small depression, the nasion, at the root of the nose. With a little finger inserted into the nostril, the bony margins of the anterior nasal aperture can be felt: they are formed by the inferior border of the nasal bone, the sharp margins of the nasal notch, and the coapted nasal spines of the maxillae (Ch. 32).
The orbital opening is somewhat quadrangular (Ch. 39). The supraorbital margin is formed entirely by the frontal bone and is easily palpable. At the junction of its sharp lateral two-thirds and rounded medial third (about two fingers’ breadth from the median plane) the supraorbital notch, if present, may be felt. This notch transmits the supraorbital nerve and vessels, and pressure exerted here with the fingernail can be painful. A frontal notch may also be found towards the bridge of the nose and is associated with the supratrochlear neurovascular bundle.
The anterior surface of the maxilla is extensive and may be palpated between the infraorbital margin and the alveolar processes that bear the upper teeth (when present). The canine eminence overlies the roots of the canine tooth and separates the incisive fossa anteriorly from the deeper canine fossa posteriorly. The bone in the canine fossa is thin and may be removed easily to access the maxillary sinus via an intraoral approach as part of a Caldwell–Luc procedure, e.g. to remove a tooth fragment that has been accidentally dislodged into the sinus during the attempted extraction of a posterior maxillary tooth in close proximity to the sinus. The palatine process of the maxilla, which forms the greater part of the roof of the mouth, is easily palpable within the mouth (Ch. 30).
Soft tissues and viscera
The muscular, fatty and cutaneous features which so clearly differentiate individuals are readily apparent on inspection. The external features of the eyelids and eyebrows are described in (Ch. 39). The tympanic membrane may be examined under direct vision using an auroscope and is described in (Ch. 36). The retinal vascular supply may be examined directly by ophthalmoscopy (Ch. 40).
Temporalis is palpable if the flat of the hand is placed on the side of the head and the jaw is clenched and unclenched, and the anterior border of masseter is prominent when the jaw is clenched. With the mouth open, it is possible to examine all the teeth and the palatine tonsils (when present), and to inspect and palpate the orifices of the parotid ducts. The palatine tonsil lies between the anterior and posterior pillars of the fauces (palatoglossus and palatopharyngeus respectively). Patients with a peritonsillar abscess (quinsy) present with ispilateral enlargement of the tonsil with displacement of the uvula to the contralateral side. The tongue may be examined for its general appearance and any abnormalities of movement, which may reflect neuronal damage. Deviation of the protruded tongue to the affected side, muscle wasting and fasciculation may occur following hypoglossal nerve injury.
Parotid gland
The parotid gland is soft and indistinct and lies largely below the external acoustic meatus, wedged between the ramus of the mandible, the mastoid process and sternocleidomastoid (Ch. 29). The anterior border of the gland is represented by a line descending from the mandibular condyle to a point just above the middle of masseter and then to a point approximately 2 cm below and behind the angle of the mandible. Its concave upper border corresponds to a curve traced from the mandibular condyle across the lobule of the ear to the mastoid process. The posterior border corresponds to a line drawn between the posterior ends of the anterior and upper borders. A large tumour of the deep lobe of the parotid may present as an intraoral mass. The parotid duct arises from the gland just above half-way along its anterior margin. It runs over masseter to its anterior border where it bends sharply and pierces the underlying buccinator opposite the upper second permanent molar. The orifice of the duct is visible as a small papilla within the cheek opposite the second upper molar tooth. Cannulation of the duct is integral to the procedures of sialography, ductal dilatation and basket retrieval of ductal stones (sialoliths). The duct can be palpated on the face at the anterior border of the clenched masseter, and its course can be represented by the middle third of a line drawn from the lower border of the tragus of the auricle to the midpoint of the philtrum of the upper lip.
Nerves
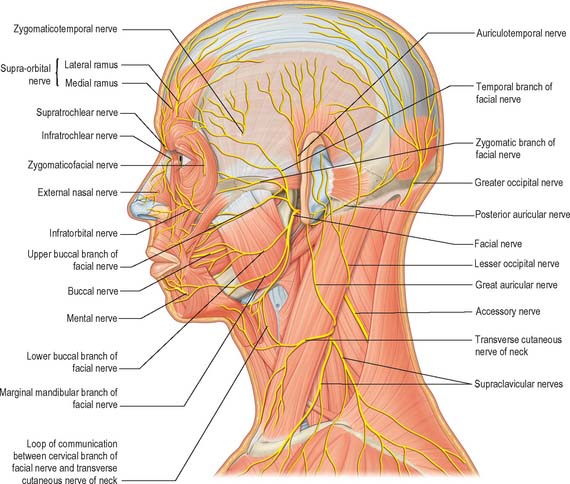
Facial nerve
The nerve exits the skull at the stylomastoid foramen and so is initially deep to the posterior margin of the external acoustic meatus: the nerve trunk lies approximately 1 cm deep and inferior to the tragal point. It usually divides within the substance of the parotid gland into superior (temporofacial) and inferior (cervicofacial) trunks which collectively give off five main peripheral branches that radiate out across the face (Fig. 25.10; see Fig. 29.17). Cadaveric and intra-operative microdissection studies have revealed that the distribution of the rami that are given off from these branches is highly variable: the use of surface anatomical coordinates alone to locate them is therefore unreliable, and can only give an approximation of their underlying trajectory. The course of the temporal branch(es) corresponds to a line extending anteriorly and superiorly from the attachment of the lobule (approximately 0.5 cm below the tragus) to a point 1.5 cm above the lateral aspect of the ipsilateral eyebrow. This branch is particularly vulnerable to damage as it runs over the zygomatic arch, and to a lesser extent in the lateral brow: it may be injured in facial rhytidectomy or with coronal or endoscopic brow lifting. The buccal branches have been described as running both above and below the parotid duct. The marginal mandibular nerve lies either along the body of the mandible (80%) or it may briefly enter the neck, where it lies within 1.2 cm of the lower border of the body (20%). Branches that enter the neck curve upwards and re-enter the face by crossing the lower border of the mandible at the anterior border of masseter. As they do so, they also cross the facial artery and vein. Incisions to access the submandibular region of the neck are therefore usually made at least 1.5 cm (two fingers’ breadth) below the lower border of the mandible in order to avoid damaging the marginal mandibular branch: injury results in ipsilateral paralysis of depressor anguli oris and depressor labii inferioris and produces a characteristic deformity.
Dermatomes
Our knowledge of the extent of individual dermatomes is largely based on clinical evidence. The dermatomes of the face arise mainly from cutaneous branches of the three major divisions of the trigeminal nerve (Fig. 25.10). The skin covering the front and sides of the neck, and over the angle of the mandible, and of the lateral scalp and posterior aspect of the pinna, is supplied by branches of the cervical plexus (C2–C4), and the skin over the back of the head is supplied by the greater occipital nerve (C2, posterior primary ramus) (see Fig. 25.10, and Figs 29.15 and 42.3).
SURFACE ANATOMY OF THE NECK
Soft tissues and viscera
Triangles of the neck
From the front and side the neck is obviously divided into anterior and posterior triangles by sternocleidomastoid (Fig. 25.11). In prosected cadaveric specimens, the anterior triangle may be further subdivided into submental, muscular, carotid and digastric triangles, and the posterior cervical triangle may be partitioned into occipital and supraclavicular triangles. It should be noted that the structures that form the boundaries of some of these lesser triangles are not readily palpable or visible.
Root of the neck
The root of the neck (Ch. 28) is the transitional zone between the neck, thorax and both upper limbs. It contains numerous important structures, including the oesophagus and trachea in the midline, and the apices of the lungs covered by apical pleura, the common carotid and subclavian arteries and the branches of the thyrocervical trunks, the internal jugular veins, the phrenic and vagus nerves and cervical sympathetic trunks, and the roots of the brachial plexus on both sides, and the terminations of the thoracic and right lymphatic ducts on the left and right sides respectively.
Course of vessels
Subclavian artery
The subclavian artery enters the root of the neck behind the sternoclavicular joint. It arches upwards to reach a point approximately 2 cm above the clavicle deep to the posterior border of sternocleidomastoid, and then passes across the upper surface of the first rib behind the middle region of the clavicle. The subclavian pulse may therefore be located behind the clavicle at the lateral border of sternocleidomastoid or where the artery crosses the first rib.
External jugular vein
The external jugular vein lies superficial to sternocleidomastoid and can be represented by a line which starts just below and behind the angle of the mandible and runs down to the clavicle near the posterior border of sternocleidomastoid (Fig. 25.3). It drains into the subclavian vein after penetrating the investing layer of deep cervical fascia and may be kinked at this point. If the proximal part of the vein is damaged it may be held open by the surrounding fascia: air can then be sucked in, resulting in an air embolus. The external jugular vein can be distended if venous pressure is raised, e.g. by performing Valsalva’s manoeuvre (forced expiration against a closed mouth and blocked nostrils) or by supraclavicular digital pressure.
Internal jugular vein
The internal jugular vein runs in the carotid sheath, lying just lateral to the arteries. It therefore has similar surface markings to those described for the common and internal carotid arteries and is represented in surface projection by a broad band from the lobule of the ear to the medial end of the clavicle, where it joins the subclavian vein. The inferior bulb of the internal jugular vein lies in the lesser supraclavicular fossa (the depression between the sternal and clavicular heads of sternocleidomastoid): this site is one of several at which the internal jugular vein may be accessed for central vein cannulation (see Ch. 28). The jugular venous pulse reflects the jugular venous pressure (central venous pressure) and is a measure of cardiac function. Pulsation of the great veins may be seen in this region if the central venous pressure is raised (e.g. right-sided heart failure). Internal jugular vein cannulation is described in Chapter 28.
Course of nerves
Spinal accessory nerve
The course of the spinal accessory nerve can be indicated by a line that crosses the floor of the posterior triangle passing from the junction of the upper third and middle thirds of the posterior border of sternocleidomastoid (Erb’s point; see Fig. 25.11) to the junction of the lower and middle thirds of the anterior border of trapezius. The course of the nerve may also be represented by a line joining the palpable transverse process of the atlas (approximately 1 cm below the mastoid process) to the anterior border of trapezius 5 cm above the clavicle.
Cervical plexus
The cutaneous branches of the cervical plexus emerge from behind the posterior border of sternocleidomastoid just below the spinal accessory nerve (Fig. 25.10).
Cervical sympathetic ganglia
The superior cervical ganglion lies slightly anterior to the (palpable) transverse process of the second cervical vertebra, while the middle cervical ganglion, when present, lies just in front of the transverse process of the sixth cervical vertebra (which is difficult to palpate). The inferior cervical ganglion may be fused with the first thoracic cervical ganglion, forming the stellate or cervicothoracic ganglion. Stellate ganglion block is often employed to perform a sympathetic nerve block to the head and neck, or to the arm: the surface marking is approximately at the level of the transverse process of the seventh cervical vertebra (situated two finger’s breadths above the sterno-clavicular joint when the neck is fully extended) (Ellis et al 1997).