Head and Neck
ADDITIONAL LEARNING RESOURCES for Chapter 8, Head and Neck, on STUDENT CONSULT (www.studentconsult.com):
Conceptual overview
General description
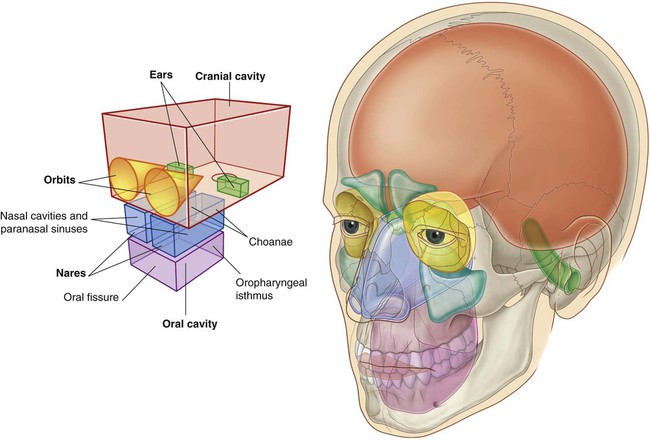
The head and neck are anatomically complex areas of the body.
Head
Other anatomically defined regions
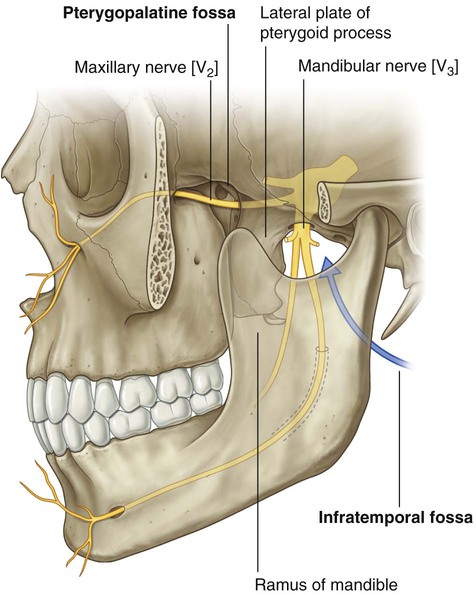
In addition to the major compartments of the head, two other anatomically defined regions (infratemporal fossa and pterygopalatine fossa) of the head on each side are areas of transition from one compartment of the head to another (Fig. 8.2). The face and scalp also are anatomically defined areas of the head and are related to external surfaces.
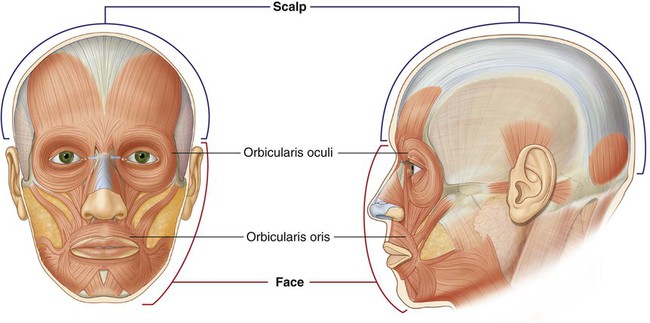
The face is the anterior aspect of the head and contains a unique group of muscles that move the skin relative to underlying bone and control the anterior openings to the orbits and oral cavity (Fig. 8.3).
The scalp covers the superior, posterior, and lateral regions of the head (Fig. 8.3).
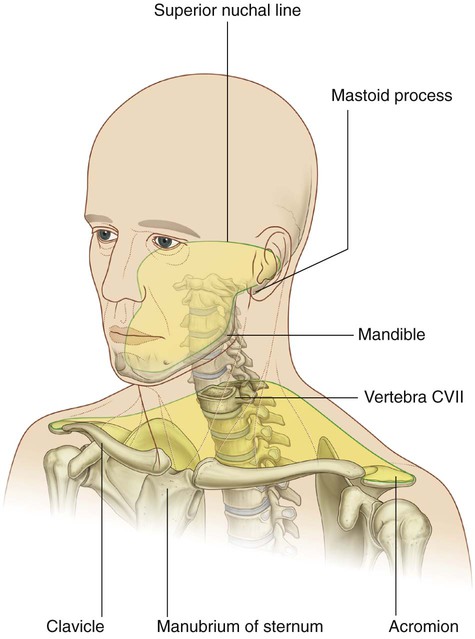
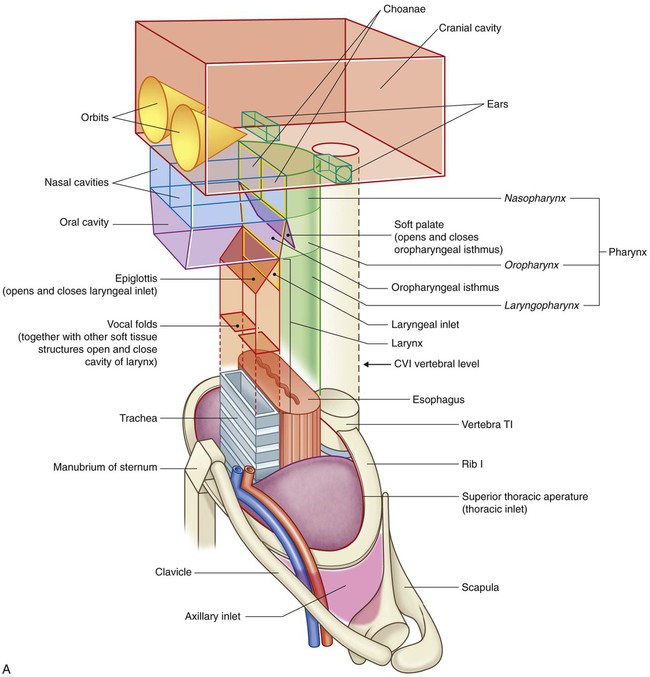
Neck
The neck extends from the head above to the shoulders and thorax below (Fig. 8.4). Its superior boundary is along the inferior margins of the mandible and bone features on the posterior aspect of the skull. The posterior neck is higher than the anterior neck to connect cervical viscera with the posterior openings of the nasal and oral cavities.
Compartments
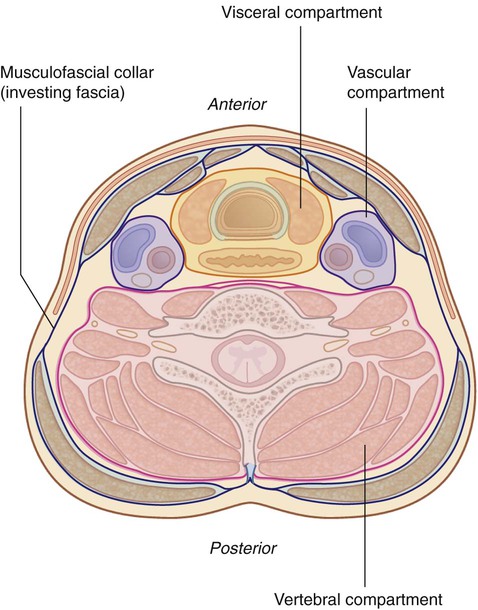
The neck has four major compartments (Fig. 8.5), which are enclosed by an outer musculofascial collar:
 The vertebral compartment contains the cervical vertebrae and associated postural muscles.
The vertebral compartment contains the cervical vertebrae and associated postural muscles.
 The visceral compartment contains important glands (thyroid, parathyroid, and thymus), and parts of the respiratory and digestive tracts that pass between the head and thorax.
The visceral compartment contains important glands (thyroid, parathyroid, and thymus), and parts of the respiratory and digestive tracts that pass between the head and thorax.
 The two vascular compartments, one on each side, contain the major blood vessels and the vagus nerve.
The two vascular compartments, one on each side, contain the major blood vessels and the vagus nerve.
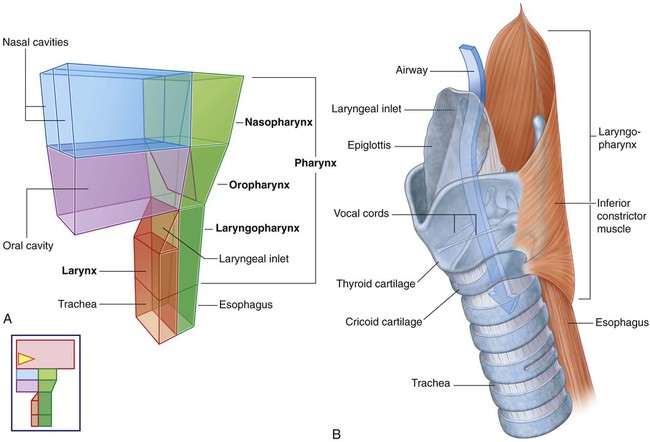
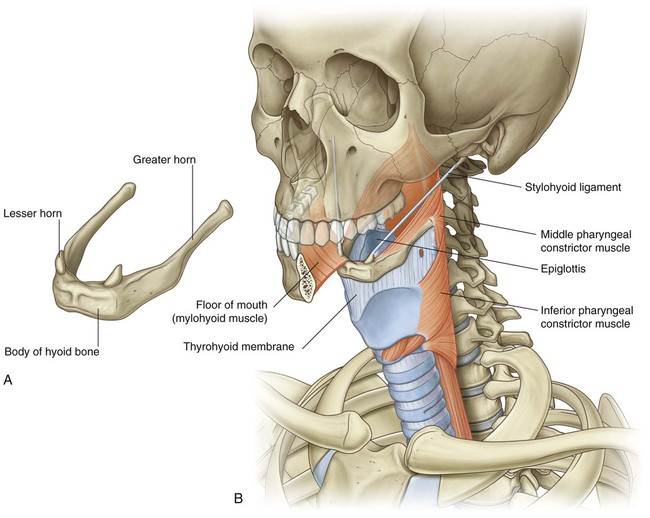
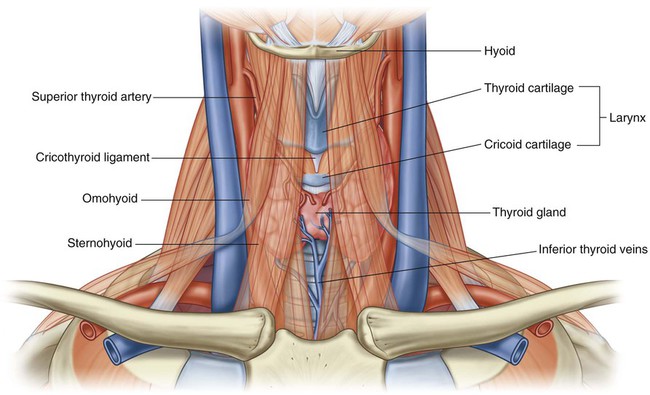
Larynx and pharynx
The larynx (Fig. 8.6) is the upper part of the lower airway and is attached below to the top of the trachea and above, by a flexible membrane, to the hyoid bone, which in turn is attached to the floor of the oral cavity. A number of cartilages form a supportive framework for the larynx, which has a hollow central channel. The dimensions of this central channel can be adjusted by soft tissue structures associated with the laryngeal wall. The most important of these are two lateral vocal folds, which project toward each other from adjacent sides of the laryngeal cavity. The upper opening of the larynx (laryngeal inlet) is tilted posteriorly, and is continuous with the pharynx.
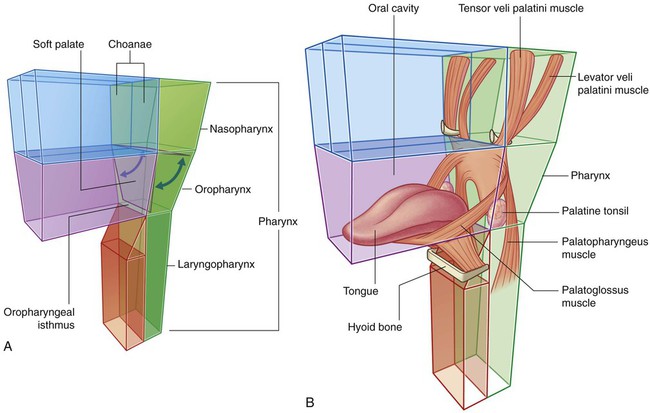
The pharynx (Fig. 8.6) is a chamber in the shape of a half-cylinder with walls formed by muscles and fascia. Above, the walls are attached to the base of the skull, and below to the margins of the esophagus. On each side, the walls are attached to the lateral margins of the nasal cavities, the oral cavity, and the larynx. The two nasal cavities, the oral cavity, and the larynx therefore open into the anterior aspect of the pharynx, and the esophagus opens inferiorly.
Component parts
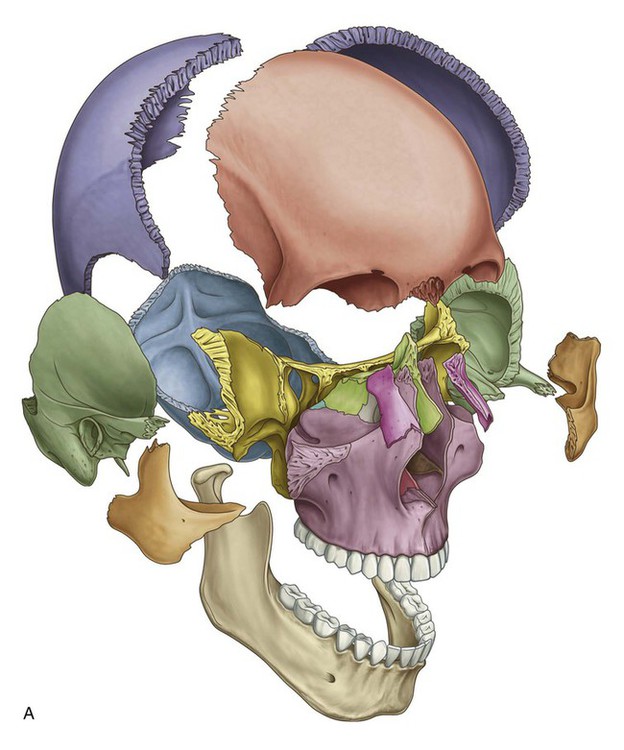
Skull
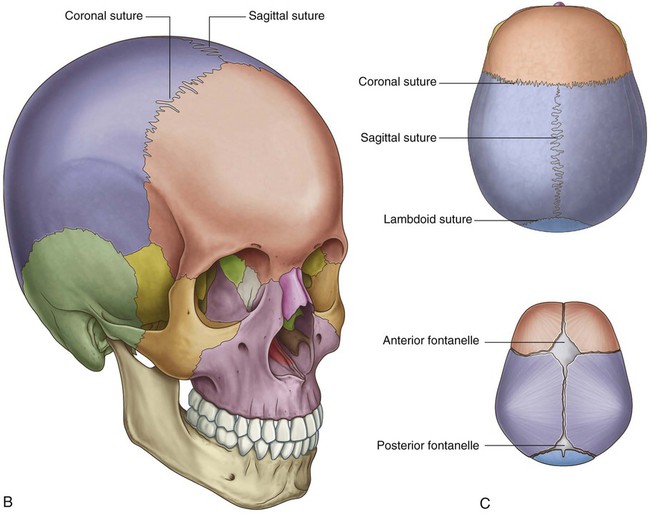
The many bones of the head collectively form the skull (Fig. 8.7A). Most of these bones are interconnected by sutures, which are immovable fibrous joints (Fig. 8.7B).
In the fetus and newborn, large membranous and unossified gaps (fontanelles) between the bones of the skull, particularly between the large flat bones that cover the top of the cranial cavity (Fig. 8.7C), allow:
Cervical vertebrae
The seven cervical vertebrae form the bony framework of the neck.
Cervical vertebrae (Fig. 8.8A) are characterized by:
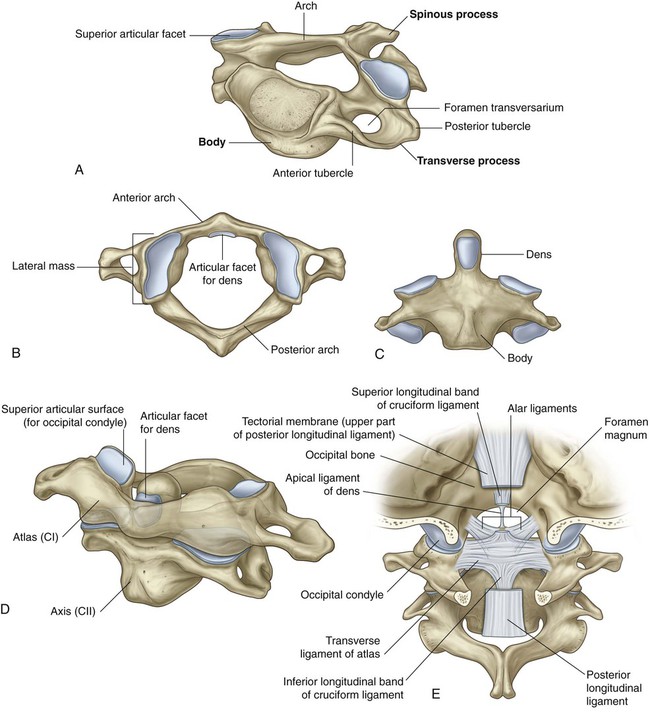
The upper two cervical vertebrae (CI and CII) are modified for moving the head (Fig. 8.8B–E; see also Chapter 2).
Hyoid bone
The hyoid bone is a small U-shaped bone (Fig. 8.9A) oriented in the horizontal plane just superior to the larynx, where it can be palpated and moved from side to side.
 The body of the hyoid bone is anterior and forms the base of the U.
The body of the hyoid bone is anterior and forms the base of the U.
 The two arms of the U (greater horns) project posteriorly from the lateral ends of the body.
The two arms of the U (greater horns) project posteriorly from the lateral ends of the body.
The hyoid bone does not articulate directly with any other skeletal elements in the head and neck.
Muscles
In the head
The muscle groups in the head include:
 the extra-ocular muscles (move the eyeball and open the upper eyelid),
the extra-ocular muscles (move the eyeball and open the upper eyelid),
 muscles of the middle ear (adjust the movement of the middle ear bones),
muscles of the middle ear (adjust the movement of the middle ear bones),
 muscles of facial expression (move the face),
muscles of facial expression (move the face),
 muscles of mastication (move the jaw—temporomandibular joint),
muscles of mastication (move the jaw—temporomandibular joint),
 muscles of the soft palate (elevate and depress the palate), and
muscles of the soft palate (elevate and depress the palate), and
 muscles of the tongue (move and change the contour of the tongue).
muscles of the tongue (move and change the contour of the tongue).
In the neck
In the neck, major muscle groups include:
 muscles of the pharynx (constrict and elevate the pharynx),
muscles of the pharynx (constrict and elevate the pharynx),
 muscles of the larynx (adjust the dimensions of the air pathway),
muscles of the larynx (adjust the dimensions of the air pathway),
 strap muscles (position the larynx and hyoid bone in the neck),
strap muscles (position the larynx and hyoid bone in the neck),
 muscles of the outer cervical collar (move the head and upper limb), and
muscles of the outer cervical collar (move the head and upper limb), and
 postural muscles in the muscular compartment of the neck (position the neck and head).
postural muscles in the muscular compartment of the neck (position the neck and head).
Relationship to other regions
Thorax
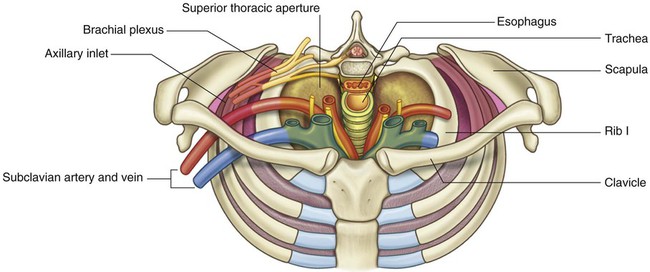
The superior thoracic aperture (thoracic inlet) opens directly into the base of the neck (Fig. 8.11). Structures passing between the head and thorax pass up and down through the superior thoracic aperture and the visceral compartment of the neck. At the base of the neck, the trachea is immediately anterior to the esophagus, which is directly anterior to the vertebral column. There are major veins, arteries, and nerves anterior and lateral to the trachea.
Key features
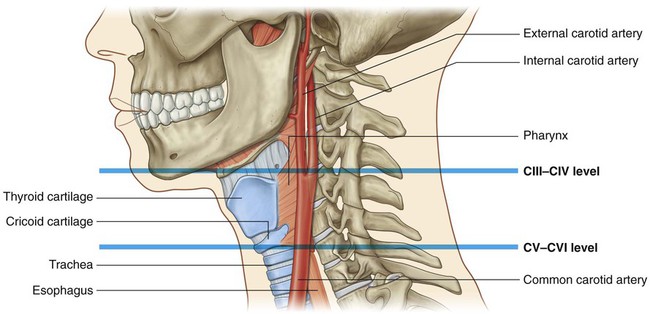
Vertebral levels CIII/IV and CV/VI
In the neck, the two important vertebral levels (Fig. 8.12) are:
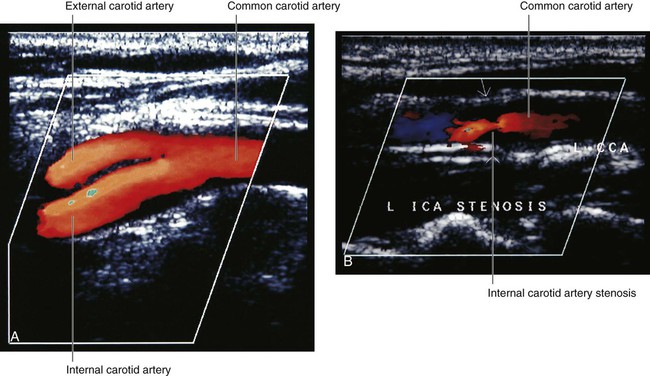
 between CIII and CIV, at approximately the superior border of the thyroid cartilage of the larynx (which can be palpated) and where the major artery on each side of the neck (the common carotid artery) bifurcates into internal and external carotid arteries; and
between CIII and CIV, at approximately the superior border of the thyroid cartilage of the larynx (which can be palpated) and where the major artery on each side of the neck (the common carotid artery) bifurcates into internal and external carotid arteries; and
 between CV and CVI, which marks the lower limit of the pharynx and larynx, and the superior limit of the trachea and esophagus—the indentation between the cricoid cartilage of the larynx and the first tracheal ring can be palpated.
between CV and CVI, which marks the lower limit of the pharynx and larynx, and the superior limit of the trachea and esophagus—the indentation between the cricoid cartilage of the larynx and the first tracheal ring can be palpated.
The internal carotid artery has no branches in the neck and ascends into the skull to supply much of the brain. It also supplies the eye and orbit. Other regions of the head and neck are supplied by branches of the external carotid artery.
Airway in the neck
The larynx (Fig. 8.13) and the trachea are anterior to the digestive tract in the neck, and can be accessed directly when upper parts of the system are blocked. A cricothyrotomy makes use of the easiest route of access through the cricothyroid ligament (cricovocal membrane, cricothyroid membrane) between the cricoid and thyroid cartilages of the larynx. The ligament can be palpated in the midline, and usually there are only small blood vessels, connective tissue, and skin (though occasionally, a small lobe of the thyroid gland—pyramidal lobe) overlying it. At a lower level, the airway can be accessed surgically through the anterior wall of the trachea by tracheostomy. This route of entry is complicated because large veins and part of the thyroid gland overlie this region.
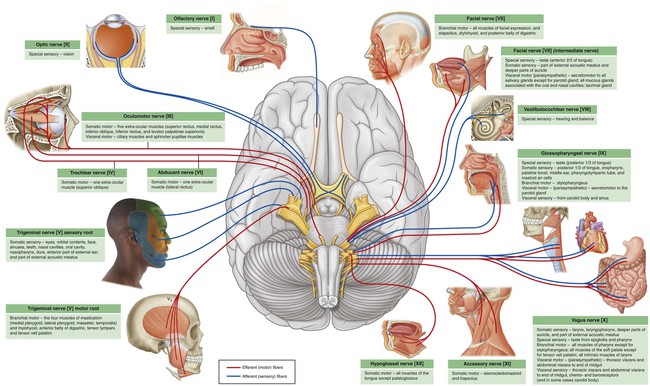
Cranial nerves
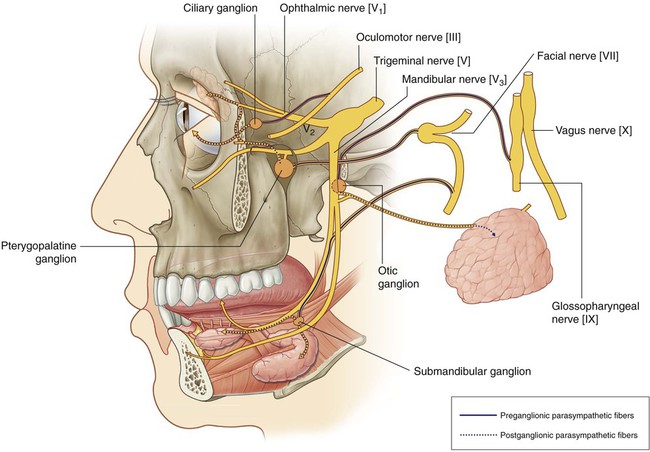
Parasympathetic fibers in the head are carried out of the brain as part of four cranial nerves—the oculomotor nerve [III], the facial nerve [VII], the glossopharyngeal nerve [IX], and the vagus nerve [X] (Fig. 8.14). Parasympathetic fibers in the oculomotor nerve [III], the facial nerve [VII], and the glossopharyngeal nerve [IX] destined for target tissues in the head leave these nerves, and are distributed with branches of the trigeminal nerve [V].
Cervical nerves
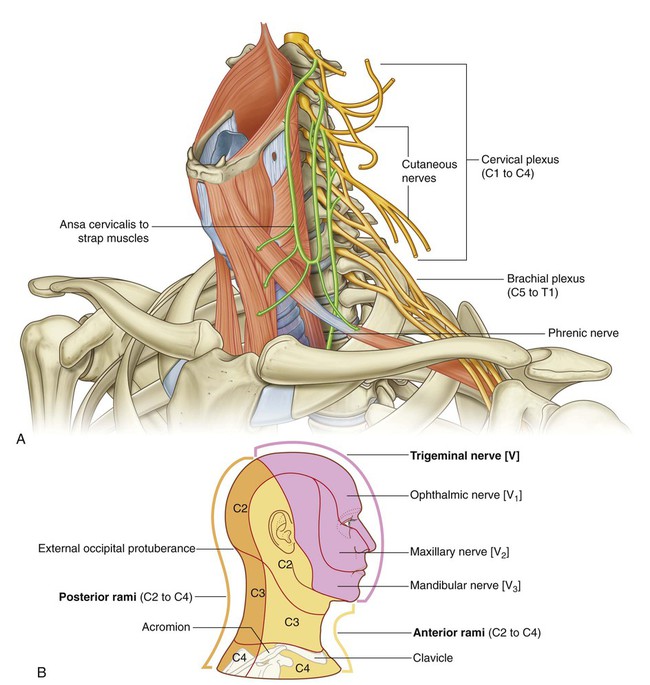
There are eight cervical nerves (C1 to C8):
The anterior rami of C1 to C4 form the cervical plexus. The major branches from this plexus supply the strap muscles, the diaphragm (phrenic nerve), skin on the anterior and lateral parts of the neck, skin on the upper anterior thoracic wall, and skin on the inferior parts of the head (Fig. 8.15B).
Functional separation of the digestive and respiratory passages
 The lower airway can be accessed through the oral cavity by intubation.
The lower airway can be accessed through the oral cavity by intubation.
 The digestive tract (esophagus) can be accessed through the nasal cavity by feeding tubes.
The digestive tract (esophagus) can be accessed through the nasal cavity by feeding tubes.
Normally, the soft palate, epiglottis, and soft tissue structures within the larynx act as valves to prevent food and liquid from entering lower parts of the respiratory tract (Fig. 8.16A).
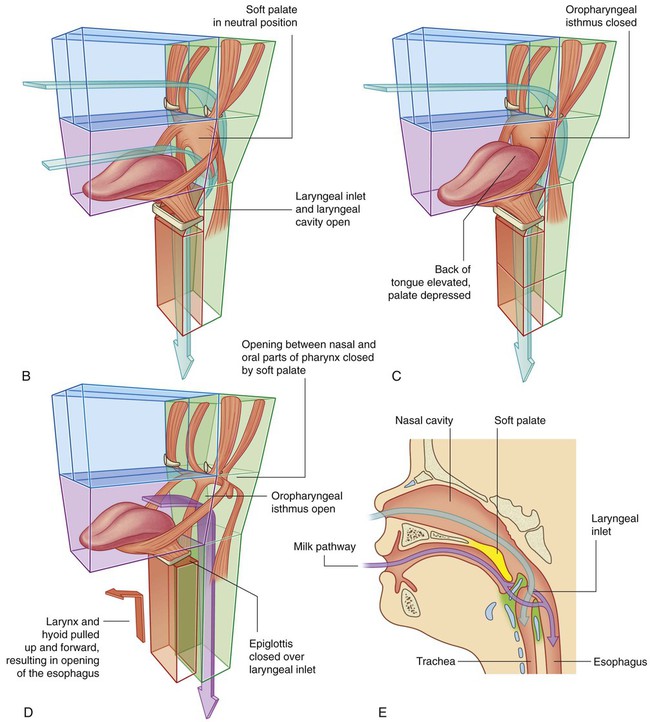
During normal breathing, the airway is open and air passes freely through the nasal cavities (or oral cavity), pharynx, larynx, and trachea (Fig. 8.16A). The lumen of the esophagus is normally closed because, unlike the airway, it has no skeletal support structures to hold it open.
When the oral cavity is full of liquid or food, the soft palate is swung down (depressed) to close the oropharyngeal isthmus, thereby allowing manipulation of food and fluid in the oral cavity while breathing (Fig. 8.16C).
When swallowing, the soft palate and parts of the larynx act as valves to ensure proper movement of food from the oral cavity into the esophagus (Fig. 8.16D).
In newborns, the larynx is high in the neck and the epiglottis is above the level of the soft palate (Fig. 8.16E). Babies can therefore suckle and breathe at the same time. Liquid flows around the larynx without any danger of entering the airway. During the second year of life, the larynx descends into the low cervical position characteristic of adults.
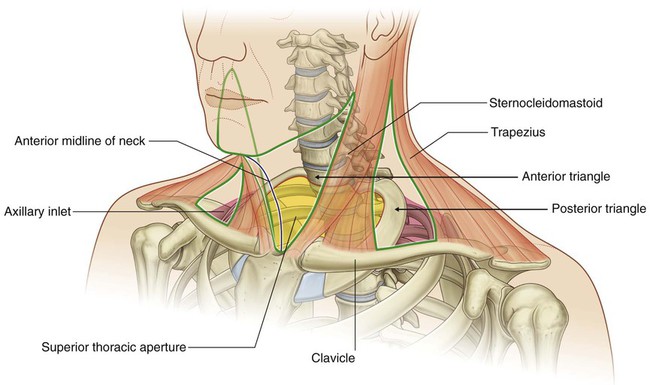
Triangles of the neck
The two muscles (trapezius and sternocleidomastoid) that form part of the outer cervical collar divide the neck into anterior and posterior triangles on each side (Fig. 8.17).
The boundaries of each anterior triangle are:
Regional anatomy
Skull
The cranium can be subdivided into:
 an upper domed part (the calvaria), which covers the cranial cavity containing the brain,
an upper domed part (the calvaria), which covers the cranial cavity containing the brain,
 a base that consists of the floor of the cranial cavity, and
a base that consists of the floor of the cranial cavity, and
The mandible is not part of the cranium nor part of the facial skeleton.
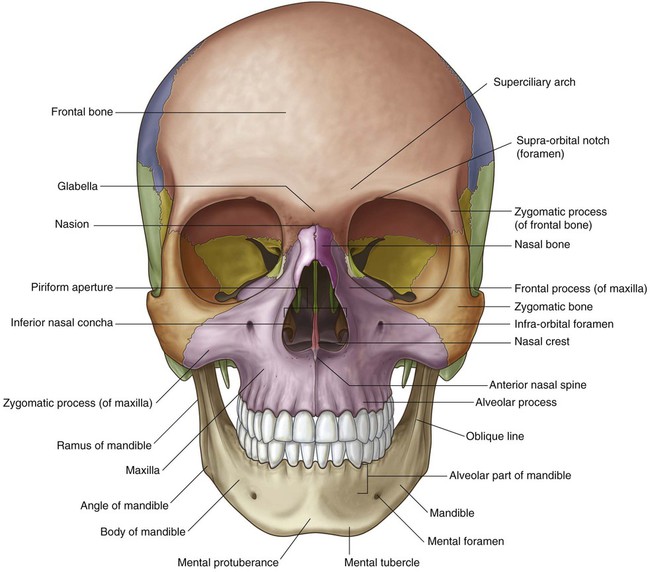
Anterior view
The anterior view of the skull includes the forehead superiorly, and, inferiorly, the orbits, the nasal region, the part of the face between the orbit and the upper jaw, the upper jaw, and the lower jaw (Fig. 8.18).
Frontal bone
The forehead consists of the frontal bone, which also forms the superior part of the rim of each orbit (Fig. 8.18).
Clearly visible in the medial part of the superior rim of each orbit is the supra-orbital foramen (supra-orbital notch; Table 8.1).
Table 8.1
External foramina of the skull
| Foramen | Structures passing through foramen |
| ANTERIOR VIEW | |
| Supra-orbital foramen | Supra-orbital nerve and vessels |
| Infra-orbital foramen | Infra-orbital nerve and vessels |
| Mental foramen | Mental nerve and vessels |
| LATERAL VIEW | |
| Zygomaticofacial foramen | Zygomaticofacial nerve |
| SUPERIOR VIEW | |
| Parietal foramen | Emissary veins |
| INFERIOR VIEW | |
| Incisive foramen | Nasopalatine nerve; sphenopalatine vessels |
| Greater palatine foramen | Greater palatine nerve and vessels |
| Lesser palatine foramen | Lesser palatine nerves and vessels |
| Pterygoid canal | Pterygoid nerve and vessels |
| Foramen ovale | Mandibular nerve [V3]; lesser petrosal nerve |
| Foramen spinosum | Middle meningeal artery |
| Foramen lacerum | Filled with cartilage |
| Carotid canal | Internal carotid artery and nerve plexus |
| Foramen magnum | Continuation of brain and spinal cord; vertebral arteries and nerve plexuses; anterior spinal artery; posterior spinal arteries; roots of accessory nerve [XI]; meninges |
| Condylar canal | Emissary veins |
| Hypoglossal canal | Hypoglossal nerve [XII] and vessels |
| Jugular foramen | Internal jugular vein; inferior petrosal sinus; glossopharyngeal nerve [IX]; vagus nerve [X]; accessory nerve [XI] |
| Stylomastoid foramen | Facial nerve [VII] |
Medially, the frontal bone projects inferiorly forming a part of the medial rim of the orbit.
Mandible
The body of the mandible is arbitrarily divided into two parts:
Laterally, a mental foramen (Table 8.1) is visible halfway between the upper border of the alveolar part of the mandible and the lower border of the base of the mandible. Continuing past this foramen is a ridge (the oblique line) passing from the front of the ramus onto the body of the mandible. The oblique line is a point of attachment for muscles that depress the lower lip.
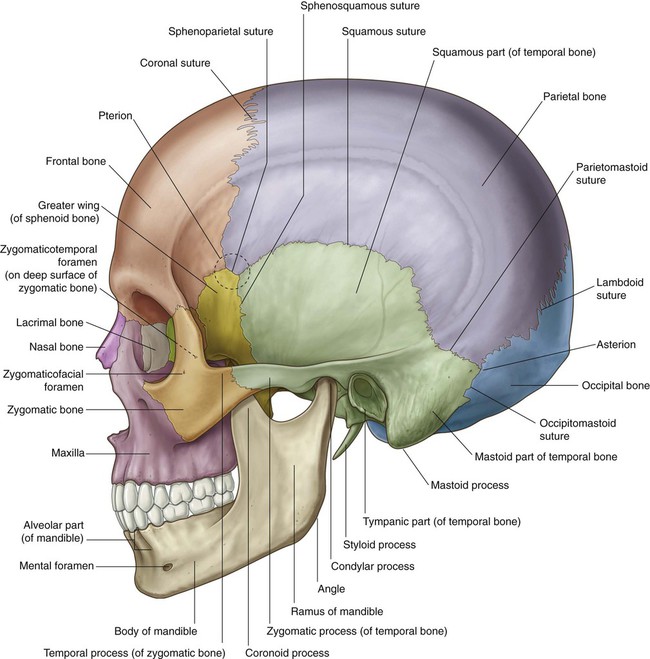
Lateral view
The lateral view of the skull consists of the lateral wall of the cranium, which includes lateral portions of the calvaria and the facial skeleton, and half of the lower jaw (Fig. 8.19):
 Bones forming the lateral portion of the calvaria include the frontal, parietal, occipital, sphenoid, and temporal bones.
Bones forming the lateral portion of the calvaria include the frontal, parietal, occipital, sphenoid, and temporal bones.
 Bones forming the visible part of the facial skeleton include the nasal, maxilla, and zygomatic bones.
Bones forming the visible part of the facial skeleton include the nasal, maxilla, and zygomatic bones.
Lateral portion of the calvaria
In lower parts of the lateral portion of the calvaria, the frontal bone articulates with the greater wing of the sphenoid bone (Fig. 8.19), which then articulates with the parietal bone at the sphenoparietal suture, and with the anterior edge of the temporal bone at the sphenosquamous suture.
Temporal bone
A major contributor to the lower portion of the lateral wall of the cranium is the temporal bone (Fig. 8.19), which consists of several parts:
 The squamous part has the appearance of a large flat plate, forms the anterior and superior parts of the temporal bone, contributes to the lateral wall of the cranium, and articulates anteriorly with the greater wing of the sphenoid bone at the sphenosquamous suture, and with the parietal bone superiorly at the squamous suture.
The squamous part has the appearance of a large flat plate, forms the anterior and superior parts of the temporal bone, contributes to the lateral wall of the cranium, and articulates anteriorly with the greater wing of the sphenoid bone at the sphenosquamous suture, and with the parietal bone superiorly at the squamous suture.
 The zygomatic process is an anterior bony projection from the lower surface of the squamous part of the temporal bone that initially projects laterally and then curves anteriorly to articulate with the temporal process of the zygomatic bone to form the zygomatic arch.
The zygomatic process is an anterior bony projection from the lower surface of the squamous part of the temporal bone that initially projects laterally and then curves anteriorly to articulate with the temporal process of the zygomatic bone to form the zygomatic arch.
 Immediately below the origin of the zygomatic process from the squamous part of the temporal bone is the tympanic part of the temporal bone, and clearly visible on the surface of this part is the external acoustic opening leading to the external acoustic meatus (ear canal).
Immediately below the origin of the zygomatic process from the squamous part of the temporal bone is the tympanic part of the temporal bone, and clearly visible on the surface of this part is the external acoustic opening leading to the external acoustic meatus (ear canal).
 The petromastoid part, which is usually separated into a petrous part and a mastoid part for descriptive purposes.
The petromastoid part, which is usually separated into a petrous part and a mastoid part for descriptive purposes.
Visible part of the facial skeleton
The bones of the viscerocranium visible in a lateral view of the skull include the nasal, maxilla, and zygomatic bones (Fig. 8.19) as follows:
 The maxilla with its alveolar process containing teeth forming the upper jaw; anteriorly, it articulates with the nasal bone; superiorly, it contributes to the formation of the inferior and medial borders of the orbit; medially, its frontal process articulates with the frontal bone; laterally, its zygomatic process articulates with the zygomatic bone.
The maxilla with its alveolar process containing teeth forming the upper jaw; anteriorly, it articulates with the nasal bone; superiorly, it contributes to the formation of the inferior and medial borders of the orbit; medially, its frontal process articulates with the frontal bone; laterally, its zygomatic process articulates with the zygomatic bone.
 The zygomatic bone, an irregularly shaped bone with a rounded lateral surface that forms the prominence of the cheek, is a visual centerpiece in this view— medially, it assists in the formation of the inferior rim of the orbit through its articulation with the zygomatic process of the maxilla; superiorly, its frontal process articulates with the zygomatic process of the frontal bone assisting in the formation of the lateral rim of the orbit; laterally, seen prominently in this view of the skull, the horizontal temporal process of the zygomatic bone projects backward to articulate with the zygomatic process of the temporal bone and so form the zygomatic arch.
The zygomatic bone, an irregularly shaped bone with a rounded lateral surface that forms the prominence of the cheek, is a visual centerpiece in this view— medially, it assists in the formation of the inferior rim of the orbit through its articulation with the zygomatic process of the maxilla; superiorly, its frontal process articulates with the zygomatic process of the frontal bone assisting in the formation of the lateral rim of the orbit; laterally, seen prominently in this view of the skull, the horizontal temporal process of the zygomatic bone projects backward to articulate with the zygomatic process of the temporal bone and so form the zygomatic arch.
Usually a small foramen (the zygomaticofacial foramen; Table 8.1) is visible on the lateral surface of the zygomatic bone. A zygomaticotemporal foramen is present on the medial deep surface of the bone.
Mandible
The final bony structure visible in a lateral view of the skull is the mandible. Inferiorly in the anterior part of this view, it consists of the anterior body of the mandible, a posterior ramus of the mandible, and the angle of the mandible where the inferior margin of the mandible meets the posterior margin of the ramus (Fig. 8.19).
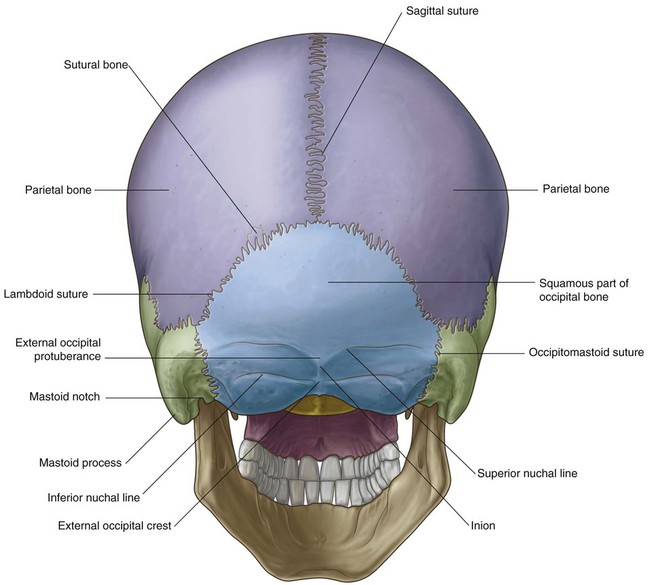
Posterior view
The occipital, parietal, and temporal bones are seen in the posterior view of the skull.
Occipital bone
Centrally the flat or squamous part of the occipital bone is the main structure in this view of the skull (Fig. 8.20). It articulates superiorly with the paired parietal bones at the lambdoid suture and laterally with each temporal bone at the occipitomastoid sutures. Along the lambdoid suture small islands of bone (sutural bones or wormian bones) may be observed.
Temporal bones
Laterally, the temporal bones are visible in the posterior view of the skull, with the mastoid processes being the prominent feature (Fig. 8.20). On the inferomedial border of each mastoid process is a notch (the mastoid notch), which is a point of attachment for the posterior belly of the digastric muscle.
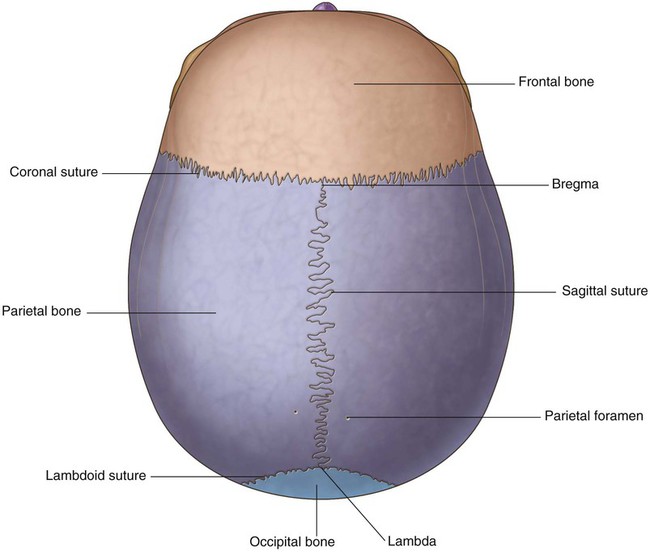
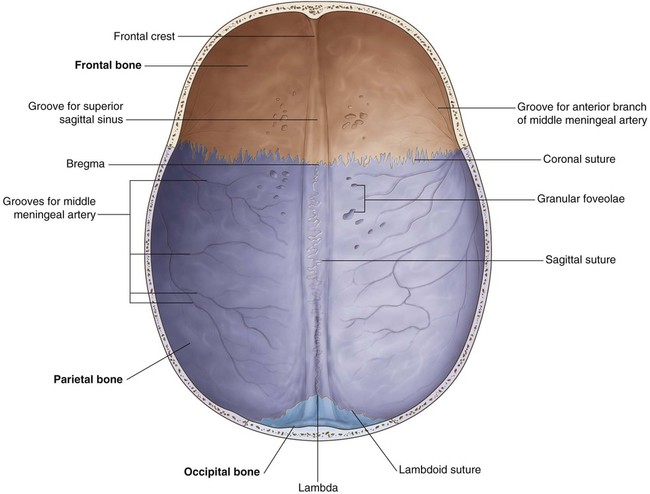
Superior view
The frontal bone, parietal bones, and occipital bone are seen in a superior view of the skull (Fig. 8.21). These bones make up the superior part of the calvaria or the calva (skullcap).
In an anterior to posterior direction:
 The unpaired frontal bone articulates with the paired parietal bones at the coronal suture.
The unpaired frontal bone articulates with the paired parietal bones at the coronal suture.
 The two parietal bones articulate with each other in the midline at the sagittal suture.
The two parietal bones articulate with each other in the midline at the sagittal suture.
 The parietal bones articulate with the unpaired occipital bone at the lambdoid suture.
The parietal bones articulate with the unpaired occipital bone at the lambdoid suture.
The only foramina visible in this view of the skull may be the paired parietal foramina, posteriorly, one on each parietal bone just lateral to the sagittal suture (Fig. 8.21).
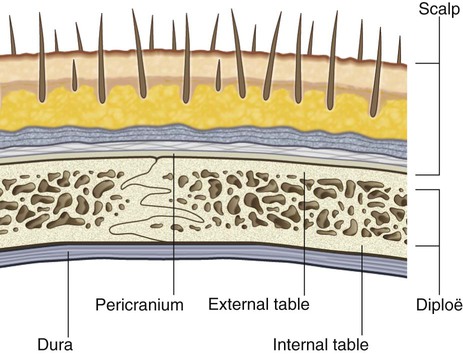
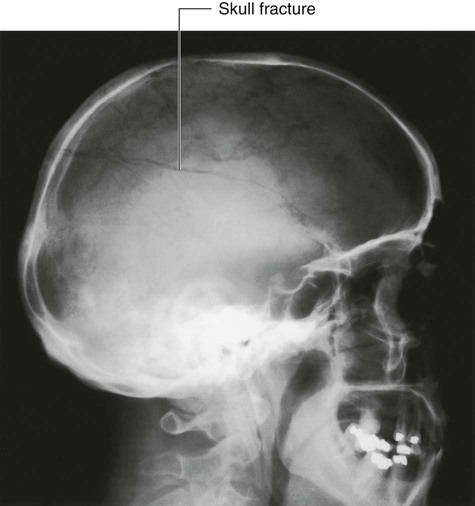
The bones making up the calvaria (Fig. 8.22) are unique in their structure, consisting of dense internal and external tables of compact bone separated by a layer of spongy bone (the diploë).
Inferior view
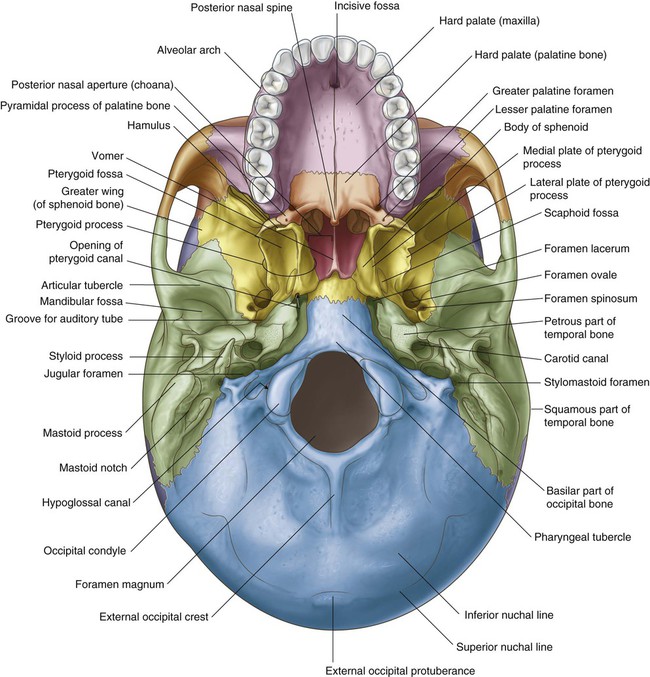
The base of the skull is seen in the inferior view and extends anteriorly from the middle incisor teeth posteriorly to the superior nuchal lines and laterally to the mastoid processes and zygomatic arches (Fig. 8.23).
For descriptive purposes the base of the skull is often divided into:
 an anterior part, which includes the teeth and the hard palate,
an anterior part, which includes the teeth and the hard palate,
 a middle part, which extends from behind the hard palate to the anterior margin of the foramen magnum, and
a middle part, which extends from behind the hard palate to the anterior margin of the foramen magnum, and
 a posterior part, which extends from the anterior edge of the foramen magnum to the superior nuchal lines.
a posterior part, which extends from the anterior edge of the foramen magnum to the superior nuchal lines.
Anterior part
The main features of the anterior part of the base of the skull are the teeth and the hard palate.
The teeth project from the alveolar processes of the two maxillae. These processes are together arranged in a U-shaped alveolar arch that borders the hard palate on three sides (Fig. 8.23).
Several additional features are also visible when the hard palate is examined:
 the incisive fossa in the anterior midline immediately posterior to the teeth, the walls of which contain incisive foramina (the openings of the incisive canals, which are passageways between the hard palate and nasal cavity);
the incisive fossa in the anterior midline immediately posterior to the teeth, the walls of which contain incisive foramina (the openings of the incisive canals, which are passageways between the hard palate and nasal cavity);
 the greater palatine foramina near the posterolateral border of the hard palate on each side, which lead to greater palatine canals;
the greater palatine foramina near the posterolateral border of the hard palate on each side, which lead to greater palatine canals;
 just posterior to the greater palatine foramina, the lesser palatine foramina in the pyramidal process of each palatine bone, which lead to lesser palatine canals;
just posterior to the greater palatine foramina, the lesser palatine foramina in the pyramidal process of each palatine bone, which lead to lesser palatine canals;
 a midline pointed projection (the posterior nasal spine) in the free posterior border of the hard palate.
a midline pointed projection (the posterior nasal spine) in the free posterior border of the hard palate.
Middle part
The middle part of the base of the skull is complex:
 Forming the anterior half are the vomer and sphenoid bones.
Forming the anterior half are the vomer and sphenoid bones.
 Forming the posterior half are the occipital and paired temporal bones.
Forming the posterior half are the occipital and paired temporal bones.
Anterior half
Most of the anterior part of the middle part of the base of the skull consists of the sphenoid bone.
Three parts of the sphenoid bone, the body, greater wings, and pterygoid processes, are seen in the inferior view of the skull (Fig. 8.23). The lesser wing of the sphenoid is not seen in the inferior view.
Lateral to the lateral plate of the pterygoid process is the greater wing of the sphenoid (Fig. 8.23), which not only forms a part of the base of the skull but also continues laterally to form part of the lateral wall of the skull. It articulates laterally and posteriorly with parts of the temporal bone.
Posterior half
In the posterior half of the middle part of the base of the skull are the occipital bone and the paired temporal bones (Fig. 8.23).
Wedge-shaped in its appearance, with its apex anteromedial, the petrous part of the temporal bone is between the greater wing of the sphenoid anteriorly and the basilar part of the occipital bone posteriorly. The apex forms one of the boundaries of the foramen lacerum, an irregular opening filled in life with cartilage (Fig. 8.23).
Just lateral to the greater wing of the sphenoid is the squamous part of the temporal bone, which participates in the temporomandibular joint. It contains the mandibular fossa, which is a concavity where the head of the mandible articulates with the base of the skull. An important feature of this articulation is the prominent articular tubercle, which is the downward projection of the anterior border of the mandibular fossa (Fig. 8.23).
Posterior part
The posterior part of the base of the skull extends from the anterior edge of the foramen magnum posteriorly to the superior nuchal lines (Fig. 8.23). It consists of parts of the occipital bone centrally and the temporal bones laterally.
Occipital bone
The occipital bone is the major bony element of this part of the base of the skull (Fig. 8.23). It has four parts organized around the foramen magnum, which is a prominent feature of this part of the base of the skull and through which the brain and spinal cord are continuous.
The parts of the occipital bone are the squamous part, which is posterior to the foramen magnum, the lateral parts, which are lateral to the foramen magnum, and the basilar part, which is anterior to the foramen magnum (Fig. 8.23).
The squamous and lateral parts are components of the posterior part of the base of the skull.
On each anterolateral border of the foramen magnum are the rounded occipital condyles (Fig. 8.23). These paired structures articulate with the atlas (vertebra CI). Posterior to each condyle is a depression (the condylar fossa) containing a condylar canal, and anterior and superior to each condyle is the large hypoglossal canal. Lateral to each hypoglossal canal is a large, irregular jugular foramen formed by opposition of the jugular notch of the occipital bone and jugular notch of the temporal bone.
Temporal bone
Laterally in the posterior part of the base of the skull is the temporal bone. The parts of the temporal bone seen in this location are the mastoid part of the petromastoid part and the styloid process (Fig. 8.23).
Finally, between the styloid process and the mastoid process is the stylomastoid foramen.
Cranial cavity
Roof
The calvaria is the dome-shaped roof that protects the superior aspect of the brain. It consists mainly of the frontal bone anteriorly, the paired parietal bones in the middle, and the occipital bone posteriorly (Fig. 8.24).
Sutures visible internally include:
 the coronal suture, between the frontal and parietal bones,
the coronal suture, between the frontal and parietal bones,
 the sagittal suture, between the paired parietal bones, and
the sagittal suture, between the paired parietal bones, and
 the lambdoid suture, between the parietal and occipital bones.
the lambdoid suture, between the parietal and occipital bones.
From anterior to posterior, features seen on the bony roof of the cranial cavity are:
 a midline ridge of bone extending from the surface of the frontal bone (the frontal crest), which is a point of attachment for the falx cerebri (a specialization of the dura mater that partially separates the two cerebral hemispheres);
a midline ridge of bone extending from the surface of the frontal bone (the frontal crest), which is a point of attachment for the falx cerebri (a specialization of the dura mater that partially separates the two cerebral hemispheres);
 at the superior point of the termination of the frontal crest the beginning of the groove for the superior sagittal sinus, which widens and deepens posteriorly and marks the position of the superior sagittal sinus (an intradural venous structure);
at the superior point of the termination of the frontal crest the beginning of the groove for the superior sagittal sinus, which widens and deepens posteriorly and marks the position of the superior sagittal sinus (an intradural venous structure);
 on either side of the groove for the superior sagittal sinus throughout its course, a small number of depressions and pits (the granular foveolae), which mark the location of arachnoid granulations (prominent structures readily identifiable when a brain with its meningeal coverings is examined; the arachnoid granulations are involved in the reabsorption of cerebrospinal fluid); and
on either side of the groove for the superior sagittal sinus throughout its course, a small number of depressions and pits (the granular foveolae), which mark the location of arachnoid granulations (prominent structures readily identifiable when a brain with its meningeal coverings is examined; the arachnoid granulations are involved in the reabsorption of cerebrospinal fluid); and
 on the lateral aspects of the roof of the cranial cavity, smaller grooves created by various meningeal vessels.
on the lateral aspects of the roof of the cranial cavity, smaller grooves created by various meningeal vessels.
Floor
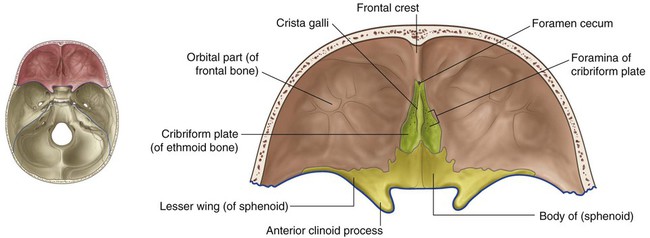
The floor of the cranial cavity is divided into anterior, middle, and posterior cranial fossae.
Anterior cranial fossa
Parts of the frontal, ethmoid, and sphenoid bones form the anterior cranial fossa (Fig. 8.25). Its floor is composed of:
 frontal bone in the anterior and lateral direction,
frontal bone in the anterior and lateral direction,
 ethmoid bone in the midline, and
ethmoid bone in the midline, and
 two parts of the sphenoid bone posteriorly, the body (midline) and the lesser wings (laterally).
two parts of the sphenoid bone posteriorly, the body (midline) and the lesser wings (laterally).
Anteriorly, a small wedge-shaped midline crest of bone (the frontal crest) projects from the frontal bone. This is a point of attachment for the falx cerebri. Immediately posterior to the frontal crest is the foramen cecum (Table 8.2). This foramen between the frontal and ethmoid bones may transmit emissary veins connecting the nasal cavity with the superior sagittal sinus.
Table 8.2
Internal foramina of the skull
| Foramen | Structures passing through foramen |
| ANTERIOR CRANIAL FOSSA | |
| Foramen cecum | Emissary veins to nasal cavity |
| Olfactory foramen in cribriform plate | Olfactory nerves [I] |
| MIDDLE CRANIAL FOSSA | |
| Optic canal | Optic nerve [II]; ophthalmic artery |
| Superior orbital fissure | Oculomotor nerve [III]; trochlear nerve [IV]; ophthalmic division of the trigeminal nerve [V1]; abducent nerve [VI]; ophthalmic veins |
| Foramen rotundum | Maxillary division of the trigeminal nerve [V2] |
| Foramen ovale | Mandibular division of the trigeminal nerve [V3]; lesser petrosal nerve |
| Foramen spinosum | Middle meningeal artery |
| Hiatus for the greater petrosal nerve | Greater petrosal nerve |
| Hiatus for the lesser petrosal nerve | Lesser petrosal nerve |
| POSTERIOR CRANIAL FOSSA | |
| Foramen magnum | End of brainstem/beginning of spinal cord; vertebral arteries; spinal roots of the accessory nerve; meninges |
| Internal acoustic meatus | Facial nerve [VII]; vestibulocochlear nerve [VIII]; labyrinthine artery |
| Jugular foramen | Glossopharyngeal nerve [IX]; vagus nerve [X]; accessory nerve [XI]; inferior petrosal sinus, sigmoid sinus (forming internal jugular vein) |
| Hypoglossal canal | Hypoglossal nerve [XII]; meningeal branch of the ascending pharyngeal artery |
| Condylar canal | Emissary vein |
Lateral to the crista galli is the cribriform plate of the ethmoid bone (Fig. 8.25). This is a sieve-like structure, which allows small olfactory nerve fibers to pass through its foramina from the nasal mucosa to the olfactory bulb. The olfactory nerves are commonly referred to collectively as the olfactory nerve [I].
Lesser wings of the sphenoid
Medially each lesser wing widens, curves posteriorly, and ends as a rounded anterior clinoid process (Fig. 8.25). These processes serve as the anterior point of attachment for the tentorium cerebelli, which is a sheet of dura that separates the posterior part of the cerebral hemispheres from the cerebellum. Just anterior to each anterior clinoid process is a circular opening in the lesser wing of the sphenoid (the optic canal), through which the ophthalmic artery and optic nerve [II] pass as they exit the cranial cavity to enter the orbit. The optic canals are usually included in the middle cranial fossa.
Middle cranial fossa
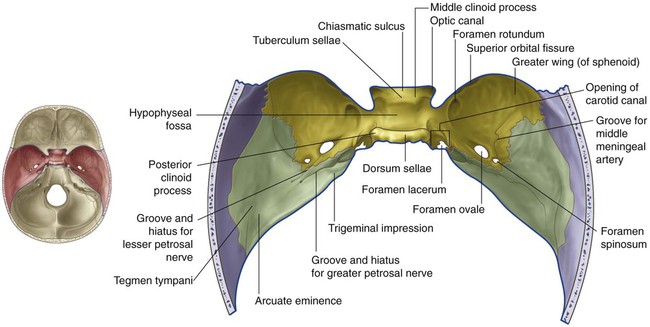
The middle cranial fossa consists of parts of the sphenoid and temporal bones (Fig. 8.26).
Sphenoid
Lateral to each side of the body of the sphenoid, the floor of the middle cranial fossa is formed on either side by the greater wing of the sphenoid (Fig. 8.26).
Posterolateral from the foramen ovale is the small foramen spinosum (Fig. 8.26). This opening also connects the infratemporal fossa with the middle cranial fossa. The middle meningeal artery and its associated veins pass through this foramen and, once inside, the groove for the middle meningeal artery across the floor and lateral wall of the middle cranial fossa clearly marks their path.
Posteromedial to the foramen ovale is the rounded intracranial opening of the carotid canal. Directly inferior to this opening is an irregular foramen (the foramen lacerum) (Fig. 8.26). Clearly observed in the inferior view of the skull, the foramen lacerum is closed in life by a cartilaginous plug, and no structures pass through it completely.
Temporal bone
Medially, there is a slight depression (trigeminal impression) in the anterior surface of the petrous part of the temporal bone (Fig. 8.26), which marks the location of the sensory ganglion for the trigeminal nerve [V].
Anterolateral to the groove for the greater petrosal nerve is a second, smaller groove and hiatus for the lesser petrosal nerve, a branch from the tympanic plexus carrying fibers that originally came from the glossopharyngeal nerve [IX] (Fig. 8.26).
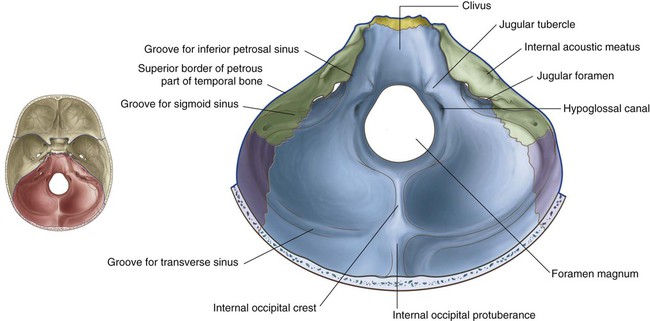
Posterior cranial fossa
The posterior cranial fossa consists mostly of parts of the temporal and occipital bones, with small contributions from the sphenoid and parietal bones (Fig. 8.27). It is the largest and deepest of the three cranial fossae and contains the brainstem (midbrain, pons, and medulla) and the cerebellum.
Boundaries
The anterior boundaries of the posterior cranial fossa in the midline are the dorsum sellae and the clivus (Fig. 8.27). The clivus is a slope of bone that extends upward from the foramen magnum. It is formed by contributions from the body of the sphenoid and from the basilar part of the occipital bone.
Grooves and foramina
The clivus slopes upward from the foramen magnum. Lateral to the clivus is a groove for the inferior petrosal sinus between the basilar part of the occipital bone and the petrous part of the petromastoid part of the temporal bone (Fig. 8.27).
Inferior to the internal acoustic meatus the temporal bone is separated from the occipital bone by the large jugular foramen (Fig. 8.27). Leading to this foramen from the medial side is the groove for the inferior petrosal sinus, and from the lateral side the groove for the sigmoid sinus.
Squamous part of the occipital bone
The squamous part of the occipital bone has several prominent features (Fig. 8.27):
 Running upward in the midline from the foramen magnum is the internal occipital crest.
Running upward in the midline from the foramen magnum is the internal occipital crest.
 On either side of the internal occipital crest, the floor of the posterior cranial fossa is concave to accommodate the cerebellar hemispheres.
On either side of the internal occipital crest, the floor of the posterior cranial fossa is concave to accommodate the cerebellar hemispheres.
 The internal occipital crest ends superiorly in a bony prominence (the internal occipital protuberance).
The internal occipital crest ends superiorly in a bony prominence (the internal occipital protuberance).
 Extending laterally from the internal occipital protuberance are grooves produced by the transverse sinuses, which continue laterally, eventually joining a groove for each sigmoid sinus—each of these grooves then turns inferiorly toward the jugular foramina.
Extending laterally from the internal occipital protuberance are grooves produced by the transverse sinuses, which continue laterally, eventually joining a groove for each sigmoid sinus—each of these grooves then turns inferiorly toward the jugular foramina.
The transverse and sigmoid sinuses are intradural venous sinuses.
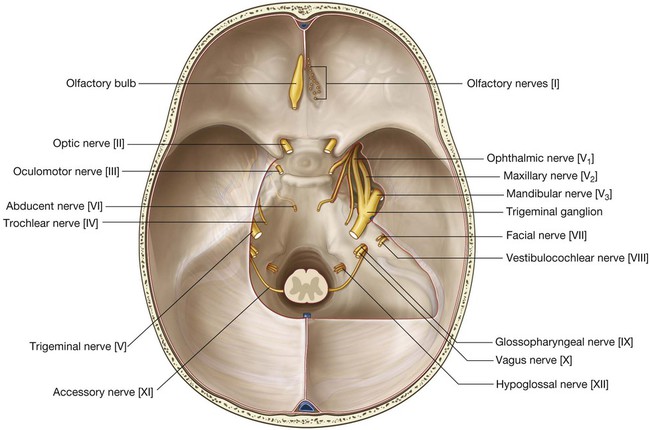
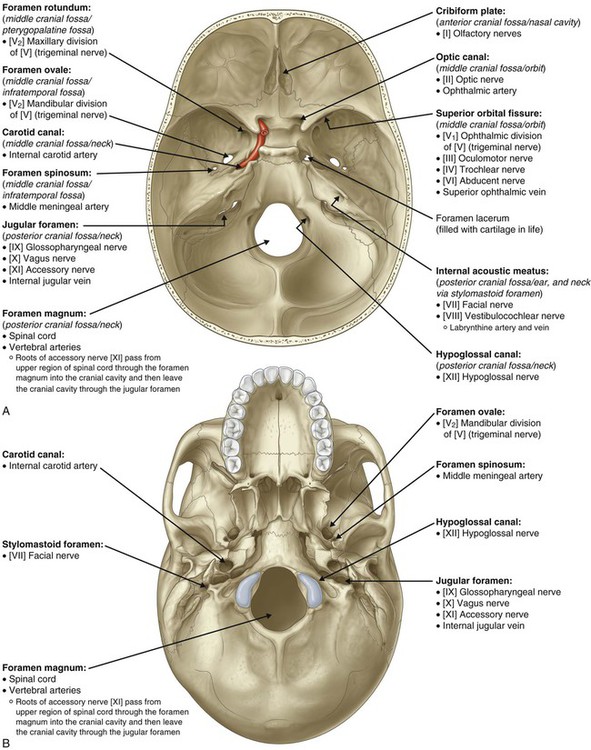
Foramina and fissures through which major structures enter and leave the cranial cavity
Foramina and fissures through which major structures pass between the cranial cavity and other regions are summarized in Fig. 8.28.
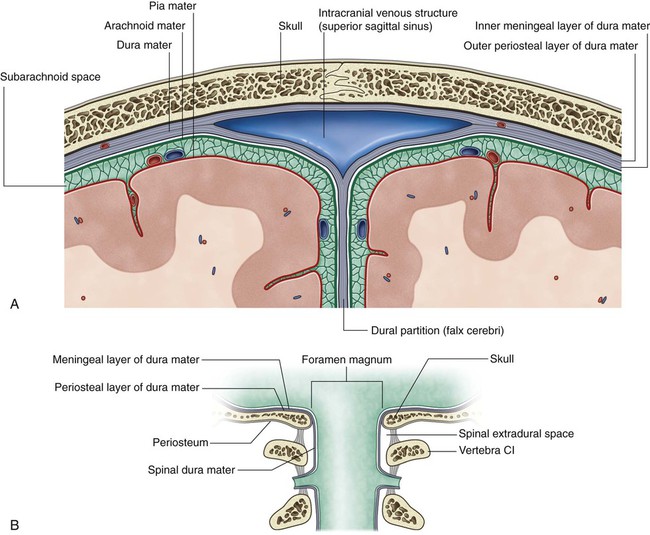
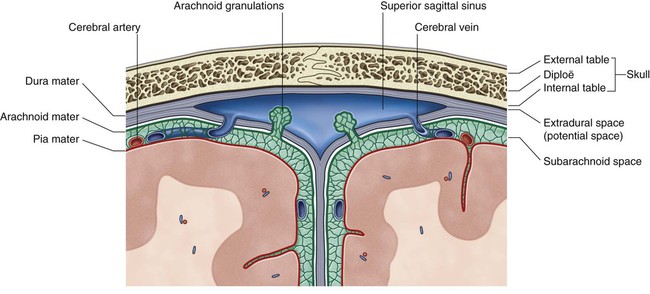
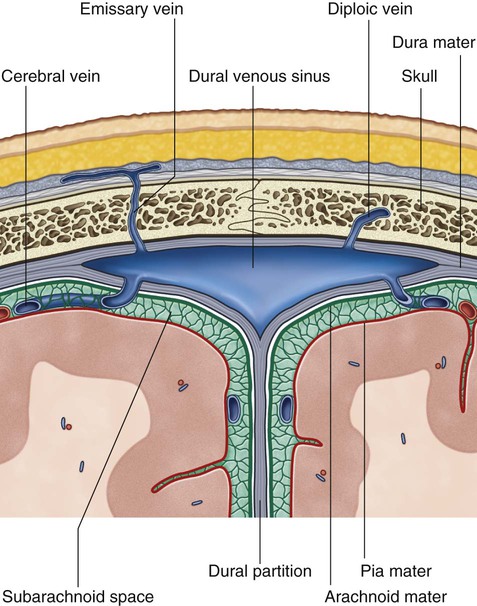
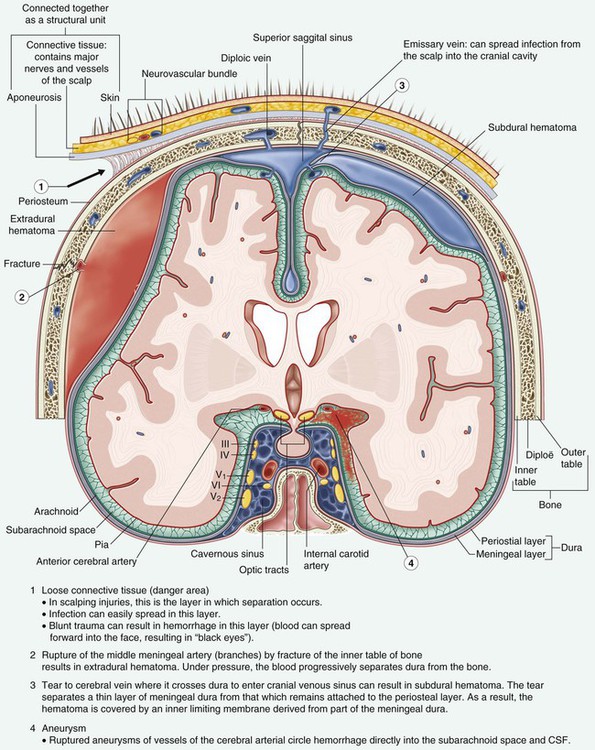
Meninges
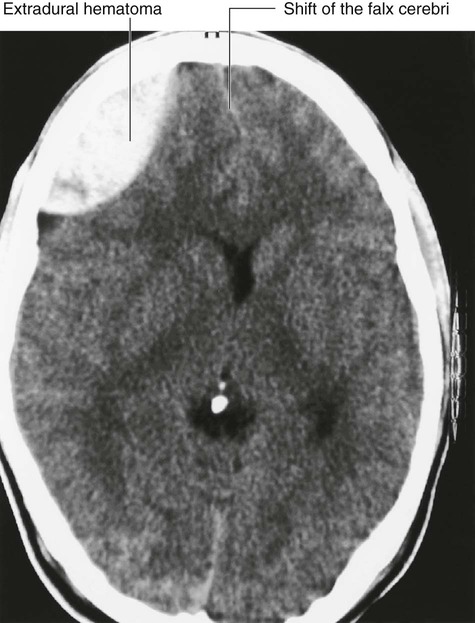
The brain, as well as the spinal cord, is surrounded by three layers of membranes (the meninges, Fig. 8.31A)—a tough, outer layer (the dura mater), a delicate, middle layer (the arachnoid mater), and an inner layer firmly attached to the surface of the brain (the pia mater).
The cranial meninges are continuous with, and similar to, the spinal meninges through the foramen magnum, with one important distinction—the cranial dura mater consists of two layers, and only one of these is continuous through the foramen magnum (Fig. 8.31B).
Cranial dura mater
The cranial dura mater is a thick, tough, outer covering of the brain. It consists of an outer periosteal layer and an inner meningeal layer (Fig. 8.31A):
 The outer periosteal layer is firmly attached to the skull, is the periosteum of the cranial cavity, contains the meningeal arteries, and is continuous with the periosteum on the outer surface of the skull at the foramen magnum and other intracranial foramina (Fig. 8.31B).
The outer periosteal layer is firmly attached to the skull, is the periosteum of the cranial cavity, contains the meningeal arteries, and is continuous with the periosteum on the outer surface of the skull at the foramen magnum and other intracranial foramina (Fig. 8.31B).
 The inner meningeal layer is in close contact with the arachnoid mater and is continuous with the spinal dura mater through the foramen magnum.
The inner meningeal layer is in close contact with the arachnoid mater and is continuous with the spinal dura mater through the foramen magnum.
The two layers of dura separate from each other at numerous locations to form two unique types of structures (Fig. 8.31A):
Dural partitions
Falx cerebri
The falx cerebri (Fig. 8.32) is a crescent-shaped downward projection of meningeal dura mater from the dura lining the calva that passes between the two cerebral hemispheres. It is attached anteriorly to the crista galli of the ethmoid bone and frontal crest of the frontal bone. Posteriorly it is attached to and blends with the tentorium cerebelli.
Tentorium cerebelli
The tentorium cerebelli (Fig. 8.32) is a horizontal projection of the meningeal dura mater that covers and separates the cerebellum in the posterior cranial fossa from the posterior parts of the cerebral hemispheres. It is attached posteriorly to the occipital bone along the grooves for the transverse sinuses. Laterally, it is attached to the superior border of the petrous part of the temporal bone, ending anteriorly at the anterior and posterior clinoid processes.
Falx cerebelli
The falx cerebelli (Fig. 8.32) is a small midline projection of meningeal dura mater in the posterior cranial fossa. It is attached posteriorly to the internal occipital crest of the occipital bone and superiorly to the tentorium cerebelli. Its anterior edge is free and is between the two cerebellar hemispheres.
Diaphragma sellae
The final dural projection is the diaphragma sellae (Fig. 8.32). This small horizontal shelf of meningeal dura mater covers the hypophyseal fossa in the sella turcica of the sphenoid bone. There is an opening in the center of the diaphragma sellae through which passes the infundibulum, connecting the pituitary gland with the base of the brain, and any accompanying blood vessels.
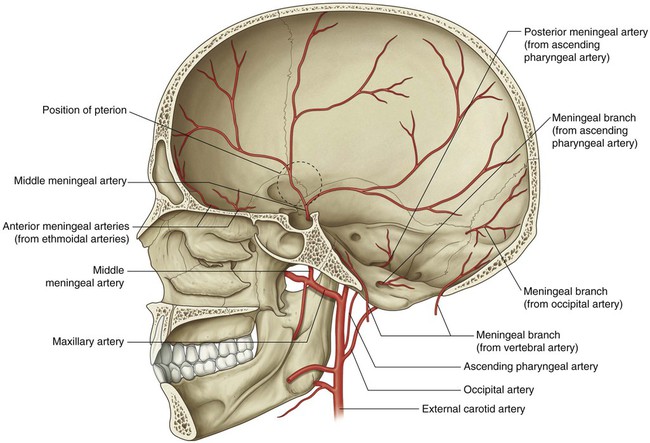
Arterial supply
The arterial supply to the dura mater (Fig. 8.33) travels in the outer periosteal layer of the dura and consists of:
 anterior meningeal arteries in the anterior cranial fossa,
anterior meningeal arteries in the anterior cranial fossa,
 the middle and accessory meningeal arteries in the middle cranial fossa, and
the middle and accessory meningeal arteries in the middle cranial fossa, and
 the posterior meningeal artery and other meningeal branches in the posterior cranial fossa.
the posterior meningeal artery and other meningeal branches in the posterior cranial fossa.
The anterior meningeal arteries are branches of the ethmoidal arteries.
 The anterior branch passes in an almost vertical direction to reach the vertex of the skull, crossing the pterion during its course.
The anterior branch passes in an almost vertical direction to reach the vertex of the skull, crossing the pterion during its course.
 The posterior branch passes in a posterosuperior direction, supplying this region of the middle cranial fossa.
The posterior branch passes in a posterosuperior direction, supplying this region of the middle cranial fossa.
The posterior meningeal artery and other meningeal branches supplying the dura mater in the posterior cranial fossa come from several sources (Fig. 8.33):
 The posterior meningeal artery, the terminal branch of the ascending pharyngeal artery, enters the posterior cranial fossa through the jugular foramen.
The posterior meningeal artery, the terminal branch of the ascending pharyngeal artery, enters the posterior cranial fossa through the jugular foramen.
 A meningeal branch from the ascending pharyngeal artery enters the posterior cranial fossa through the hypoglossal canal.
A meningeal branch from the ascending pharyngeal artery enters the posterior cranial fossa through the hypoglossal canal.
 Meningeal branches from the occipital artery enter the posterior cranial fossa through the jugular foramen and the mastoid foramen.
Meningeal branches from the occipital artery enter the posterior cranial fossa through the jugular foramen and the mastoid foramen.
 A meningeal branch from the vertebral artery arises as the vertebral artery enters the posterior cranial fossa through the foramen magnum.
A meningeal branch from the vertebral artery arises as the vertebral artery enters the posterior cranial fossa through the foramen magnum.
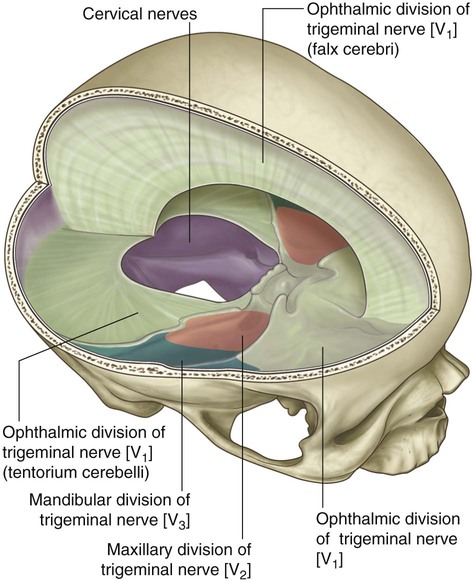
Innervation
Innervation of the dura mater (Fig. 8.34) is by small meningeal branches of all three divisions of the trigeminal nerve [V1, V2, and V3], the vagus nerve [X], and the first, second, and, sometimes, third cervical nerves. (Possible involvement of the glossopharyngeal [IX] and hypoglossal nerves [XII] in the posterior cranial fossa has also been reported.)
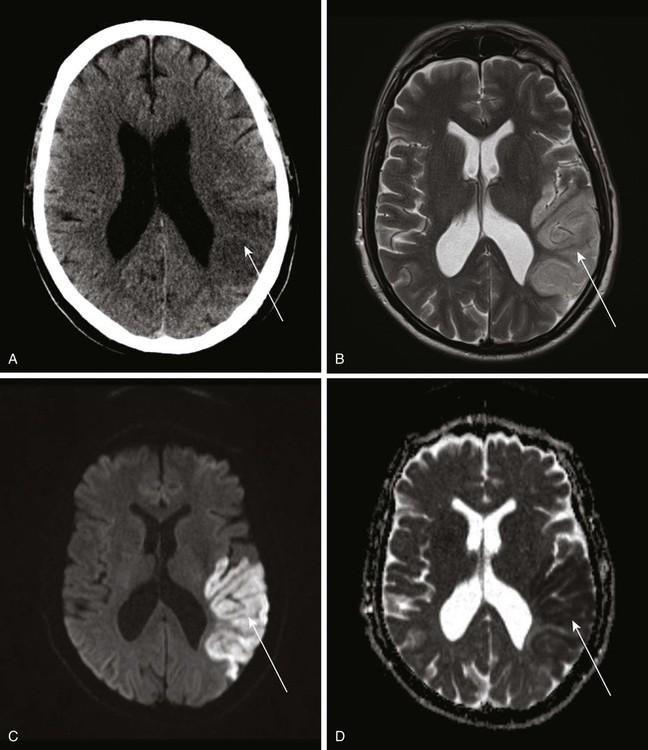
Arrangement of meninges and spaces
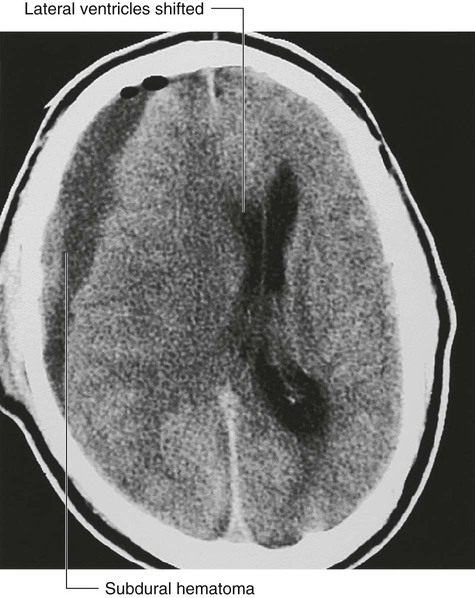
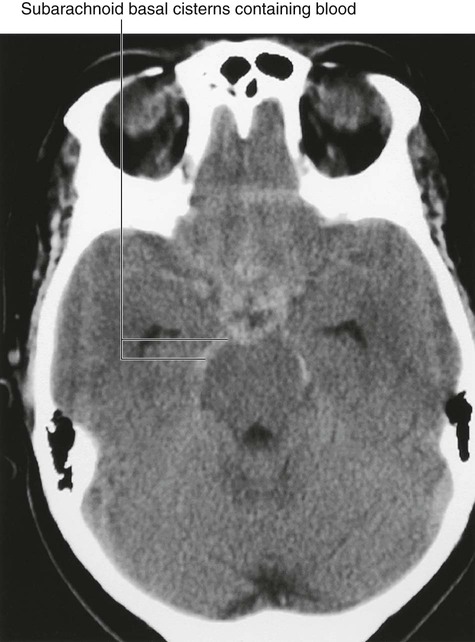
There is a unique arrangement of meninges coupled with real and potential spaces within the cranial cavity (Fig. 8.35).
Subarachnoid space
Deep to the arachnoid mater is the only normally occurring fluid-filled space associated with the meninges, the subarachnoid space (Fig. 8.35). It occurs because the arachnoid mater clings to the inner surface of the dura mater and does not follow the contour of the brain, while the pia mater, being against the surface of the brain, closely follows the grooves and fissures on the surface of the brain. The narrow subarachnoid space is therefore created between these two membranes (Fig. 8.35).
The CSF returns to the venous system through arachnoid villi. These project as clumps (arachnoid granulations) into the superior sagittal sinus, which is a dural venous sinus, and its lateral extensions, the lateral lacunae (Fig. 8.35).
Brain and its blood supply
Brain
The brain is a component of the central nervous system.
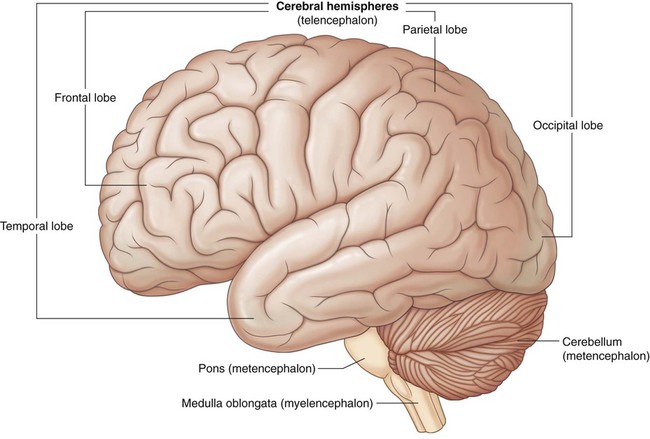
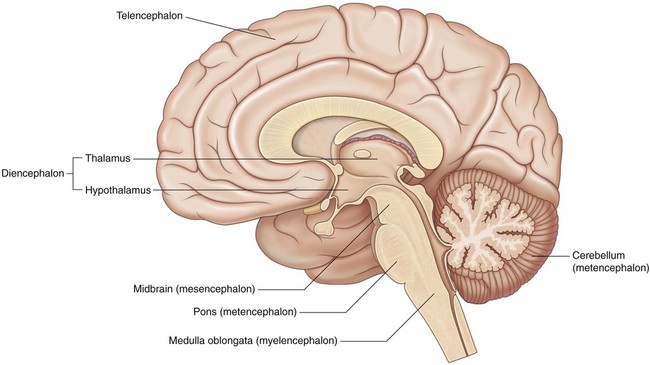
During development the brain can be divided into five continuous parts (Figs. 8.36 and 8.37). From rostral (or cranial) to caudal they are:
 The telencephalon (cerebrum) becomes the large cerebral hemispheres. The surface of these hemispheres consists of elevations (gyri) and depressions (sulci), and the hemispheres are partially separated by a deep longitudinal fissure. The cerebrum fills the area of the skull above the tentorium cerebelli and is subdivided into lobes based on position.
The telencephalon (cerebrum) becomes the large cerebral hemispheres. The surface of these hemispheres consists of elevations (gyri) and depressions (sulci), and the hemispheres are partially separated by a deep longitudinal fissure. The cerebrum fills the area of the skull above the tentorium cerebelli and is subdivided into lobes based on position.
 The diencephalon, which is hidden from view in the adult brain by the cerebral hemispheres, consists of the thalamus, hypothalamus, and other related structures, and classically is considered to be the most rostral part of the brainstem. (However, in common usage today, the term brainstem usually refers to the midbrain, pons, and medulla.)
The diencephalon, which is hidden from view in the adult brain by the cerebral hemispheres, consists of the thalamus, hypothalamus, and other related structures, and classically is considered to be the most rostral part of the brainstem. (However, in common usage today, the term brainstem usually refers to the midbrain, pons, and medulla.)
 The mesencephalon (midbrain), which is the first part of the brainstem seen when an intact adult brain is examined, located at the junction between and in both the middle and posterior cranial fossae.
The mesencephalon (midbrain), which is the first part of the brainstem seen when an intact adult brain is examined, located at the junction between and in both the middle and posterior cranial fossae.
 The metencephalon, which gives rise to the cerebellum (consisting of two lateral hemispheres and a midline part in the posterior cranial fossa below the tentorium cerebelli) and the pons (anterior to the cerebellum, and is a bulging part of the brainstem in the most anterior part of the posterior cranial fossa against the clivus and dorsum sellae).
The metencephalon, which gives rise to the cerebellum (consisting of two lateral hemispheres and a midline part in the posterior cranial fossa below the tentorium cerebelli) and the pons (anterior to the cerebellum, and is a bulging part of the brainstem in the most anterior part of the posterior cranial fossa against the clivus and dorsum sellae).
 The myelencephalon (medulla oblongata), the caudalmost part of the brainstem, ends at the foramen magnum or the uppermost rootlets of the first cervical nerve and to which cranial nerves VI to XII are attached.
The myelencephalon (medulla oblongata), the caudalmost part of the brainstem, ends at the foramen magnum or the uppermost rootlets of the first cervical nerve and to which cranial nerves VI to XII are attached.
Blood supply
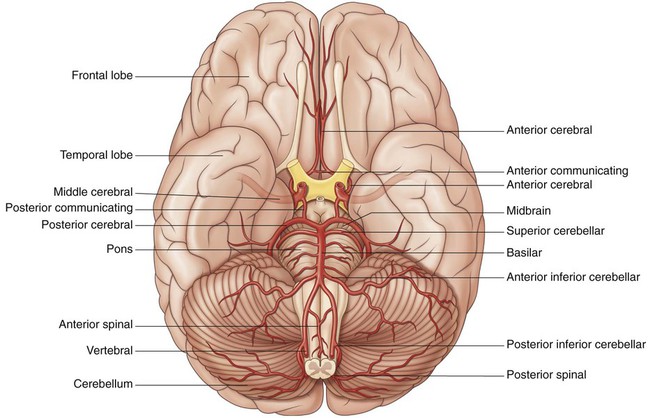
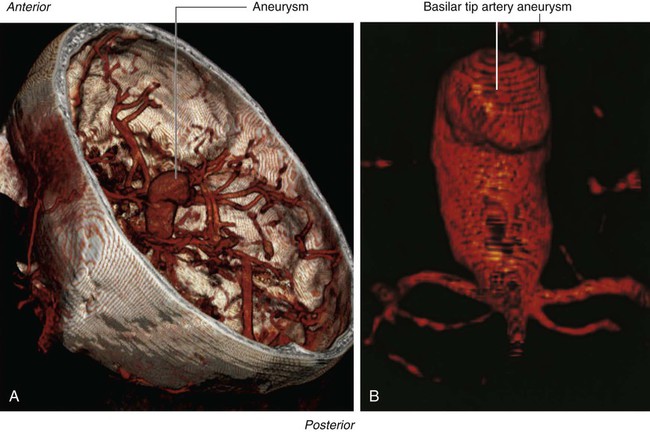
The brain receives its arterial supply from two pairs of vessels, the vertebral and internal carotid arteries (Fig. 8.38), which are interconnected in the cranial cavity to produce a cerebral arterial circle (of Willis).
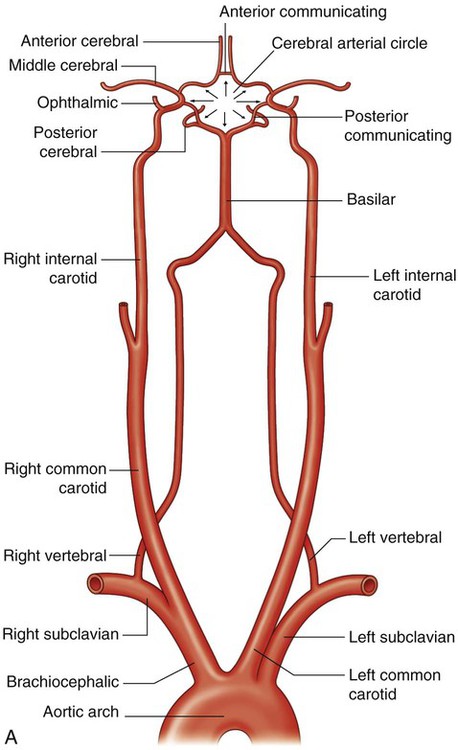
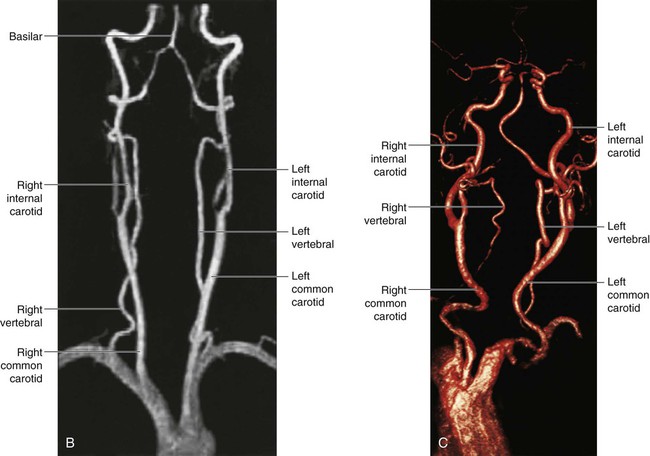
Vertebral arteries
Each vertebral artery arises from the first part of each subclavian artery (Fig. 8.38) in the lower part of the neck, and passes superiorly through the transverse foramina of the upper six cervical vertebrae. On entering the cranial cavity through the foramen magnum each vertebral artery gives off a small meningeal branch.
Continuing forward, the vertebral artery gives rise to three additional branches before joining with its companion vessel to form the basilar artery (Figs. 8.38 and 8.39):
 One branch joins with its companion from the other side to form the single anterior spinal artery, which then descends in the anterior median fissure of the spinal cord.
One branch joins with its companion from the other side to form the single anterior spinal artery, which then descends in the anterior median fissure of the spinal cord.
 A second branch is the posterior spinal artery, which passes posteriorly around the medulla and then descends on the posterior surface of the spinal cord in the area of the attachment of the posterior roots—there are two posterior spinal arteries, one on each side (although the posterior spinal arteries can originate directly from the vertebral arteries, they more commonly branch from the posterior inferior cerebellar arteries).
A second branch is the posterior spinal artery, which passes posteriorly around the medulla and then descends on the posterior surface of the spinal cord in the area of the attachment of the posterior roots—there are two posterior spinal arteries, one on each side (although the posterior spinal arteries can originate directly from the vertebral arteries, they more commonly branch from the posterior inferior cerebellar arteries).
 Just before the two vertebral arteries join, each gives off a posterior inferior cerebellar artery.
Just before the two vertebral arteries join, each gives off a posterior inferior cerebellar artery.
The basilar artery travels in a rostral direction along the anterior aspect of the pons (Fig. 8.39). Its branches in a caudal to rostral direction include the anterior inferior cerebellar arteries, several small pontine arteries, and the superior cerebellar arteries. The basilar artery ends as a bifurcation, giving rise to two posterior cerebral arteries.
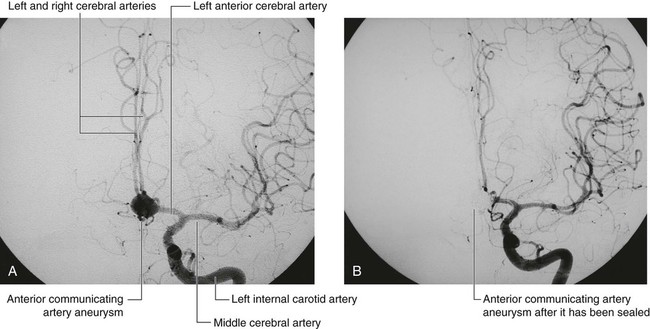
Internal carotid arteries
The two internal carotid arteries arise as one of the two terminal branches of the common carotid arteries (Fig. 8.38). They proceed superiorly to the base of the skull where they enter the carotid canal.
Entering the cranial cavity each internal carotid artery gives off the ophthalmic artery, the posterior communicating artery, the middle cerebral artery, and the anterior cerebral artery (Fig. 8.39).
Cerebral arterial circle
The cerebral arterial circle (of Willis) is formed at the base of the brain by the interconnecting vertebrobasilar and internal carotid systems of vessels (Fig. 8.38). This anastomotic interconnection is accomplished by:
 an anterior communicating artery connecting the left and right anterior cerebral arteries to each other, and
an anterior communicating artery connecting the left and right anterior cerebral arteries to each other, and
 two posterior communicating arteries, one on each side, connecting the internal carotid artery with the posterior cerebral artery (Figs. 8.38 and 8.39).
two posterior communicating arteries, one on each side, connecting the internal carotid artery with the posterior cerebral artery (Figs. 8.38 and 8.39).
Venous drainage
Also emptying into the dural venous sinuses are diploic veins, which run between the internal and external tables of compact bone in the roof of the cranial cavity, and emissary veins, which pass from outside the cranial cavity to the dural venous sinuses (Fig. 8.43).
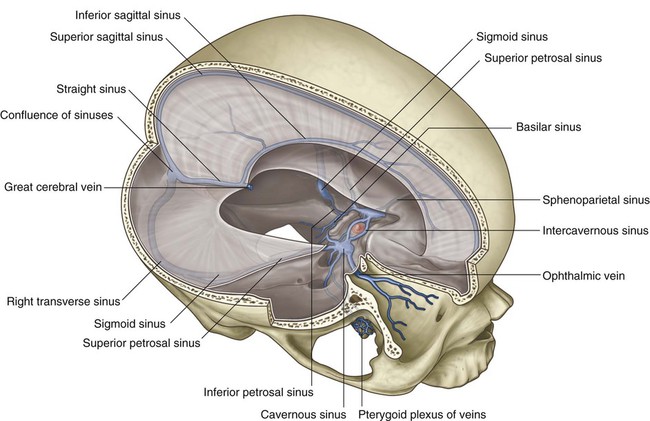
Dural venous sinuses
The dural venous sinuses include the superior sagittal, inferior sagittal, straight, transverse, sigmoid, and occipital sinuses, the confluence of sinuses, and the cavernous, sphenoparietal, superior petrosal, inferior petrosal, and basilar sinuses (Fig. 8.44, Table 8.3).
Table 8.3
| Dural sinus | Location | Receives |
| Superior sagittal | Superior border of falx cerebri | Superior cerebral, diploic, and emissary veins and CSF |
| Inferior sagittal | Inferior margin of falx cerebri | A few cerebral veins and veins from the falx cerebri |
| Straight | Junction of falx cerebri and tentorium cerebelli | Inferior sagittal sinus, great cerebral vein, posterior cerebral veins, superior cerebellar veins, and veins from the falx cerebri |
| Occipital | In falx cerebelli against occipital bone | Communicates inferiorly with vertebral plexus of veins |
| Confluence of sinuses | Dilated space at the internal occipital protuberance | Superior sagittal, straight, and occipital sinuses |
| Transverse (right and left) | Horizontal extensions from the confluence of sinuses along the posterior and lateral attachments of the tentorium cerebelli | Drainage from confluence of sinuses (right—transverse and usually superior sagittal sinuses; left—transverse and usually straight sinuses); also superior petrosal sinus, and inferior cerebral, cerebellar, diploic, and emissary veins |
| Sigmoid (right and left) | Continuation of transverse sinuses to internal jugular vein; groove of parietal, temporal, and occipital bones | Transverse sinuses, and cerebral, cerebellar, diploic, and emissary veins |
| Cavernous (paired) | Lateral aspect of body of sphenoid | Cerebral and ophthalmic veins, sphenoparietal sinuses, and emissary veins from pterygoid plexus of veins |
| Intercavernous | Crossing sella turcica | Interconnect cavernous sinuses |
| Sphenoparietal (paired) | Inferior surface of lesser wings of sphenoid | Diploic and meningeal veins |
| Superior petrosal (paired) | Superior margin of petrous part of temporal bone | Cavernous sinus, and cerebral and cerebellar veins |
| Inferior petrosal (paired) | Groove between petrous part of temporal bone and occipital bone ending in internal jugular vein | Cavernous sinus, cerebellar veins, and veins from the internal ear and brainstem |
| Basilar | Clivus, just posterior to sella turcica of sphenoid | Connect bilateral inferior petrosal sinuses and communicate with vertebral plexus of veins |
Superior sagittal sinus
The superior sagittal sinus is in the superior border of the falx cerebri (Fig. 8.44). It begins anteriorly at the foramen cecum, where it may receive a small emissary vein from the nasal cavity, and ends posteriorly in the confluence of sinuses, usually bending to the right to empty into the right transverse sinus. The superior sagittal sinus communicates with lateral extensions (lateral lacunae) of the sinus containing numerous arachnoid granulations.
Inferior sagittal and straight sinuses
The inferior sagittal sinus is in the inferior margin of the falx cerebri (Fig. 8.44). It receives a few cerebral veins and veins from the falx cerebri, and ends posteriorly at the anterior edge of the tentorium cerebelli, where it is joined by the great cerebral vein and together with the great cerebral vein forms the straight sinus (Fig. 8.44).
Confluence of sinuses, transverse and sigmoid sinuses
The superior sagittal and straight sinuses, and the occipital sinus (in the falx cerebelli) empty into the confluence of sinuses, which is a dilated space at the internal occipital protuberance (Fig. 8.44) and is drained by the right and left transverse sinuses.
As the transverse sinuses leave the surface of the occipital bone, they become the sigmoid sinuses (Fig. 8.44), which turn inferiorly, grooving the parietal, temporal, and occipital bones, before ending at the beginning of the internal jugular veins. The sigmoid sinuses also receive blood from cerebral, cerebellar, diploic, and emissary veins.
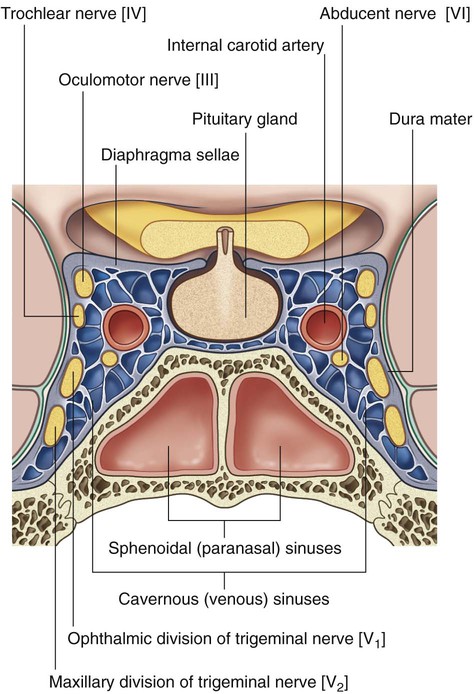
Cavernous sinuses
The paired cavernous sinuses are against the lateral aspect of the body of the sphenoid bone on either side of the sella turcica (Fig. 8.45). They are of great clinical importance because of their connections and the structures that pass through them.
Structures passing through each cavernous sinus are:
Structures in the lateral wall of each cavernous sinus are, from superior to inferior:
Connecting the right and left cavernous sinuses are the intercavernous sinuses on the anterior and posterior sides of the pituitary stalk (Fig. 8.44).
Superior and inferior petrosal sinuses
The superior petrosal sinuses drain the cavernous sinuses into the transverse sinuses. Each superior petrosal sinus begins at the posterior end of the cavernous sinus, passes posterolaterally along the superior margin of the petrous part of each temporal bone, and connects to the transverse sinus (Fig. 8.44). The superior petrosal sinuses also receive cerebral and cerebellar veins.
Basilar sinuses connect the inferior petrosal sinuses to each other and to the vertebral plexus of veins. They are on the clivus, just posterior to the sella turcica of the sphenoid bone (Fig. 8.44).
Cranial nerves
In addition to having somatic and visceral components similar to those of spinal nerves, some cranial nerves also contain special sensory and motor components (Tables 8.4 and 8.5).
Table 8.4
Cranial nerve functional components
| Functional component | Abbreviation | General function | Cranial nerves containing component |
| General somatic afferent | GSA | Perception of touch, pain, temperature | Trigeminal nerve [V]; facial nerve [VII]; glossopharyngeal nerve [IX]; vagus nerve [X] |
| General visceral afferent | GVA | Sensory input from viscera | Glossopharyngeal nerve [IX]; vagus nerve [X] |
| Special afferent* | SA | Smell, taste, vision, hearing, and balance | Olfactory nerve [I]; optic nerve [II]; facial nerve [VII]; vestibulocochlear nerve [VIII]; glossopharyngeal nerve [IX]; vagus nerve [X] |
| General somatic efferent | GSE | Motor innervation to skeletal (voluntary) muscles | Oculomotor nerve [III]; trochlear nerve [IV]; abducent nerve [VI]; accessory nerve [XI]; hypoglossal nerve [XII] |
| General visceral efferent | GVE | Motor innervation to smooth muscle, heart muscle, and glands | Oculomotor nerve [III]; facial nerve [VII]; glossopharyngeal nerve [IX]; vagus nerve [X] |
| Branchial efferent** | BE | Motor innervation to skeletal muscles derived from pharyngeal arch mesoderm | Trigeminal nerve [V]; facial nerve [VII]; glossopharyngeal nerve [IX]; vagus nerve [X] |
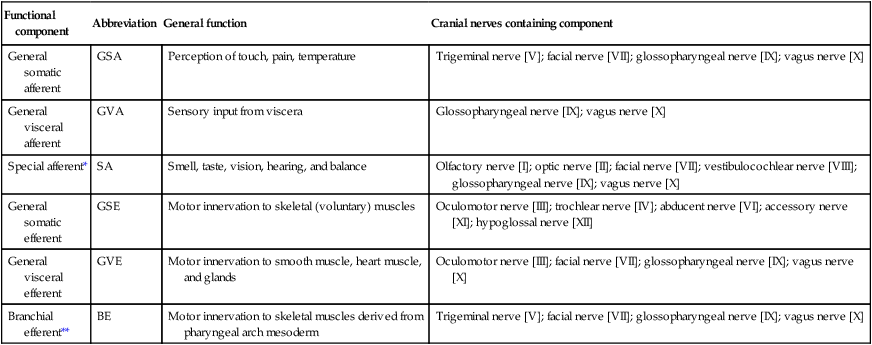
Other terminology used when describing functional components:
*Special sensory, or special visceral afferent (SVA): smell, taste. Special somatic afferent (SSA): vision, hearing, balance.
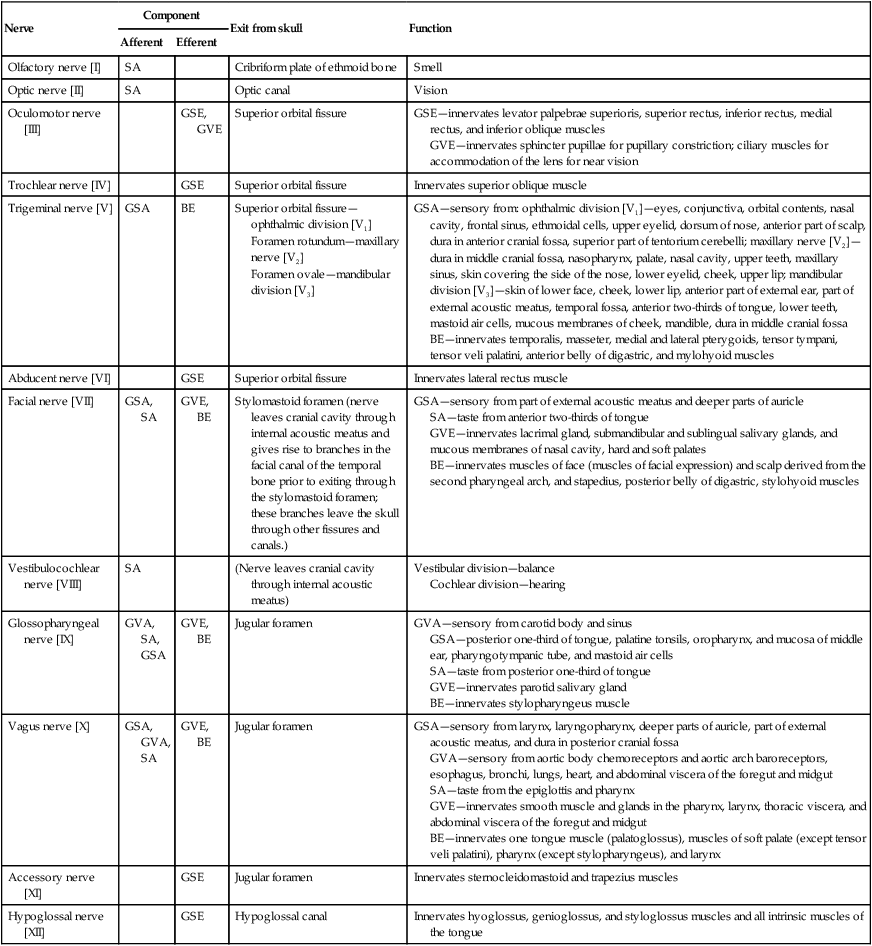
Table 8.5
Cranial nerves (see Table 8.4 for abbreviations)
| Nerve | Component | Exit from skull | Function | |
| Afferent | Efferent | |||
| Olfactory nerve [I] | SA | Cribriform plate of ethmoid bone | Smell | |
| Optic nerve [II] | SA | Optic canal | Vision | |
| Oculomotor nerve [III] | GSE, GVE | Superior orbital fissure | GSE—innervates levator palpebrae superioris, superior rectus, inferior rectus, medial rectus, and inferior oblique muscles GVE—innervates sphincter pupillae for pupillary constriction; ciliary muscles for accommodation of the lens for near vision |
|
| Trochlear nerve [IV] | GSE | Superior orbital fissure | Innervates superior oblique muscle | |
| Trigeminal nerve [V] | GSA | BE | Superior orbital fissure—ophthalmic division [V1] Foramen rotundum—maxillary nerve [V2] Foramen ovale—mandibular division [V3] |
GSA—sensory from: ophthalmic division [V1]—eyes, conjunctiva, orbital contents, nasal cavity, frontal sinus, ethmoidal cells, upper eyelid, dorsum of nose, anterior part of scalp, dura in anterior cranial fossa, superior part of tentorium cerebelli; maxillary nerve [V2]—dura in middle cranial fossa, nasopharynx, palate, nasal cavity, upper teeth, maxillary sinus, skin covering the side of the nose, lower eyelid, cheek, upper lip; mandibular division [V3]—skin of lower face, cheek, lower lip, anterior part of external ear, part of external acoustic meatus, temporal fossa, anterior two-thirds of tongue, lower teeth, mastoid air cells, mucous membranes of cheek, mandible, dura in middle cranial fossa BE—innervates temporalis, masseter, medial and lateral pterygoids, tensor tympani, tensor veli palatini, anterior belly of digastric, and mylohyoid muscles |
| Abducent nerve [VI] | GSE | Superior orbital fissure | Innervates lateral rectus muscle | |
| Facial nerve [VII] | GSA, SA | GVE, BE | Stylomastoid foramen (nerve leaves cranial cavity through internal acoustic meatus and gives rise to branches in the facial canal of the temporal bone prior to exiting through the stylomastoid foramen; these branches leave the skull through other fissures and canals.) | GSA—sensory from part of external acoustic meatus and deeper parts of auricle SA—taste from anterior two-thirds of tongue GVE—innervates lacrimal gland, submandibular and sublingual salivary glands, and mucous membranes of nasal cavity, hard and soft palates BE—innervates muscles of face (muscles of facial expression) and scalp derived from the second pharyngeal arch, and stapedius, posterior belly of digastric, stylohyoid muscles |
| Vestibulocochlear nerve [VIII] | SA | (Nerve leaves cranial cavity through internal acoustic meatus) | Vestibular division—balance Cochlear division—hearing |
|
| Glossopharyngeal nerve [IX] | GVA, SA, GSA | GVE, BE | Jugular foramen | GVA—sensory from carotid body and sinus GSA—posterior one-third of tongue, palatine tonsils, oropharynx, and mucosa of middle ear, pharyngotympanic tube, and mastoid air cells SA—taste from posterior one-third of tongue GVE—innervates parotid salivary gland BE—innervates stylopharyngeus muscle |
| Vagus nerve [X] | GSA, GVA, SA | GVE, BE | Jugular foramen | GSA—sensory from larynx, laryngopharynx, deeper parts of auricle, part of external acoustic meatus, and dura in posterior cranial fossa GVA—sensory from aortic body chemoreceptors and aortic arch baroreceptors, esophagus, bronchi, lungs, heart, and abdominal viscera of the foregut and midgut SA—taste from the epiglottis and pharynx GVE—innervates smooth muscle and glands in the pharynx, larynx, thoracic viscera, and abdominal viscera of the foregut and midgut BE—innervates one tongue muscle (palatoglossus), muscles of soft palate (except tensor veli palatini), pharynx (except stylopharyngeus), and larynx |
| Accessory nerve [XI] | GSE | Jugular foramen | Innervates sternocleidomastoid and trapezius muscles | |
| Hypoglossal nerve [XII] | GSE | Hypoglossal canal | Innervates hyoglossus, genioglossus, and styloglossus muscles and all intrinsic muscles of the tongue | |
 first arch—trigeminal nerve [V3],
first arch—trigeminal nerve [V3],
 second arch—facial nerve [VII],
second arch—facial nerve [VII],
 third arch—glossopharyngeal nerve [IX],
third arch—glossopharyngeal nerve [IX],
 fourth arch—superior laryngeal branch of the vagus nerve [X],
fourth arch—superior laryngeal branch of the vagus nerve [X],
 sixth arch—recurrent laryngeal branch of the vagus nerve [X].
sixth arch—recurrent laryngeal branch of the vagus nerve [X].
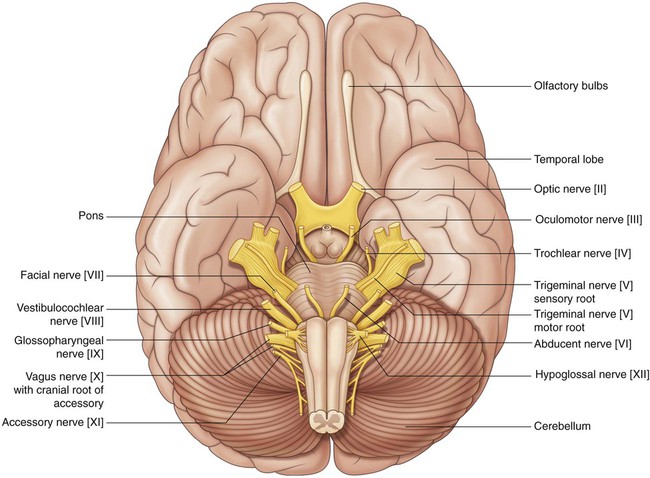
Olfactory nerve [I]
The receptors are in the roof and upper parts of the nasal cavity, and the central processes, after joining into small bundles, enter the cranial cavity by passing through the cribriform plate of the ethmoid bone (Fig. 8.50). They terminate by synapsing with secondary neurons in the olfactory bulbs (Fig. 8.51).
Optic nerve [II]
The optic nerve [II] carries SA fibers for vision. These fibers return information to the brain from photoreceptors in the retina. Neuronal processes leave the retinal receptors, join into small bundles, and are carried by the optic nerves to other components of the visual system in the brain. The optic nerves enter the cranial cavity through the optic canals (Fig. 8.50).
Oculomotor nerve [III]
The oculomotor nerve [III] carries two types of fibers:
 General somatic efferent (GSE) fibers innervate most of the extra-ocular muscles.
General somatic efferent (GSE) fibers innervate most of the extra-ocular muscles.
 General visceral efferent (GVE) fibers are part of the parasympathetic part of the autonomic division of the PNS.
General visceral efferent (GVE) fibers are part of the parasympathetic part of the autonomic division of the PNS.
The oculomotor nerve [III] leaves the anterior surface of the brainstem between the midbrain and the pons (Fig. 8.51). It enters the anterior edge of the tentorium cerebelli, continues in an anterior direction in the lateral wall of the cavernous sinus (Figs. 8.50 and 8.51; see Fig. 8.45), and leaves the cranial cavity through the superior orbital fissure.
Trochlear nerve [IV]
The trochlear nerve [IV] is a cranial nerve that carries GSE fibers to innervate the superior oblique muscle, an extra-ocular muscle in the orbit. It arises in the midbrain and is the only cranial nerve to exit from the posterior surface of the brainstem (Fig. 8.51). After curving around the midbrain, it enters the inferior surface of the free edge of the tentorium cerebelli, continues in an anterior direction in the lateral wall of the cavernous sinus (Figs. 8.50 and 8.51; see Fig. 8.45), and enters the orbit through the superior orbital fissure.
Trigeminal nerve [V]
 The GSA fibers provide sensory input from the face, anterior one-half of the scalp, mucous membranes of the oral and nasal cavities and the paranasal sinuses, the nasopharynx, part of the ear and external acoustic meatus, part of the tympanic membrane, the orbital contents and conjunctiva, and the dura mater in the anterior and middle cranial fossae.
The GSA fibers provide sensory input from the face, anterior one-half of the scalp, mucous membranes of the oral and nasal cavities and the paranasal sinuses, the nasopharynx, part of the ear and external acoustic meatus, part of the tympanic membrane, the orbital contents and conjunctiva, and the dura mater in the anterior and middle cranial fossae.
 The BE fibers innervate the muscles of mastication; the tensor tympani, tensor veli palatini, and mylohyoid muscles; and the anterior belly of the digastric muscle.
The BE fibers innervate the muscles of mastication; the tensor tympani, tensor veli palatini, and mylohyoid muscles; and the anterior belly of the digastric muscle.
The trigeminal nerve exits from the anterolateral surface of the pons as a large sensory root and a small motor root (Fig. 8.51). These roots continue forward out of the posterior cranial fossa and into the middle cranial fossa by passing over the medial tip of the petrous part of the temporal bone (Fig. 8.50).
In the middle cranial fossa the sensory root expands into the trigeminal ganglion (Fig. 8.50), which contains cell bodies for the sensory neurons in the trigeminal nerve and is comparable to a spinal ganglion. The ganglion is in a depression (the trigeminal depression) on the anterior surface of the petrous part of the temporal bone, in a dural cave (the trigeminal cave). The motor root is below and completely separate from the sensory root at this point.
Abducent nerve [VI]
The abducent nerve [VI] carries GSE fibers to innervate the lateral rectus muscle in the orbit. It arises from the brainstem between the pons and medulla and passes forward, piercing the dura covering the clivus (Figs. 8.50 and 8.51). Continuing upward in a dural canal, it crosses the superior edge of the petrous temporal bone, enters and crosses the cavernous sinus (see Fig. 8.45) just inferolateral to the internal carotid artery, and enters the orbit through the superior orbital fissure.
Facial nerve [VII]
The facial nerve [VII] carries GSA, SA, GVE, and BE fibers:
 The GSA fibers provide sensory input from part of the external acoustic meatus and deeper parts of the auricle.
The GSA fibers provide sensory input from part of the external acoustic meatus and deeper parts of the auricle.
 The SA fibers are for taste from the anterior two-thirds of the tongue.
The SA fibers are for taste from the anterior two-thirds of the tongue.
 The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate secretomotor activity in the lacrimal gland, submandibular and sublingual salivary glands, and glands in the mucous membranes of the nasal cavity, and hard and soft palates.
The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate secretomotor activity in the lacrimal gland, submandibular and sublingual salivary glands, and glands in the mucous membranes of the nasal cavity, and hard and soft palates.
 The BE fibers innervate the muscles of the face (muscles of facial expression) and scalp derived from the second pharyngeal arch, and the stapedius muscle, the posterior belly of the digastric muscle, and the stylohyoid muscle.
The BE fibers innervate the muscles of the face (muscles of facial expression) and scalp derived from the second pharyngeal arch, and the stapedius muscle, the posterior belly of the digastric muscle, and the stylohyoid muscle.
The facial nerve [VII] attaches to the lateral surface of the brainstem, between the pons and medulla oblongata (Fig. 8.51). It consists of a large motor root and a smaller sensory root (the intermediate nerve):
 The intermediate nerve contains the SA fibers for taste, the parasympathetic GVE fibers, and the GSA fibers.
The intermediate nerve contains the SA fibers for taste, the parasympathetic GVE fibers, and the GSA fibers.
The motor and sensory roots cross the posterior cranial fossa and leave the cranial cavity through the internal acoustic meatus (Fig. 8.50). After entering the facial canal in the petrous part of the temporal bone, the two roots fuse and form the facial nerve [VII]. Near this point the nerve enlarges as the geniculate ganglion, which is similar to a spinal ganglion containing cell bodies for sensory neurons.
At the geniculate ganglion the facial nerve [VII] turns and gives off the greater petrosal nerve, which carries mainly preganglionic parasympathetic (GVE) fibers (Table 8.6).
Table 8.6
Parasympathetic ganglia of the head
| Ganglion | Cranial nerve origin of preganglionic fibers | Branch supplying preganglionic fibers to ganglion | Function |
| Ciliary | Oculomotor nerve [III] | Branch to ciliary ganglion | Innervation of sphincter pupillae muscle for pupillary constriction, and ciliary muscles for accommodation of the lens for near vision |
| Pterygopalatine | Facial nerve [VII] | Greater petrosal nerve | Innervation of lacrimal gland, and mucous glands of nasal cavity, maxillary sinus, and palate |
| Otic | Glossopharyngeal nerve [IX] | Lesser petrosal nerve | Innervation of parotid gland |
| Submandibular | Facial nerve [VII] | Chorda tympani to lingual | Innervation of submandibular and sublingual glands |
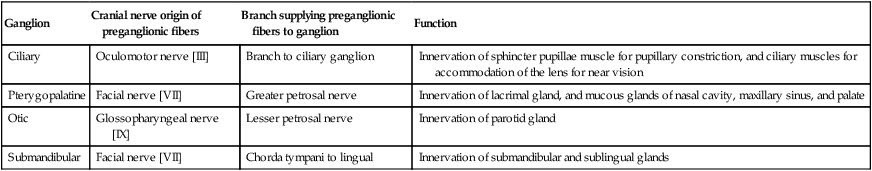
The chorda tympani carries taste (SA) fibers from the anterior two-thirds of the tongue and preganglionic parasympathetic (GVE) fibers destined for the submandibular ganglion (Table 8.6).
Vestibulocochlear nerve [VIII]
The vestibulocochlear nerve [VIII] attaches to the lateral surface of the brainstem, between the pons and medulla, after emerging from the internal acoustic meatus and crossing the posterior cranial fossa (Figs. 8.50 and 8.51). The two divisions combine into the single nerve seen in the posterior cranial fossa within the substance of the petrous part of the temporal bone.
Glossopharyngeal nerve [IX]
The glossopharyngeal nerve [IX] carries GVA, GSA, SA, GVE, and BE fibers:
 The GVA fibers provide sensory input from the carotid body and sinus.
The GVA fibers provide sensory input from the carotid body and sinus.
 The GSA fibers provide sensory input from the posterior one-third of the tongue, palatine tonsils, oropharynx, and mucosa of the middle ear, pharyngotympanic tube, and mastoid air cells.
The GSA fibers provide sensory input from the posterior one-third of the tongue, palatine tonsils, oropharynx, and mucosa of the middle ear, pharyngotympanic tube, and mastoid air cells.
 The SA fibers are for taste from the posterior one-third of the tongue.
The SA fibers are for taste from the posterior one-third of the tongue.
 The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate secretomotor activity in the parotid salivary gland.
The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate secretomotor activity in the parotid salivary gland.
 The BE fibers innervate the muscle derived from the third pharyngeal arch (the stylopharyngeus muscle).
The BE fibers innervate the muscle derived from the third pharyngeal arch (the stylopharyngeus muscle).
The glossopharyngeal nerve [IX] arises as several rootlets on the anterolateral surface of the upper medulla oblongata (Fig. 8.51). The rootlets cross the posterior cranial fossa and enter the jugular foramen (Fig. 8.50). Within the jugular foramen, and before exiting from it, the rootlets merge to form the glossopharyngeal nerve.
Tympanic nerve
The tympanic nerve also contributes GVE fibers, which leave the tympanic plexus in the lesser petrosal nerve—a small nerve that exits the temporal bone, enters the middle cranial fossa, and descends through the foramen ovale to exit the cranial cavity carrying preganglionic parasympathetic fibers to the otic ganglion (Table 8.6).
Vagus nerve [X]
The vagus nerve [X] carries GSA, GVA, SA, GVE, and BE fibers:
 The GSA fibers provide sensory input from the larynx, laryngopharynx, deeper parts of the auricle, part of the external acoustic meatus, and the dura mater in the posterior cranial fossa.
The GSA fibers provide sensory input from the larynx, laryngopharynx, deeper parts of the auricle, part of the external acoustic meatus, and the dura mater in the posterior cranial fossa.
 The GVA fibers provide sensory input from the aortic body chemoreceptors and aortic arch baroreceptors, and the esophagus, bronchi, lungs, heart, and abdominal viscera in the foregut and midgut.
The GVA fibers provide sensory input from the aortic body chemoreceptors and aortic arch baroreceptors, and the esophagus, bronchi, lungs, heart, and abdominal viscera in the foregut and midgut.
 The SA fibers are for taste around the epiglottis and pharynx.
The SA fibers are for taste around the epiglottis and pharynx.
 The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate smooth muscle and glands in the pharynx, larynx, thoracic viscera, and abdominal viscera of the foregut and midgut.
The GVE fibers are part of the parasympathetic part of the autonomic division of the PNS and stimulate smooth muscle and glands in the pharynx, larynx, thoracic viscera, and abdominal viscera of the foregut and midgut.
 The BE fibers innervate one muscle of the tongue (palatoglossus), the muscles of the soft palate (except the tensor veli palatini), pharynx (except the stylopharyngeus), and larynx.
The BE fibers innervate one muscle of the tongue (palatoglossus), the muscles of the soft palate (except the tensor veli palatini), pharynx (except the stylopharyngeus), and larynx.
The vagus nerve arises as a group of rootlets on the anterolateral surface of the medulla oblongata just inferior to the rootlets arising to form the glossopharyngeal nerve [IX] (Fig. 8.51). The rootlets cross the posterior cranial fossa and enter the jugular foramen (Fig. 8.50). Within this foramen, and before exiting from it, the rootlets merge to form the vagus nerve [X]. Within or immediately outside the jugular foramen are two ganglia, the superior (jugular) and inferior (nodose) ganglia, which contain the cell bodies of the sensory neurons in the vagus nerve [X].
Accessory nerve [XI]
The accessory nerve [XI] is a cranial nerve that carries GSE fibers to innervate the sternocleidomastoid and trapezius muscles. It is a unique cranial nerve because its roots arise from motor neurons in the upper five segments of the cervical spinal cord. These fibers leave the lateral surface of the spinal cord and, joining together as they ascend, enter the cranial cavity through the foramen magnum (Fig. 8.51). The accessory nerve [XI] continues through the posterior cranial fossa and exits through the jugular foramen (Fig. 8.50). It then descends in the neck to innervate the sternocleidomastoid and trapezius muscles from their deep surfaces.
Cranial root of the accessory nerve
Some descriptions of the accessory nerve [XI] refer to a few rootlets arising from the caudal part of the medulla oblongata on the anterolateral surface just inferior to the rootlets arising to form the vagus nerve [X] as the “cranial” root of the accessory nerve (Fig. 8.51). Leaving the medulla, the cranial roots course with the “spinal” roots of the accessory nerve [XI] into the jugular foramen, at which point the cranial roots join the vagus nerve [X]. As part of the vagus nerve [X], they are distributed to the pharyngeal musculature innervated by the vagus nerve [X] and are therefore described as being part of the vagus nerve [X].
Hypoglossal nerve [XII]
The hypoglossal nerve [XII] carries GSE fibers to innervate all intrinsic muscles and most of the extrinsic muscles of the tongue. It arises as several rootlets from the anterior surface of the medulla (Fig. 8.51), passes laterally across the posterior cranial fossa, and exits through the hypoglossal canal (Fig. 8.50). This nerve innervates the hyoglossus, styloglossus, and genioglossus muscles and all intrinsic muscles of the tongue.