HEAD (ALSO EYE, EAR, NOSE, THROAT, AND MOUTH)
HEADACHE
Tension or fatigue headache is characterized by throbbing pain in the temples, over the eyes, and in the posterior neck and shoulder muscles. It can be treated with rest, sunglasses, and moderate pain medication, such as aspirin or acetaminophen every 3 to 4 hours. Sometimes, applying warm packs or massage to tense muscles relaxes them and helps relieve the pain.
Migraine headache is generally more severe. It is defined as episodic attacks of headache lasting 4 to 72 hours and characterized by at least two of the following: moderate to severe intensity, one-sided pain, throbbing or “pulsating,” and worsening with movement. In addition, there is nausea or vomiting (which may be treated with metoclopramide [Reglan] 10 mg by mouth or with ondansetron [Zofran] 4 mg oral dissolving tablet), and aversion to light or sound. Migraine headache is currently thought to be caused by painful dilation of small arteries in the head. Migraine headaches have many variations, which may include stuffy or runny nose and weakness of an arm or a leg. Some people experience an “aura” before the “classic” migraine headache, in which they may smell strange odors or see flashing lights. Others develop tunnel vision—diminished peripheral vision. The headaches are characterized as excruciating, pounding, or explosive. Occasionally they will respond to nonsteroidal antiinflammatory medications, such as ibuprofen, but often require stronger pain medications and sometimes may need to be treated with narcotics. A person suffering from a migraine should be placed in a quiet, dark area to minimize external stimuli. He should be encouraged to drink enough liquid to treat or prevent dehydration and offered ibuprofen, acetaminophen, or aspirin. Caffeine may be helpful.
Specific antimigraine medications include the “triptans,” such as sumatriptan (Imitrex), naratriptan (Amerge), rizatriptan (Maxalt), and zolmitriptan (Zomig). These medications should be given as early as possible in the course of the headache to achieve maximal effectiveness. Other medicines that are effective include propranolol or metoprolol, amitriptyline, methysergide, flunarizine, and prochlorperazine (Compazine) given with diphenhydramine (Benadryl). Ergotamine drugs (such as dihydroergotamine mesylate [Migranal] nasal spray) directly constrict arteries; these should only be used under the direct supervision of a physician, since they may worsen the effects of certain types of migraines. If an oxygen (see page 431) tank is available, the victim may get some relief by breathing 10 liters per minute by face mask. An elderly person with a severe migraine, which may be confused with a stroke (see page 144), should seek immediate medical attention. A migraine headache may be precipitated by lack of sleep, high altitude, emotional stress, cyclical hormone changes, noxious odors, and certain ingested substances (such as caffeine and monosodium glutamate). Therefore, the migraine sufferer should seek to obtain regular sleep (go to bed and wake up at the same times every day), rest, and meals (do not skip or delay); limit caffeine consumption to the equivalent of two cups of coffee or two 12-ounce sodas per day; avoid tobacco products; avoid known personal triggers (e.g., red wine); practice relaxation techniques; and strive to maintain fitness through regular exercise and dietary discretion. For certain sufferers, a neurologist may prescribe topiramate (Topamax) to be taken between episodes of migraine to reduce the frequency of headaches.
Sinus headache is associated with sinus infection (see page 194) and is typified by fever, nasal congestion, production of a foul nasal discharge, and pain produced by tapping over the affected sinus(es). It should be treated with an oral decongestant (pseudoephedrine), nasal spray (Neo-Synephrine 0.25% or Afrin 0.05%), an antibiotic (azithromycin, amoxicillin-clavulanate, erythromycin, or ampicillin) if an infection is present, and warm packs applied over the affected sinus(es).
Subarachnoid hemorrhage is bleeding that occurs, usually suddenly, from a leaking blood vessel (commonly an aneurysm) underneath the thin tissue layer that surrounds the brain and spinal cord. The headache is usually sudden in onset, described as “the worst headache of my life,” and may be associated with a fainting spell, altered mental status, seizure, and collapse. If a person suffers a subarachnoid hemorrhage and remains awake, he may complain of a stiff or painful neck with or without back pain about 2 to 4 hours after the bleed. Anyone who complains of a severe headache after extreme physical straining (such as weight lifting or a difficult bowel movement) or who collapses suddenly after reporting a headache should be suspected to have suffered a subarachnoid hemorrhage and be brought rapidly to a hospital.
Meningitis, an infection that involves the lining of the brain and spinal cord, is a true emergency. The headache of meningitis is severe, and often accompanied by nausea, vomiting, photophobia, fever, altered mental status, and weakness. A purplish skin rash indicates infection with the bacteria Neisseria meningitidis, a particularly fulminant and contagious form (“meningococcal”) of infectious meningitis. The classic signs of meningitis are a stiff neck with a fever. The victim demonstrates extreme discomfort when the chin is flexed downward against the chest, and may complain that the pain also occurs in the back (along the course of the spinal cord). It is important to note that an infant can suffer meningitis without a stiff neck and may present only with poor feeding, fever, vomiting, seizures, and extreme lethargy (“floppy baby”). If meningitis is suspected, the victim must be evacuated rapidly. If antibiotics are available, the recommendations currently given to doctors for antibiotics are as follows: age 16 to 50 years, vancomycin plus either cefotaxime or ceftriaxone; age greater than 50 years, vancomycin plus either cefotaxime or ceftriaxone, as well as ampicillin.
Giant cell arteritis is a type of inflammation that occurs in elders that can affect the temporal artery, which travels in a path along the sides of the scalp over the ears (temples). The associated headache may be quite severe and accompanied by thickened and tender arteries that may be noticeably enlarged with or without overlying reddened skin. Pulses may or may not be appreciated in these arteries, and the victim may have pain radiating down the side of the face as low as into the jaw. Permanent partial or complete loss of vision may occur in one or both eyes, which makes this condition an emergency. This condition is frequently associated with the disorder polymyalgia rheumatica. The immediate treatment is administration of a corticosteroid, such as prednisone 40 to 60 mg by mouth each day until a physician can evaluate the patient.
A headache that is atypically severe or prolonged may represent a serious problem, such as accelerated (out of control) high blood pressure (hypertension), brain tumor, infection, glaucoma, blood clot within the brain, carbon monoxide poisoning, inflammation of the temporal artery, or hemorrhage. The victim should be evaluated by a physician at the earliest opportunity. If a person develops a severe headache associated with a fainting spell or stiff neck, or is known to suffer from high blood pressure, keep him as calm as possible and urgently seek assistance. If high blood pressure is known to be the problem, and the victim is taking antihypertensive drugs, he should be advised to avoid using medications or other substances that might counteract the effects of his antihypertensives. These include ephedra, phenylephrine, certain herbal supplements (such as ginseng and yohimbine), appetite suppressants, anabolic steroids, and certain nonsteroidal antiinflammatory drugs.
In general, particularly worrisome headaches include a single headache that is the “first” or “worst” of a person’s life; headache with a fever that is not explained by an obvious illness; headache with vomiting that is not explained by an obvious illness; headache associated with a neurologic sign, such as weakness or altered speech; headache associated with altered mental status; headache associated with neck pain when the chin is flexed to the chest; progressively worsening headache; sudden headache in an elder; headache in someone suffering from cancer; headache after a blow to the head; headache following an episode of loss of consciousness; or headache in someone suffering from immunosuppression.
EAR
Earache
An earache may be caused by infection, injury, or a foreign body in the ear. For a discussion of ear squeeze (barotitis) that occurs with scuba diving, see page 404.
Ear Infection
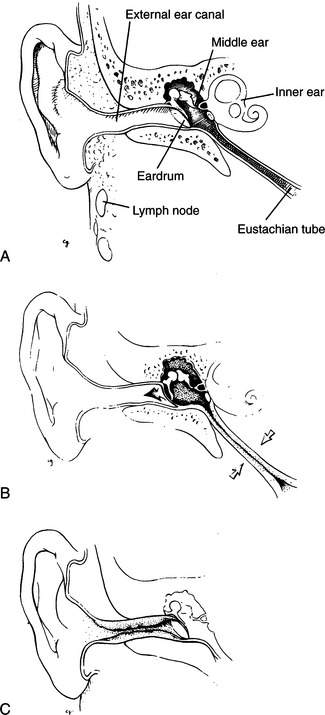
Ear infection can be either internal (otitis media) or external (otitis externa) to the eardrum (tympanic membrane) (Figure 107).
Otitis media. Infection may occur that reddens and inflames the eardrum and causes blood, serum, or pus to collect behind the drum (see Figure 107, B). With otitis media (middle ear infection), there is no drainage from the external ear canal (unless the eardrum ruptures, which is unusual in an adult, although more common in a child) and the victim has a fever, often with a sore throat. In many cases, the victim has a history of prior infections. Most often, otitis media occurs in children; when it occurs in an adult, it may be associated with a sinus infection or functional obstruction of the eustachian tube (the pressure-release mechanism from the middle ear into the throat). A young child can rapidly become severely ill from otitis media; an infant may develop meningitis (see page 174) following an ear infection. It is interesting to note that children who chew sugarless gum containing xylitol (or who ingest syrup or granules containing xylitol), which is derived from birch trees, may have fewer ear infections. This is supposedly because xylitol inhibits the growth of certain bacteria that cause the infections. It is reasonable to advise children prone to ear infections to avoid sugar-containing gum or candies.
Although many cases of otitis media in children are caused by viruses, such as respiratory syncytial virus, and resolve without antibiotic treatment, if you are distant from physician care and suspect otitis media, treat the child victim with an antibiotic. Adults and children should be treated with amoxicillin (80 to 100 mg/kg [2.2 lb] of body weight per day in three divided doses), amoxicillin-clavulanate (same dose of the amoxicillin component as for amoxicillin), cefdinir (14 mg/kg once daily or in 2 divided doses), cefpodoxime (10 mg/kg once daily or in two divided doses), cefuroxime (15 mg/kg in two divided doses), or clarithromycin for 10 days, or with azithromycin for 5 days. An additional antibiotic choice for children is erythromycin-sulfisoxazole for 10 days. Other antibiotics that have been approved for treatment are cephalexin, cefprozil, loracarbef, and ceftibuten. Aspirin, ibuprofen, or acetaminophen should be used to control fever. To avoid Reye syndrome (postviral encephalopathy and liver failure), do not use aspirin to control fever in a child under age 17.
Otitis externa (swimmer’s ear). Ear infection, commonly from the bacterium Pseudomonas aeruginosa, that develops in the external ear canal (often noted in swimmers and divers who do not keep the canal completely dry) rarely involves the eardrum (see Figure 107, C). When the external canal is kept moist, it is easier for bacteria to invade the skin and cause infection. The earliest symptom may be itching. Subsequent symptoms include a white to yellow-green liquid or cheesy discharge from the ear, pain, and decreased hearing. Occasionally, the victim complains of exquisite tenderness when the earlobe is tugged or the jaw is moved and has tender, swollen lymph glands in the neck on the affected side. In a severe case, the victim may have a fever and appear toxic.
If the victim has only a discharge without fever or swollen lymph glands, he may be treated with ear drops, such as 2% nonaqueous acetic acid (VoSoL or Domeboro Otic). Household vinegar diluted 1:1 with fresh water or with rubbing (isopropyl) alcohol (approximately 70%) can be used as a substitute. These ear drops should be administered four to five times a day and may be retained with a cotton or gauze wick gently placed into the external ear canal, or by using an expanding foam ear sponge (such as a Speedi-Wick, Shippert Medical Technologies). To avoid injuring the eardrum, do not attempt to clean out the ear with a cotton swab or similar object. The solution should be retained in the ear for a minimum of 5 minutes with each application. If there is any suggestion that the eardrum may be punctured (e.g., the presence of bleeding), do not use this solution.
If the victim has a discharge with fever and/or swollen lymph glands, the ear drops should contain hydrocortisone (VoSoL HC); he should also be given oral ciprofloxacin, erythromycin, or penicillin. An ear drop that may be useful is ciprofloxacin with hydrocortisone (Cipro HC otic suspension). Another is ofloxacin otic solution (Floxin otic) 0.3%. These ear drops are used twice a day. If the discharge from the ear is gray or black, a fungal infection may also exist, in which case tolnaftate 1% solution may be added to the treatment regimen. Aspirin, ibuprofen, or acetaminophen should be used to control fever. To avoid Reye syndrome (postviral encephalopathy and liver failure), do not use aspirin to control fever in a child under age 17.
To prevent swimmer’s ear, the external ear canal should be irrigated with VoSoL, Domeboro Otic solution (2% acetic acid, aluminum acetate, sodium acetate, and boric acid) or diluted vinegar/alcohol (described above) after each scuba dive or immersion episode in the water. Keep the solution in the canal for a full 5 minutes before allowing it to drain.
Injury to the Eardrum
If something is poked into the ear, a hard blow is struck to the external ear, a diver descends rapidly without equalizing the pressure in his middle ear (see page 404), or a person is subjected to a loud explosive noise, the eardrum may be ruptured. This causes immediate intense pain and possibly loss of hearing, along with occasional nausea, vomiting, and dizziness. If the eardrum is ruptured, cover the external ear to prevent the ingress of dirt, and seek the aid of a physician. If debris has entered the ear, start the victim on penicillin or erythromycin by mouth. Do not put liquid medicine into the ear if you suspect that the eardrum is ruptured. If the dizziness is disabling, administer medicine for motion sickness (see page 440). Use appropriate pain medication.
EYE
Foreign Body under the Eyelid and Scratched Cornea; Corneal Ulcer
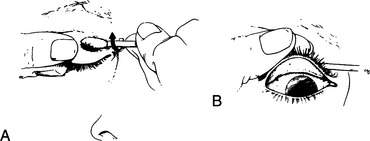
If a foreign body lodges on the cornea (the clear surface of the eye) without actual penetration of the eyeball, irrigate the eye copiously with an eyewash solution (use water if you do not have eyewash). If this is not successful, have the victim look downward, grasp his upper lid firmly by the eyelashes, and fold it up and inside out over a cotton swab (Figure 108). You can lightly grease the swab with antiseptic ointment to keep it from sticking to the skin. If you can see the foreign body on the undersurface of the upper eyelid, gently wipe it away with a cotton swab or piece of moistened cloth. If you do not see the object, check between the lower eyelid and the eyeball. After the inspection, pull down on the eyelashes to unfold the lid.
Once you have removed the object, if the victim still feels as if something is in his eye, he may have suffered a scratch on the cornea (corneal abrasion). In this case, it may help control the discomfort to patch the eye closed for 24 hours. However, never patch an eye closed if there is any sign of an active infection (pus or discharge). When the patch is removed, if there is residual pain, a gritty sensation, gooey discharge, or blurred vision, see a doctor as soon as possible. Tiny objects, such as the spine of a horse nettle (sand brier), can become embedded in the cornea and not be visible without the magnification available to an ophthalmologist.
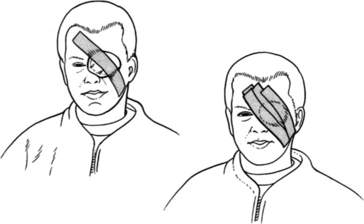
To patch an eye, a ½ in (1.3 cm) thick pad of soft cloth or bandage should be shaped to fit neatly over the eye socket, and affixed snugly to the face with tape or bandages extending across the patch onto the cheek below and the forehead opposite the affected eye (Figure 109). Prepackaged sterile elliptical eye pads are available. If only tape is available, the eyelids may be taped closed with a single small piece of tape.
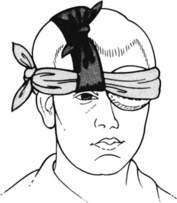
Another way to hold an eye shield, patch, or padding around the eye is with a cravat (see page 277). First, place a strip of cloth approximately 2 in (5 cm) wide and 15 in (38 cm) long over the top of the head front-to-back, so that the face-side end hangs over the uninjured eye, near the nose. Place the patch, pad, or shield over the eye and hold it in place with a cravat, which should be wrapped horizontally around the head and then tied in position on top of the hanging cloth strip. Make the first tie (single loop or half square knot) in the cravat behind the head and at the base of the skull, and keep wrapping it around, to complete the final tie (square knot) where the ends meet. If the final tie will be over an eye, shift the cravat. Pull up the ends of the hanging cloth strip and tie them at the top of the head; this should lift the cravat up off the uninjured eye (Figure 110).
Injured Eyeball
If the eyeball is perforated, there will be a combination of loss of vision (ranging from hazy vision to blindness), pain, excessive tearing, a dilated pupil, and visible blood in the eye. There may be gelatinous material extruding from the eye, and the pupil will be irregular or jagged in appearance. Do not attempt to rinse out the wound vigorously; remove obvious dirt and debris without placing any pressure on the eye. Close the eyelid gently and cover the eye with a protective shield. This can be fashioned by cutting gauze pads or soft cloth to the proper size, or by fashioning a doughnut-shaped shield with a cloth, cravat bandage, or shirt (Figure 111). Another good way to keep pressure off the eye is to cut an eye-sized hole in a stack of gauze pads and place the stack over the eye, taping or wrapping it in place. An eye shield can also be improvised by cutting off the bottom 2 in (5 cm) of a paper cup and taping it over the eye. Metal or plastic preshaped eye shields can be carried.
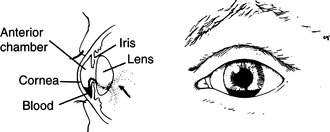
Bleeding into the Eye
If the eyeball has been struck (not torn or ruptured), there may be bleeding from small blood vessels within the eye into the clear liquid that fills the space directly behind the cornea and in front of the lens. Such bleeding is called a hyphema. It first appears as diffuse bloody (red) clouding of the fluid behind the cornea, which settles over the course of 6 to 8 hours into a clearly visible layer of blood (Figure 112). If such a condition is noted, the victim should have his eye patched closed (see the previous section) or wear sunglasses; he should be transported to an eye doctor. If possible, keep his head elevated and in an upright position and apply a rigid eye shield to protect the eye from being struck. The victim should avoid straining.
Removing Contact Lenses
If a victim is severely injured and he is wearing contact lenses, they should be removed. A contact lens remover may be used, or a slightly sticky surface of mini-marshmallow can be placed carefully against the lens to grasp it. Either soft or hard lenses can be removed by the following technique (Figure 113):
1. Slide the lens off the clear surface of the eye (cornea) over to the white area away from the nose.
2. Place one finger at the outside edge of the lower eyelid and pull the eyelid taut, while keeping the eye slightly open. This should lift the edge of the lens, so that you can pick it up. If you cannot remove the lens, position it so that as much as possible is over the white (and not on the cornea).
3. Place the lens in a container with contact lens solution, eyewash, or water (if possible, add 1 tsp, or 5 mL, of table salt per pint, or 473 mL, of water).
4. A soft contact lens can often be removed by simply pinching it gently between your thumb and index finger.
Subconjunctival Hemorrhage
Bleeding into the white of the eye (subconjunctival hemorrhage) may occur spontaneously or after coughing, straining (vigorous exertion), vomiting, or strangulation (Figure 114). The bleeding is painless, does not interfere with vision (the cornea is not involved), and does not require any therapy. The blood will absorb over a period of a few weeks, as from any other bruise. If it does not, seek the care of an eye doctor.
Red Eye
A red or pink, itchy eye is usually caused by a viral infection. Other causes include bacterial infection, insect bite or sting, allergy (see page 205), overuse of contact lenses, corneal abrasion or ulcer (see page 180), foreign body (see page 180), irritation from chemicals or smoke, snow blindness (see page 187), glaucoma (see page 190), or injury (see page 182). If the infection is caused by a virus or bacteria, symptoms include itching, tearing, watery (viral) or thick (bacterial) discharge (runny yellow or greenish pus), crusted eyelashes and lids, and swollen eyelids, which are often stuck together on awakening in the morning. You may notice a swollen lymph gland in front of the ear. If fluid collects underneath the loosely attached (to the eyeball) conjunctiva (membrane-like external lining of the eyeball), it may cause it to swell up and balloon away from the eyeball.
“Pink Eye” and Contact Lenses
“Pink eye” usually refers to a viral infection that causes redness, often accompanied by itching and a thick, yellow or green discharge. Often the lids are stuck together in the morning after sleeping. This viral conjunctivitis is believed to be highly contagious, so the sufferer should take care to not share his implements of facial washing and drying. It is not uncommon to have “pink eye” develop in one eye and then rapidly be spread to the other eye, presumably because of touching the infected eye and then transferring the infection.
1. Should a contact lens become displaced (e.g., fall out of the eye), it may be more easily lost than eyeglasses.
2. Contact lens solution can degrade or become contaminated by exposure to extreme temperatures, dehydration, or passing over dust and dirt that can accumulate on the threads of bottle caps.
3. Handling contact lenses with dirty hands can introduce bacteria and fungi to lenses or tissues of the eyes.
4. It may not be easy to change out contact lenses quickly if needed for a different refraction or environmental (e.g., sun or wind exposure) condition.
5. Once an eye becomes infected, contact lenses must be removed. They should not be reused if removed because of infection.
Blepharitis
Blepharitis is usually a chronic flaking and irritation of the skin at the base of the eyelashes, affecting both eyes. It may become infected, and be accompanied by fluctuating vision, itchy and burning eyes, and mucous discharge on awakening. Treatment is the application of bacitracin or erythromycin ophthalmic ointment thinly to the lid margins at bedtime for 4 weeks. Warm, moist compresses should be used a few times a day for 5 to 10 minutes at a time to loosen the debris, which is then gently wiped away. Artificial tears are useful to lessen the sensation of dry eyes.
Snow Blindness
High exposure to UVB can cause a corneal burn within 1 hour, although symptoms may not become apparent for 6 to 12 hours. Symptoms include excessive tearing, pain, redness, swollen eyelids, pain when looking at light, headache, a gritty sensation in the eyes, and decreased (hazy) vision. Similar symptoms occur when the surface of the eye is physically scratched (corneal abrasion). Treatment consists of patching the eye closed (see page 181) after instilling a few drops of ophthalmic antibiotic solution (such as moxifloxacin 0.5%, sodium sulamyd 10%, or gentamicin), because the surface of the cornea will regenerate spontaneously in 24 to 48 hours. It is important to check the eye first for a foreign body (see page 180). After patching, the eye must be rechecked in 24 hours. If the eye appears to be infected with pus, it should be left unpatched; administer a topical antibiotic solution (see page 182) three to four times a day, and have the victim wear sunglasses. Pain medicine should be used as appropriate. If both eyes are involved, only the more severely affected eye should be patched, so that the victim can continue to make his way.
Eye Allergies
Seasonal allergies commonly involve the eyes, often causing conjunctivitis. See page 185.
Vitreous Detachment
Floaters are small spots, lines, clouds, cobwebs, or veils that move around in the field of vision, especially when the eyes move. They can be in one or both eyes, but usually show up in one eye at a time. They are easiest to see when one looks at the sky or against a plain white background. Floaters are caused by tiny opacities inside the vitreous, which is the gel that fills the inside of the eyes. In childhood and adolescence, the vitreous gel is clear, so that floaters are not seen. In adulthood, floaters can develop when the vitreous gel forms small clumps as part of the aging process. As light passes from the outside of the eye, through the cornea and lens, and then through the vitreous gel before it strikes the retina to record an image, the floaters can cast shadows on the retina. Floaters are annoying, but not dangerous, particularly if they have been present for a long time.
In terms of exercise, it is wise to avoid sudden head or eye movements, so no jogging or swimming with rapid head movements, wrestling, significant straining, and so on. Until the vitreous separation process is complete, a person should try to turn the head to look in a direction, rather than hold the head in a fixed position and move the eyes. All of this may be difficult in a precarious situation, such as rock climbing or kayaking, but one should just do the best he can given the particular circumstances.
Glaucoma
Glaucoma is a condition in which the pressure of the fluid within the eye is elevated. If this happens suddenly, the pressure can injure the nerves within the eye that record vision; blindness can result. Symptoms of an acute attack of glaucoma include severe pain, blurred vision or “halos” around lights, clouding of the cornea, intense reddening of the white of the eye, a dilated pupil that doesn’t react to light, nausea, vomiting, and headache. The victim of acute glaucoma is truly miserable. If an attack occurs, the victim should be kept in a sitting or standing position and rushed to an ophthalmologist. If the victim is carrying medication(s), instill a drop of pilocarpine or carbachol and (depending on which medications are carried by the victim) a drop of timolol (or betaxolol, carteolol, levobunolol, or metipronol), latanoprost (or travoprost, unoprostone, or bimatoprost), brimonidine (or apraclonidine), and/or dorzolamide (or brinzolamide) in the affected eye. If you are distant from care, and acetazolamide (Diamox) is available and there are no contraindications to its use (see page 336), it may be administered in a dose of 125 mg, 250 mg, or 500 mg sustained release by mouth twice a day.
Injured Eyelid
If the eyelid is injured, wash the eye carefully, apply bacitracin or mupirocin ointment, and then patch the eye closed (see page 181). If the eye cannot be covered with eyelid, apply a thick layer of antiseptic ointment to the eyelid and exposed eyeball and patch the eye. Seek immediate medical attention.
Sty
A sty is a small abscess (see page 241) that develops in one of the glands at the base of an eyelash. The infection causes the eyelid to swell, redden, and become painful. The victim may notice increased tear production and the sensation of a foreign body in the eye. Usually, the sty comes to a head on the outside of the lid, but occasionally it will come to a head inside. If a sty begins to develop, the victim should hold warm, moist compresses to his eyelid for 30 minutes four times a day to soften the abscess. It will either disappear or enlarge and come to a head. Never squeeze an abscess on the face. If the sty enlarges, comes to a head, and is extremely painful or interferes with vision, but will not open spontaneously, it can be carefully lanced with a sharp blade or needle to drain the pus. A physician should perform this procedure, unless the victim is more than 48 hours from medical attention and the infection has worsened to the extent that there is progressive swelling of the eyelid that impedes vision, or of the cheek or forehead. In this event, also administer dicloxacillin, erythromycin, or cephalexin. After the sty is incised, the pus can be expressed gently by pressing on opposite lateral sides with two cotton-tipped applicators.
Eyelid Infection and Periorbital Cellulitis
Redness and swelling of the eyelid and “soft” tissues around the eye (eyebrow, upper cheek) caused by infection is known as periorbital (around the orbit, or eye) cellulitis. This is extremely serious and must be treated aggressively, because the infection can spread to create an abscess in the brain. Treatment consists of administration of an antibiotic (moxifloxacin, levofloxacin, ciprofloxacin, cephalexin, clindamycin, amoxicillin-clavulanate, dicloxacillin, or erythromycin) and immediate evacuation to a hospital. To differentiate periorbital cellulitis from the swollen eyelids associated with an allergic reaction, note that with cellulitis, the onset will have been more gradual (typically associated with a less severe eye infection, such as conjunctivitis, or a local infection such as a sty or pimple), the affliction is only on one side, there are fever and chills, the soft tissues are painful, there is headache, and there is often a purulent (with pus) discharge from the eye. With an allergy, the eye is more “puffy,” the onset is sudden, the eye is itchy and watering, there is no purulent discharge, and there are associated signs and symptoms of allergy (skin rash, generalized itching, swollen lips, etc.) (see page 66).
NOSE
Nosebleed
Nosebleed is classified as anterior or posterior, depending on where it originates within the nose. Generally, anterior nosebleed is less serious, because the victim will usually drain blood outward through the nostrils. Posterior nosebleed is more difficult to control, and the victim often drains blood back into the throat, with coughing and potential choking. Anterior nosebleed is more common and can usually be managed outside of the hospital. If you suspect a posterior nosebleed (bleeding from the nose accompanied by brisk bleeding into the throat, so that a lot of blood is continually swallowed, particularly after the anterior bleeding has been controlled), immediately evacuate the victim to a hospital.
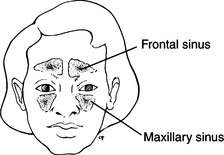
Sinusitis
The sinuses are spaces filled with air and lined with mucus-producing tissues found in the front of the skull and in the bones of the face (Figure 115). Sinusitis is a blockage and infection/inflammation of the lining of the sinuses, usually caused by bacteria, and characterized by nasal congestion, headache, fever, decreased ability to smell, and tenderness in and over the involved sinus, with or without foul yellow or green discharge from the nose. Occasionally, the pain radiates to the eyes, bridge of the nose, and upper teeth. It is often made worse by bending forward. A person with sinusitis can become quite ill and suffer from excruciating headache, nausea, vomiting, and chills. Treatment involves the administration of an antibiotic (first choice is amoxicillin-clavulanate, amoxicillin, azithromycin, or telithromycin; other choices include moxifloxacin, levofloxacin, clarithromycin, doxycline, ciprofloxacin, trovafloxacin, levofloxacin, moxifloxacin, cefuroxime axetil, cefpodoxime, cefproxil, cefdinir, loracarbef, or erythromycin) and decongestants (oral pseudoephedrine and a nasal spray: phenylephrine 0.25% [Neo-Synephrine ¼%] or oxymetazoline 0.05% [Afrin]), as well as warm packs over the affected area(s). Don’t use a topical decongestant for more than 3 or 4 consecutive days, to avoid “rebound” swelling of the inside of the nasal passages from chemical irritation and sensitization to the drug. Antihistamine drugs should not be routinely used, because they may dry out nasal and sinus secretions. A person suffering from sinusitis should avoid rapid changes in ambient external pressure (such as scuba diving or air travel in unpressurized aircraft).
THROAT
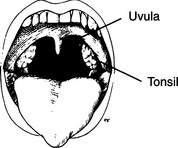
Sore Throat and Tonsillitis
Sore throat (pharyngitis) is a common complication of viral infections (the common cold, infectious mononucleosis), breathing dry air (“altitude throat”), or primary bacterial throat infection (“strep throat”). Symptoms of an infection include pain with swallowing, fever, swollen lymph nodes (“swollen glands”) in the anterior neck, red throat, swollen tonsils, pus over the tonsils and throat (Figure 116), headache, fever, abdominal pain, and nausea and vomiting.
Because the symptoms of a viral throat and tonsil infection and a bacterial strep (group A beta-hemolytic streptococcus [GABHS]) throat are frequently identical, it is hard to make the differentiation without a throat-swab “rapid strep test” or bacterial culture. Below age 3 years, a child rarely has a strep throat; in young adults, the presence of strep throat in the presence of classic symptoms (fever, pus, and swollen tonsils and lymph glands in the neck) is roughly 50%. However, because the potential complications (kidney or heart disease) of an untreated strep throat in a young person outweigh the complications of antibiotic use, it is advisable to treat with penicillin (or amoxicillin), cefadroxil, or erythromycin for a full 10-day course, or with azithromycin or clarithromycin for 5 days. If none of these drugs is available, clindamycin or cephalexin can be used. Even if the victim improves after 2 to 3 days, the antibiotic should be taken for the full course.
If a person develops an acute sore throat that rapidly becomes extremely uncomfortable (severe pain, difficulty swallowing), a single dose of dexamethasone or its equivalent (see page 340) may be given along with an antibiotic, assuming the victim can swallow the medications. This may help decrease inflammation, but should not be given routinely for a “nontoxic,” or run-of-the-mill, sore throat. If someone with a sore throat has a high fever associated with difficult or noisy breathing, altered (e.g. hoarse) or muffled voice (“like talking with a potato in his mouth”), drooling, stiff neck, or any visible swelling (bulging) in the back of the throat, he should be made as comfortable as possible and transported immediately to a hospital. Such a condition may indicate an abscess (see page 241) in the back of the throat or next to a tonsil, infection and inflammation of the epiglottis (epiglottitis), or massively swollen tonsils. Any of these may rapidly obstruct the airway.
A sore throat can be caused by overgrowth of the fungus Candida albicans, which leads to a condition known as “thrush.” This occurs most commonly in persons who are immunosuppressed, have recently taken broad-spectrum antibiotics, use inhaled or oral steroids, wear dentures or orthodontic appliances, have diabetes, or are elders. Symptoms include burning in the mouth and throat, white patches on the palate and in the mouth and throat, painful swallowing, heartburn, drooling, and loss of appetite. If thrush is suspected, it can be treated with nystatin (Mycostatin) oral suspension, swished and swallowed four times a day for 2 weeks, or with nystatin oral lozenges 4 to 5 times daily for 2 weeks.
Infectious Mononucleosis
Mononucleosis (“mono”) is a viral disease characterized by low-grade (less than 101°F, or 38.3°C) fever, sore throat, swollen lymph glands (mostly in the neck, but occasionally in the armpits or in the groin), headache, fatigue, and, occasionally, skin rash, dark urine, muscle aching, and an enlarged spleen. Treatment consists of increased rest (it sometimes requires weeks for a normal energy level to return) and elimination of any physical activity that requires heavy exertion or risks abdominal injury (and thus rupture of the spleen). The diagnosis is confirmed by a blood test; until that can be performed, the victim should be treated for a possible strep throat (see page 195). Because infectious mononucleosis can be spread via saliva, infected people should avoid sharing eating utensils and towels.
MOUTH
Fever Blisters (Cold Sores)
Crops of blisters on the face, mouth, and lips that break out in times of stress (viral illness, emotional crisis, intense sun exposure) are often caused by reactivated herpes simplex virus (usually HSV-1). The blisters often weep and may become infected. Unfortunately, there is little to do for these when they first appear except keep them clean and dry. If the skin cracks and becomes painful, the blisters may be lubricated with bacitracin or mupirocin ointment. Anesthetic ointment can be used if it is helpful. Further sun exposure should be prevented with an adequate lip sunscreen (see page 228) of sun protection factor (SPF) 20 or greater.
All herpes viruses are contagious. During times of visible blisters, eating and drinking utensils should not be shared. To maximize prevention, use a high-SPF sunscreen and consider taking acyclovir (Zovirax) (400 mg twice daily by mouth) the day before and during intense ultraviolet light exposure.
Black Tongue
Black “hairy” discoloration of the tongue may be caused by excessive growth of the papillae of the tongue. It may be associated with topical or systemic antibiotics, poor mouth and dental hygiene, smoking, drinking alcohol, or even certain mouthwashes. Usually, the only symptom is the discoloration, but some patients suffer nausea, bad breath, or altered taste of food. Treatment consists of brushing the tongue with a soft brush. Black hairy tongue may be due to the presence of a yeast (e.g., Candida albicans) infection and/or the use of certain medications, such as bismuth (found in Pepto-Bismol) or doxycycline. If the discoloration does not resolve spontaneously, it may be treated with clotrimazole (10 mg troche dissolved in the mouth 5 times a day for 14 days) or with a 3-day treatment of fluconazole (150 mg by mouth once a day).
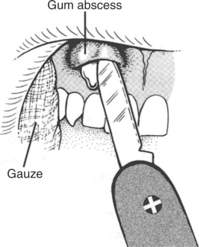
Toothaches and Tooth Infections
If an abscess (infection) (see page 241) develops in the root of the tooth or in the gum, there may be associated fever; swelling of the gum, jaw, or palate; and swollen lymph glands under the jaw and in the neck. If the abscess extends, the cheek and side of the face may swell. The victim should be started on penicillin, metronidazole, cephalexin, or erythromycin, and given appropriate pain medication. If there is a soft, pointing abscess in the gum adjacent to a tooth and the victim is suffering, the abscess can be punctured with a scalpel or knife and drained (Figure 117). Hold snow or ice against the gum to provide some anesthesia before the incision. A gauze or cotton wick should be placed into the abscess cavity for a day or two (see page 243). After this procedure, the area should be rinsed with salt water after each meal, at least four times a day.
Another remedy for a cavity caused by decay or a lost filling is to fill the cavity with temporary filling material from a dental kit. Such materials include Cavit, which requires no mixing. It is applied directly to the tooth, using a wetted toothpick or cotton-tipped applicator as a packing and shaping instrument. Intermediate Restorative Material (IRM) is prepared by adding a few drops of clove oil to powdered zinc oxide to make as dry a “dough” as possible. Zinc oxide–eugenol combination cements are advantageous in that they have an anesthetic effect and can be mixed to different consistencies, depending on whether they are to be used as filling material or adhesives. However, the liquid can leak from its container, and the cement is sticky and more difficult to work with than Cavit.
Broken, Displaced, or Lost Tooth
If a tooth is cracked (with the root still present and in place), there is little for the victim to do other than keep his mouth clean and avoid contact with extremes of temperature. If air, saliva, the tongue, or temperature change coming into contact with an exposed nerve causes intolerable pain, a temporary cap (shield) can be created by mixing melted paraffin (candle wax) with a few strands of cotton. When the mixture begins to harden but can still be easily molded, press a wad onto the tooth, using the teeth on either side as anchors. A cap can also be fashioned from Cavit or IRM (see the discussion above).
If the socket of a broken or lost tooth continues to bleed, apply direct pressure by having the victim bite on a gauze pack for 30 minutes. If there is a large blood clot, remove it, and then apply pressure. Keep the head elevated. Avoid rinsing, spitting, tooth brushing, and tobacco use for 24 hours. Gentle rinses with warm saltwater can be started after that time period. If the bleeding does not stop after several hours, biting on a dry tea bag (tannic acid) may help. “Dry socket” may occur 2 to 4 days after a tooth is lost. This is characterized by pain, foul odor, and a bad taste. Inspection of the tooth socket may show exposed bone. Treatment is gentle saltwater rinses followed by packing with a strip of eugenol-soaked gauze. The pack should be changed every 1 to 2 days until the symptoms are relieved, which may take up to 10 days. During this period, do not ingest alcohol or carbonated beverages.