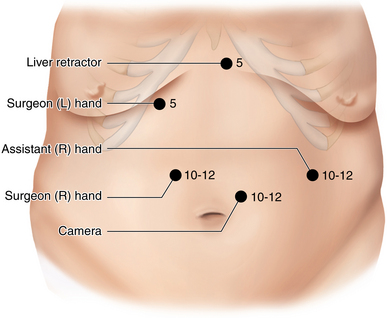
CHAPTER 25 Handsewn gastrojejunal anastomosis
Step 2. Preoperative considerations
♦ For details regarding patient preparation, anesthetic considerations, room set-up & patient positioning, see Chapter 24.
Step 3. Operative steps
Creation of pouch
♦ For the construction of gastrojejunostomy (following completion of jejunojejunostomy), attention is turned to the upper abdomen for the retraction of the left lobe of the liver. A Nathanson retractor is placed in the epigastrium to elevate the liver, and the gastroesophageal junction is exposed.
♦ The angle of His is mobilized with a Harmonic scalpel.
♦ The pars flaccida of the gastrohepatic ligament is opened.
The lesser omentum, located approximately 6 cm from the GE junction, is divided with Harmonic scalpel up to the gastric wall of the lesser curvature.
♦ The stomach is divided transversely using a 45-mm endoscopic gastrointestinal stapler transversely.
♦ This is followed by additional vertical firings of 60 mm Gold cartridges up to the previously mobilized angle of His. A slim gastric pouch (approximately 15 cc’s) is created entirely based on the lesser curvature.
Gastrojejunal anastomosis
♦ The proximal end of the Roux limb is brought to the upper abdomen (usually in an antecolic, antegastric manner).
♦ A running backwall suture line is created using a 2-0 Vicryl suture (~20 cm in length). This is created by lining up the antimesenteric side of the Roux limb to the pouch staple line. The suture is run from the patient’s left side corner to the right corner and the remaining suture and needle are saved.
♦ An enterotomy is made into the gastric pouch and the Roux limb (∼1 to 1.5 cm in length) a few millimeters away from the running backwall suture line.
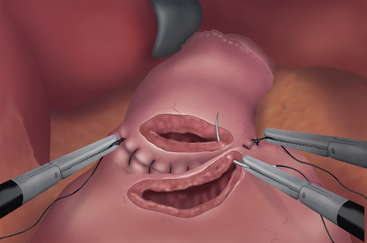
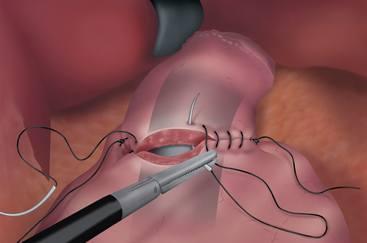
♦ An second, inner, running suture line is created using 2-0 Vicryl which is started at the patient’s left side corner of the open enterotomy (Figures 25-2, 25-3, and 25-4).
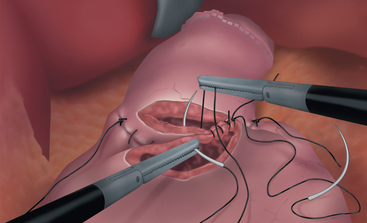
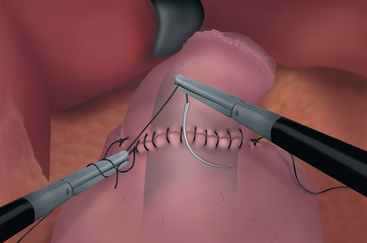
♦ Another 2-0 Vicryl suture is used to close the inner layer anteriorly. Prior to completion of the inner layer closure, a 34 French (1 cm in diameter) large orogastric tube is passed across the anastomosis into the Roux limb to be used as a stent (Figures 25-5).
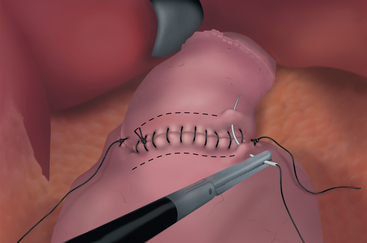
♦ The inner layer closure is completed by bringing the two sutures onto the anterior aspect of the anastomosis and tying them to each other (Figure 25-6). Needles are cut and removed.
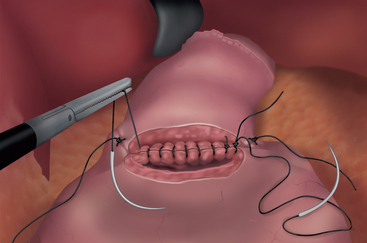
♦ The previous outer layer Vicryl suture is then used to continue anteriorly as Lembert sutures to reinforce the inner layer (Figure 25-7).
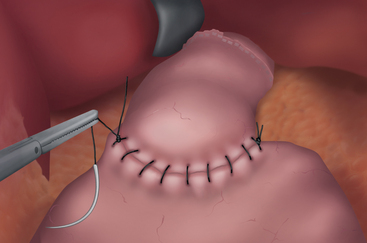
♦ This can be completed by starting a separate second suture beginning from the corner and tying in the middle of the anterior aspect of gastrojejunostomy (Figure 25-8).
Leak test
♦ The completed anastomosis is then tested for its integrity. The tip of the Ewald tube is pulled back just beyond the anastomosis, and the Roux limb is occluded with an atraumatic grasper. The patient is placed in the Trendelenburg position, and the left upper quadrant is flooded with normal saline to immerse the anastomosis. Air is introduced into the Roux limb through the tube until adequate inflation of the gastric pouch and proximal Roux limb is observed.
♦ If leakage (seen as bubbling) is noted, the area is repaired with additional nonabsorbable sutures until no further air leak is noted.
Step 5. Pearls and pitfalls
♦ To minimize the risks of anastomotic ulcers and stricture, at least the inner layer closure is done using absorbable sutures.
♦ The aperture of the anastomosis is regulated by closing the enterotomy defect over a predetermined caliber bougie or an orogastric tube. Care should be taken to avoid suturing into the tube which can result in disruption of the entire closure.
♦ Back-hand suturing in the corners may allow more precise suturing if forehand stitching appears awkward in orientation.
♦ The tension on the running suture is maintained by the assistant throughout the closure process to avoid loosening of the closure and thus, potential anastomotic leakage. Prior to tying the knots, the entire suture is cinched down to further eliminate potential gaps.