8 Handheld Echocardiography
Although technology has transformed almost all aspects of our daily lives, the bedside cardiac physical examination uses technology that is almost 200 years old. In 1816, embarrassed to examine an obese young woman by putting his head to her chest, René Théophile-Hyacinthe Laennec rolled a sheet of paper, then placed one end over her precordium and the other to his ear. Thus, the stethoscope was born.1 The sphygmomanometer for measurement of blood pressure dates back to 1881, when it was invented by Samuel Siegfried Karl Ritter von Basch. It is with these two ancient tools that most physicians approach a patient at the bedside to this day. In the interim, the explosive growth of medical technology has spawned relatively inexpensive, miniature ultrasound machines, which can be taken to the bedside and allow immediate imaging across several medical specialties.
Background
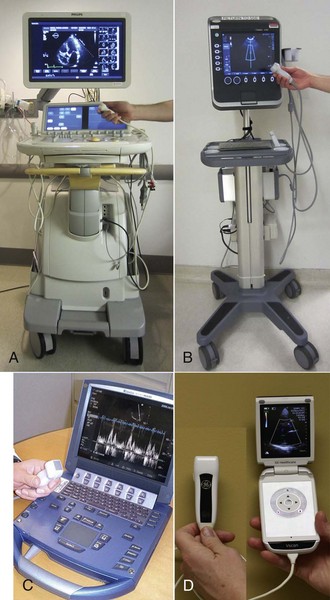
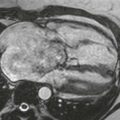
In 1978, J. R. Roelandt proposed the first miniaturized HCU system.2 Since that time, bulky keyboards, large monitors, and video recorders have now been replaced by touch pads, flat screens, and digital storage devices. The American Society of Echocardiography defines an HCU device as a small ultrasound machine typically weighing less than 6 pounds that can obtain images and data.3 Since that publication in 2002, advances in ultrasound technology have incorporated all the capabilities expected of a full sized system into these small machines (Fig. 8-1).4–6
Types of Echocardiographic Instruments
Currently, there are four basic types of echocardiographic systems (Table 8-1):
1. Large, very expensive systems carrying the most advanced instrumentation, capable of two-dimensional (2D), M-mode imaging, designated contrast settings, color flow Doppler, pulsed-wave (PW) and continuous-wave (CW) Doppler, tissue Doppler imaging, tissue harmonic imaging, speckle strain imaging, stress echocardiography formats, and broadband multifrequency imaging with image processing and digital storage, as well as volumetric (three-dimensional [3D], four-dimensional [4D]) imaging and transesophageal, intravascular, and intracardiac echocardiography. These systems typically are based in a hospital echocardiography laboratory or large office practice, with an instrument cost over $250,000.
2. Compact, smaller version of the full-sized systems that are more portable and less expensive, but have most of the features available on larger systems. Some are capable of transesophageal echocardiography (TEE) but lack volumetric (3D) imaging. With a compact system, resolution and penetration may be less robust with a lower cost between $100,000 and $150,000. These systems are usually located in an echocardiography laboratory or cardiology office but also are offered in smaller, battery-powered options that can be attached to a cart or separated and carried for portability.
3. Handheld or hand-carried ultrasound (HCU) devices are small, light, battery powered, less expensive systems with good 2D imaging quality and full Doppler capabilities, often with digital and wireless communication, some with stress and TEE options. These systems can be cart mounted or hand carried and may be in an office, emergency department, or hospital setting to provide “point-of-care” ultrasound with multiprobe capability. HCU systems cost between $50,000 and $100,000, depending on options.
4. Palm-sized devices are very small. They can truly be held in one hand and viewed on a small screen and have potential as a smartphone application. These devices can image in 2D, with a caliper for measurement, usually with no or limited color flow Doppler and no electrocardiographic gating. They are relatively inexpensive for their size and capability, around $10,000, and can be used for point-of-care screening or as a true “echo-stethoscope.”
TABLE 8-1 Classification of Currently Available Echocardiography Machines According to Size and Function
| Echocardiography Machines | Capabilities |
|---|---|
| Stationary high-end systems | Full range of standard echocardiographic modalities and measurements (MM, 2D, PW, CW, Color, TDI, TEE), and advanced modalities (3D, contrast) |
| Mobile (smaller machines on wheels, middle range technology) | Full range of standard echocardiographic modalities and measurements (MM, 2D, PW, CW, Color, TDI, TEE) |
| Portable (small machines that can be carried by a person) | Basic, standard echocardiographic modalities and measurements (MM, 2D, PW, CW, Color) |
| Handheld or pocket-size imaging devices | Limited functions (2D, Color) and measurement package |
Color, Color Doppler; MM, M-mode; PW, pulsed ware; TDI, tissue Doppler imaging.
From Sicari R, Galderisi M, Voigt JU, et al: The use of pocket-size imaging devices: a position statement of the European Association of Echocardiography. Eur J Echocardiogr 12:85-87, 2011.
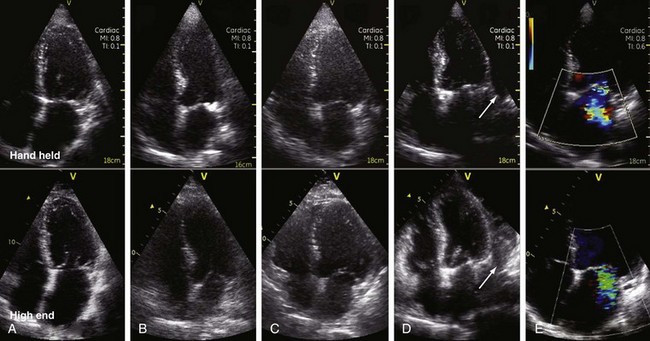
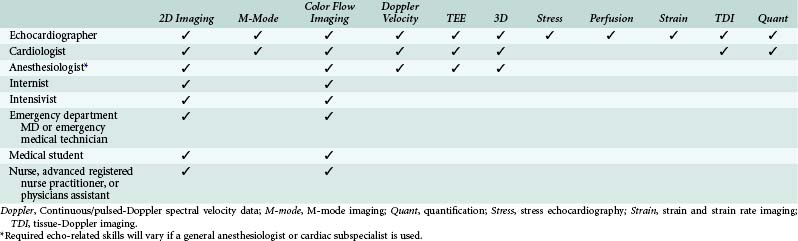
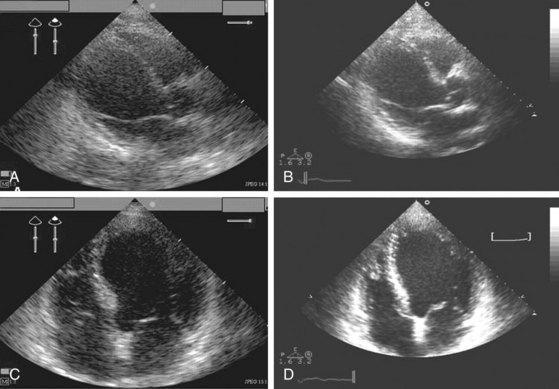
These echocardiographic systems can be separated on the basis of performance capability, size, weight, and cost. Some of the smaller systems can perform a full examination, whereas the palm-sized units can be applied for screening of left ventricular (LV) function, wall thickness, chamber size, hypertrophy, pericardial effusions, and abdominal aortic aneurysms (Fig. 8-2). Ultimately, the choice of system to use will vary with the goal of the examination, the skill and experience of the persons performing the imaging, and its interpretation (Table 8-2). Typically, complete and compact echocardiography systems are used by cardiologists in the context of an echocardiography laboratory. The focus of this chapter is the use of hand-carried and palm-sized echocardiography systems outside the echocardiography laboratory by health care providers in other specialties. The two most important considerations in the clinical use of these smaller, readily accessible, heavily promoted systems are (1) the technical performance of the imaging device and (2) the appropriate level of skill and training to acquire and interpret the images.
Reliability and Accuracy
The reliability and accuracy of the hand-carried ultrasound devices have been validated in studies comparing their performance to full-size systems with images obtained by skilled technicians or physicians. Vourvouri and colleagues7,8 demonstrated greater than a 90% concordance between results using an HCU and a standard full-size system in the echocardiographic evaluation of LV size and function with older-generation hand-carried devices including the OptiGo (Philips Healthcare, Andover, Mass.) and Sono-heart (Sonosite, Bothell, Wash.). Vourvouri and co-workers9 also imaged 300 consecutive patients referred to a cardiologist with a hand-carried device. Agreement between the HCU device (OptiGo) and the standard system for the detection of major abnormalities was excellent (98%). However, even this level of agreement may be suboptimal in the clinical setting, because the HCU did miss 4% of the major findings.
Because of limitations in penetration and resolution, HCUs may underestimate severity of wall motion abnormalities in patients with poor ultrasound tissue penetration, which is often a problem in overweight or obese patients. In general, the quality of the images obtained with an HCU device correlates directly with the skill and experience of the personnel acquiring and interpreting the images. Cardiology fellows had 100% agreement between HCU and conventional echocardiography on qualitative assessment of LV systolic function and a 94% concordance for LV end-diastolic dimension and interventricular septal thickness, with an ultrasound imaging time of only 6 ± 2 minutes.10 Therefore, with proper training, HCU devices represent a valuable alternative to standard echocardiographic systems for well-trained personnel in some specific clinical applications.
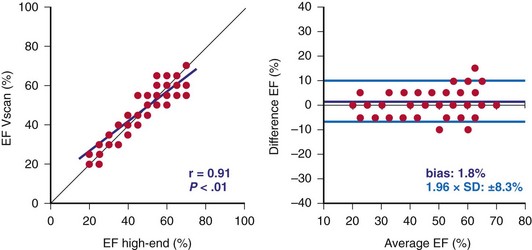
Even the smallest palm-sized devices, potentially true cardiac “stethoscopes,” have been evaluated against more sophisticated echocardiographic systems. Dalla Pozza and colleagues11 used three small ultrasound devices in a pediatric population. The two larger HCU systems (a laptop-sized Philips p50 and a compact Philips CX 50) had excellent image accuracy (93%) compared to full echocardiography instruments; however, the palm-sized device (ACUSON P10, Siemens Healthcare, Malvern, Pa.) had only a 64.5% accuracy. Prinz and Voigt12 compared the diagnostic accuracy of a palm-sized device (Vscan, GE Healthcare), used for imaging by an experienced cardiologist in 349 routine patients with varying LV function, to that of two laptop-sized HCU systems (either a Vivid 7 or E9, GE Healthcare). The palm-sized HCU showed excellent correlation in the evaluation of regional wall motion, visual ejection fraction, LV wall thickness and dimensions, and valve regurgitation (Fig. 8-3). These studies corroborate that HCUs and even palm-sized devices can be used by experienced, qualified sonographers and physicians for routine clinical cardiac imaging and may represent a valuable alternative to standard echocardiographic systems, for certain applications.
Ultrasound “Stethoscope”
The concept of a stethoscope is that the physician listens to the patient’s heart sounds to deduce clinical and hemodynamic information from the noise created by blood flow and valve motion. Echocardiography has the potential to work like a stethoscope by using (ultra)sound waves to create images of the heart and visualization of blood flow that provide more accurate data than can be obtained from the acoustic sounds appreciated with a conventional stethoscope. Integrated into the physical examination, the HCU or palm device, as an ultrasound stethoscope, facilitates rapid identification of cardiac abnormalities (e.g., valve disease, chamber dilation, hypertrophy, pericardial effusion, or wall motion abnormalities). This can eliminate more sophisticated, costly studies and expedite appropriate therapeutic interventions (Figs. 8-3 to 8-5).13–15 The Naples Ultrasound Stethoscope in Cardiology study16 demonstrated that whereas the physical examination diagnosed cardiac abnormalities in 38.2% of patients, the addition of a palm-sized echocardiography examination increased the detection of cardiac abnormalities to 69.7%. The goal of promoting these very portable palm-sized or HCU systems is not to replace the comprehensive, carefully done Doppler echocardiographic examination, a detailed anatomic and hemodynamic evaluation, but to complement and improve the physical examination.17
The European Society of Echocardiography recommended indications for palm-size echocardiography devices reflect this approach (Box 8-1).18 In addition to this limited list of indications, they further recommend:
• HCU imaging results should be included in the physical examination documentation and the images stored according to rules for other imaging data at each institution.
• Training and certification in HCU is recommended for all users, specific to the scope of practice for each user.
• Patients should be made aware that an HCU examination does not replace a complete echocardiogram.
Box 8-1
Summary of Indications for Pocket-Size Devices
1. Complement to a physical examination in the coronary and intensive care unit
2. Tool for a fast initial screening in an emergency setting
3. Cardiologic counselling in outpatient health care facilities and hospitals
4. First cardiac evaluation in ambulances
5. Screening programs in schools, industry, and community activities
6. Triaging candidates for a complete echocardiographic examination
From Sicari R, Galderisi M, Voigt JU, et al: The use of pocket-size imaging devices: a position statement of the European Association of Echocardiography. Eur J Echocardiogr 12:85-87, 2011.
Education and Training Guidelines and Requirements
Both the American Society of Echocardiography (ASE) and the American College of Emergency Physicians (ACEP) have produced written guidelines and documents on the training of physicians using cardiac ultrasound and echocardiography. Comprehensive echocardiography training guidelines have been described by the ASE and are documented in a position paper, the American College of Cardiology/American Heart Association Clinical Competence Statement on Echocardiography.19 These training guidelines are applicable for those physicians and practitioners who perform comprehensive echocardiography. However, the training requirements for comprehensive echocardiography exceed the training needed for point-of-care echocardiography in many clinical situations. For example, the requirements for emergency physicians who are performing focused ultrasound in the emergent setting are limited to the specific diagnoses being evaluated.20 Similarly, intensivists have a limited scope of practice compared to a comprehensive echocardiographic examination with a correspondingly limited training scope and duration.21
For specific HCU training, the ASE recommends at least Level 1 training (performing 75 examinations and personally interpreting 150 examinations). However, this time commitment is usually practical only for cardiology training programs. There is no consensus on the appropriate training protocols required for HCU for noncardiologist and non–emergency department use. Various focused transthoracic echocardiography (TTE) training programs for intensivists, emergency-department physicians, anesthesiologists, hospitalists, and other medical specialties have been proposed, varying from a few hours to a few days.22–24 As expected, a meta-analysis found that the accuracy of hand-carried echocardiography depended on the training time allocated and level of skill of the personnel performing the echocardiogram, ranging from medical students to cardiologists.25 Ultimately, each professional specialty society will be responsible for maintaining the integrity of their training protocols and for ensuring the responsible practice and use of these imaging techniques.
Medical Students
The use of HCU by medical students completing abbreviated training programs has been evaluated in several studies and has been found to be additive to the history and physical examination. Diagnoses by medical students trained on an HCU system (OptiGo) for 18 hours were compared with those of a board-certified, experienced cardiologist using a standard physical examination.26 Medical students performing echocardiography correctly identified 75% of abnormal findings compared with 49% by a cardiologist’s physical examination as adjudicated by findings using a standard echocardiographic system. Another study showed that a medical student echocardiography curriculum, which included 60 hours of didactics and 40 hours of supervised imaging, resulted in a significant improvement in the accuracy of bedside diagnosis.27
Medical Residents
In a formal training program of noncardiologists using HCU by Alexander at Duke, 20 medical house officers participated in a standardized 3-hour HCU training program (30 minutes of introduction to ultrasound and the HCU device, 75 minutes of case reviews, and 75 minutes of hands-on practice).28 The study demonstrated that the HCU substantially improved the assessment of LV function and pericardial effusion over history and physical examination, but was less effective for aortic valve disease. This study suggested that despite having only a 3-hour training period, medical residents can use HCU echocardiography to substantially improve their assessment of LV function and pericardial effusion with an acceptable level of accuracy compared with standard echocardiography. Kimura and associates10 devised an HCU curriculum consisting of a 1-hour lecture on cardiac physical examination and a 1-hour session of echocardiogram instruction for internal medicine residents and successfully improved their ability to accurately determine LV function.
Emergency Physicians
The ACEP Recommendations for Emergency Physicians who are performing Focused Ultrasound in the Emergent Setting (FOCUS)20 are available online (http://www.acep.org/) and include both a training-based and a practice-based pathway. Residency training in ultrasound should include appropriate verification. The practice-based pathway includes didactic education plus performance of 25 ultrasound studies with confirmatory studies for each primary indication or a total of 150 studies for general emergency medicine ultrasound privileges. The ACEP also encourages point-of-care ultrasound for many other organ systems other than the heart. Their guidelines recommend 80 hours of general ultrasound instruction throughout residency and performance of 25 to 50 cardiac ultrasound examinations.29 Wright and colleagues30 suggest that because of the steep learning curve for echocardiography, emergency-department physicians with an interest in TTE at point of care should establish a quality assurance relationship with the cardiology echocardiography section of their institution.
Intensivists
Intensivists who supervise care of a hospital’s most complex and unstable patients have also integrated general and cardiac ultrasound into their armamentarium. Manasia and co-workers31 found that after ten 1-hour tutorial sessions, intensivists who performed limited echocardiograms to assess LV function, volume status, and source of hypotension in 90 patients in the intensive care unit successfully performed a diagnostic limited TTE in 94% of patients and interpreted them correctly independently in 84% of patients. Importantly, new cardiac information provided a change of management in 37% of patients and additionally useful information was found in 41% of patients.
Recommendations
All of these studies on the type and duration of training needed for HCU examination by physicians at various levels of training and in various specialties will be helpful in defining the standards for the use of HCU by health care providers. Clearly we need evidence-based recommendations for education and training of health care providers, tailored to the scope of practice in each specialty. We also need to work toward methods of competency testing and credentialing of practitioners as HCU becomes more widespread. In a recent editorial in Chest,32 Schmidt calls for all intensivist training programs to incorporate a formal ultrasound curriculum for their fellows, including hands-on guidance. He cautions that “with the coming boom in ICU [intensive care unit] ultrasound, it is essential that skills spread as fast as the machines.”
Clinical Applications
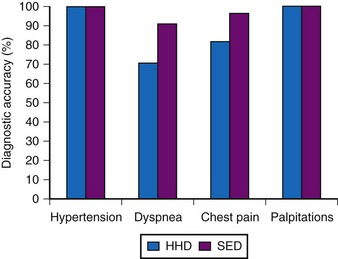
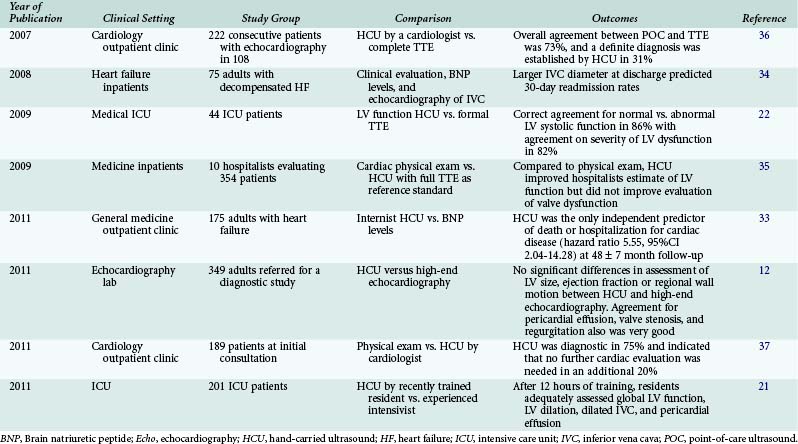
The application of HCU is undergoing active investigation in several clinical settings. The goals of HCU in each setting depend on the specific clinical issues, and the long-term effect of point-of-care ultrasound is in evolution (Fig. 8-4). However, studies already support the use of HCU to improve the diagnosis, treatment, and risk stratification of heart failure in outpatient and inpatient settings and to improve the use of full echocardiographic examinations (Table 8-3).12,21,22,33–37
Emergency Department
The ASE and ACEP recently published a consensus statement that defines the important role of focused cardiac ultrasound (FOCUS).20 FOCUS is a time-sensitive evaluation of the symptomatic patient that includes assessment for pericardial effusion and evaluation of chamber size, global cardiac function, and patient volume status. Intravascular volume may be assessed by chamber size, function, inferior vena cava size, and respiratory change. The examination may also guide emergency pericardiocentesis and transvenous pacemaker placement. The consensus statement emphasizes the complementary role of FOCUS to that of comprehensive echocardiography. HCU can supplement the physical examination, as well as facilitate the rapid triage of emergency department or intensive care patients (Box 8-2).
Box 8-2
Goals of Focused Cardiac Ultrasound in the Symptomatic Emergency-Department Patient
Assessment for the presence of pericardial effusion
Assessment of global cardiac systolic function
Identification of marked right ventricular and LV enlargement
Intravascular volume assessment
From Labovitz AJ, Noble VE, Bierig M, et al: Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr 23:1225-1230, 2010.
Intensive Care Unit
The FREE (focused rapid echocardiography evaluation) examination, which incorporates a rapid assessment of LV and RV function and relative inferior vena cava size and its respiratory change to assess overall volume status and cardiac status, was feasible in 80% of 53 patients in a trauma unit, 85% of whom were mechanically ventilated.38 Overall, 54% had a change in clinical management based on the FREE examination.
Internal Medicine
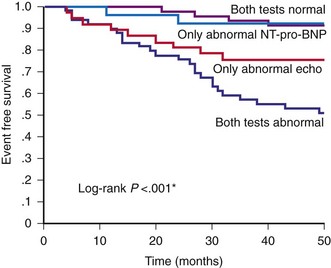
In a general community outpatient clinic, 175 patients with suspected heart failure were examined using an HCU device (OptiGo, Philips, Andover, Mass.) by an internist who had received 4 weeks of training in HCU. The examination included assessment of LV size and systolic function, left atrial size, and valve dysfunction. In the 90 patients (55%) with an abnormal baseline HCU study, 25% were hospitalized for cardiac indication over the next 48 months. On multivariate analysis, an abnormal HCU examination was a strong predictor of clinical outcome with a hazard ratio of 5.55 (95% confidence interval 2.04-14.28, P = .0004) and was more predictive than serum BNP levels (Fig. 8-5).33
Cardiology
A limited examination on a relatively inexpensive HCU system can be time efficient and cost effective. In a cardiology clinic, a hand-carried ultrasound system (OptiGo, Philips) was compared to a standard echocardiographic system with a mean examination time of 6.7 ± 1.5 minutes using an HCU versus 13.6 ± 2.4 minutes using the standard echocardiographic system.6 The HCU was considered satisfactory in 85% of patients, and the data were concordant with the standard echocardiographic system in 83.8% of patients. Certainly, a cardiologist could incorporate an HCU examination as part of the bedside evaluation with great utility and impact on clinical management (Fig. 8-6).
Because of its time saving and ability to eliminate unnecessary examinations, screening and triaging with HCU or palm-sized systems is cost effective to eliminate unnecessary full examinations. One analysis estimated a 29% reduction in departmental workload, at a significant cost savings if all patients with a complete echocardiogram requested for LV function assessment underwent HCU initially and only those with abnormal scans underwent complete standard echocardiography.39 HCU’s high accuracy for detection of normal cardiac anatomy and function also is an efficient tool in eliminating unnecessary examinations.
Future Directions
Point-of-care ultrasonography has become state-of-the-art care provided by several different medical specialties as well as primary care providers. In their New England Journal of Medicine article, Moore and Copel40 note that ultrasonography is a user-dependent technology, and as usage spreads, there is a need to ensure competence, define the benefits of appropriate use, and limit unnecessary imaging and its consequences. They focus on procedural guidance, diagnostic assessment, the e-FAST examination (focused assessment with sonography for trauma, extended to include an examination of the chest for pneumothorax), and screening, especially for abdominal aortic aneurysms. There is minimal mention of cardiac imaging. Although they state that point-of-care ultrasound may be particularly cost effective by eliminating more expensive imaging tests, appropriate training and quality assurance as well as outcome and clinical effectiveness studies are needed.41 True point-of-care ultrasound and echocardiographic examinations will be performed in the emergency department as well as by hospitalists and medical house staff. The same caution for adequate training and interpretation should be applied to the propagation of point-of-care cardiac echocardiographic imaging by noncardiologists.
William Zoghbi, in his capacity as president of the American Society of Echocardiography, editorialized that point-of-care echocardiography fulfills the mandate of the Patient Protection and Affordable Care Act of 2010 that rewards value, quality, and outcomes over quantity. HCU is poised to deliver cost-effective quality care.39,42 With the graying and aging of Americans, there will be an increased incidence of valvular heart disease and murmurs on physical examination.43 Inexpensive HCU cardiac examinations may provide effective triage for those patients requiring full echocardiographic examinations, thereby expediting care, ensuring appropriate use of expensive technologies, and reducing health care costs. Integration of hand-carried or palm-sized ultrasound devices into the medical school physical examination curriculum could empower future clinicians with the basic skills for image acquisition and interpretation and improve medical care, expediting critical decisions at significant savings to the health care system.
Key Points
 Hand-carried ultrasound (HCU) refers to small, lightweight systems with basic 2D imaging capability.
Hand-carried ultrasound (HCU) refers to small, lightweight systems with basic 2D imaging capability.
 Palm-sized devices are best suited as an adjunct to supplement the bedside physical examination.
Palm-sized devices are best suited as an adjunct to supplement the bedside physical examination.
 HCU is ideal for inexpensive screening of large populations with low prevalence of disease.
HCU is ideal for inexpensive screening of large populations with low prevalence of disease.
 Training guidelines for image acquisition and interpretation vary by specialty and need.
Training guidelines for image acquisition and interpretation vary by specialty and need.
 Small but technologically complete laptop-sized systems are also available but require the same level of training and expertise as larger complete echocardiography systems.
Small but technologically complete laptop-sized systems are also available but require the same level of training and expertise as larger complete echocardiography systems.
1 Cheng TO. How Laennec invented the stethoscope. Int J Cardiol. 2007;118:281-285.
2 Roelandt J, Wladimiroff JW, Baars AM. Ultrasonic real time imaging with a hand-held-scanner. Part II—initial clinical experience. Ultrasound Med Biol. 1978;4:93-97.
3 Seward JB, Douglas PS, Erbel R, et al. Hand-carried cardiac ultrasound (HCU) device: recommendations regarding new technology. A report from the Echocardiography Task Force on New Technology of the Nomenclature and Standards Committee of the American Society of Echocardiography. J Am Soc Echocardiogr. 2002;15:369-373.
4 Mondillo S, Giannotti G, Innelli P, et al. Handheld echocardiography: its use and usefulness. Int J Cardiol. 2006;111:1-5.
5 Mondillo S, Galderisi M. [Handheld echocardiography in clinical practice]. Ital Heart J Suppl. 2005;6:265-271.
6 Giannotti G, Mondillo S, Galderisi M, et al. Handheld echocardiography: added value in clinical cardiological assessment. Cardiovasc Ultrasound. 2005;3:7.
7 Vourvouri EC, Poldermans D, de Sutter J, et al. Experience with an ultrasound stethoscope. J Am Soc Echocardiogr. 2002;15:80-85.
8 Vourvouri EC, Schinkel AFL, Roelandt JRTC, et al. Screening for left ventricular dysfunction using a hand-carried cardiac ultrasound device. Eur J Heart Fail. 2003;5:767-774.
9 Vourvouri EC, Poldermans D, Deckers JW, et al. Evaluation of a hand carried cardiac ultrasound device in an outpatient cardiology clinic. Heart. 2005;91:171-176.
10 Kimura BJ, Amundson SA, Willis CL, et al. Usefulness of a handheld ultrasound device for bedside examination of left ventricular function. Am J Cardiol. 2002;90:1038-1039.
11 Dalla Pozza R, Loeff M, Kozlik-Feldmann R, Netz H. Hand-carried ultrasound devices in pediatric cardiology: clinical experience with three different devices in 110 patients. J Am Soc Echocardiogr. 2010;23:1231-1237.
12 Prinz C, Voigt JU. Diagnostic accuracy of a handheld ultrasound scanner in routine patients referred for echocardiography. J Am Soc Echocardiogr. 2011;24:111-116.
13 Bloch A, Crittin J, Jaussi A. Should functional cardiac murmurs be diagnosed by auscultation or by Doppler echocardiography? Clin Cardiol. 2001;24:767-769.
14 Shry EA, Smithers MA, Mascette AM. Auscultation versus echocardiography in a healthy population with precordial murmur. Am J Cardiol. 2001;87:1428-1430.
15 Salustri A, Trambaiolo P. Point-of-care echocardiography: small, smart and quick. Eur Heart J. 2002;23:1484-1487.
16 Galderisi M, Santoro A, Versiero M, et al. Improved cardiovascular diagnostic accuracy by pocket size imaging device in non-cardiologic outpatients: the NaUSiCa (Naples Ultrasound Stethoscope in Cardiology) study. Cardiovasc Ultrasound. 2010;8:51.
17 Salustri A, Trambaiolo P. The “ultrasonic stethoscope”: is it of clinical value? Heart. 2003;89:704-706.
18 Sicari R, Galderisi M, Voigt JU, et al. The use of pocket-size imaging devices: a position statement of the European Association of Echocardiography. Eur J Echocardiogr. 2011;12:85-87.
19 Douglas PS, Khanderia B, Stainback RF, et al. ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 appropriateness criteria for transthoracic and transesophageal echocardiography: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American Society of Echocardiography, American College of Emergency Physicians, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society for Cardiovascular Magnetic Resonance. Endorsed by the American College of Chest Physicians and the Society of Critical Care Medicine. J Am Soc Echocardiogr. 2007;20:787-805.
20 Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr. 2010;23:1225-1230.
21 Vignon P, Mücke F, Bellec F, et al. Basic critical care echocardiography: validation of a curriculum dedicated to noncardiologist residents. Crit Care Med. 2011;39(4):636-642.
22 Melamed R, Sprenkle MD, Ulstad VK, et al. Assessment of left ventricular function by intensivists using handheld echocardiography. Chest. 2009;135:1416-1420.
23 Breitkreutz R, Uddin S, Steiger H, et al. Focused echocardiography entry level: new concept of a 1-day training course. Minerva Anestesiol. 2009;75:285-292.
24 Khasawneh FA, Smalligan RD. Focused transthoracic echocardiography. Postgrad Med. 2010;122:230-237.
25 Kobal SL, Atar S, Siegel RJ. Hand-carried ultrasound improves the bedside cardiovascular examination. Chest. 2004;126:693-701.
26 Kobal SL, Trento L, Baharami S, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96:1002-1006.
27 Decara JM, Kirkpatrick JN, Spencer JT, et al. Use of hand-carried ultrasound devices to augment the accuracy of medical student bedside cardiac diagnoses. J Am Soc Echocardiogr. 2005;18:257-263.
28 Alexander JH, Peterson ED, Chen AY, et al. Feasibility of point-of-care echocardiography by internal medicine house staff. Am Heart J. 2004;147:476-481.
29 Emergency ultrasound guidelines. Ann Emerg Med. 2009;53:550-570.
30 Wright J, Jarman R, Connolly J, Dissmann P. Echocardiography in the emergency department. Emerg Med J. 2009;26:82-86.
31 Manasia AR, Nagaraj HM, Kodali RB, et al. Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. J Cardiothorac Vasc Anesth. 2005;19:155-159.
32 Schmidt GA. ICU ultrasound. The coming boom. Chest. 2009;135:1407-1408.
33 Lipczyńska M, Szymański P, Klisiewicz A, Hoffman P. Hand-carried echocardiography in heart failure and heart failure risk population: a community based prospective study. J Am Soc Echocardiogr. 2011;24:125-131.
34 Goonewardena SN, Gemignani A, Ronan A, et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1:595-601.
35 Martin LD, Howell EE, Ziegelstein RC, et al. Hand-carried ultrasound performed by hospitalists: does it improve the cardiac physical examination? Am J Med. 2009;122:35-41.
36 Trambaiolo P, Papetti F, Posteraro A, et al. A hand-carried cardiac ultrasound device in the outpatient cardiology clinic reduces the need for standard echocardiography. Heart. 2007;93:470-475.
37 Cardim N, Fernandez Golfin C, Ferreira D, et al. Usefulness of a new miniaturized echocardiographic system in outpatient cardiology consultations as an extension of physical examination. J Am Soc Echocardiogr. 2011 Feb;24(2):117-124.
38 Ferrada P, Murthi S, Anand RJ, et al. Transthoracic focused rapid echocardiographic examination: real-time evaluation of fluid status in critically ill trauma patients. J Trauma. 2011;70:56-62. discussion 62-54
39 Greaves K, Jeetley P, Hickman M, et al. The use of hand-carried ultrasound in the hospital setting—a cost-effective analysis. J Am Soc Echocardiogr. 2005;18:620-625.
40 Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364:749-757.
41 Kimura BJ, Amundson SA, Shaw DJ. Hospitalist use of hand-carried ultrasound: preparing for battle. J Hosp Med. 2010;5:163-167.
42 Zoghbi WA. Echocardiography at the point of care: an ultra sound future. J Am Soc Echocardiogr. 2011;24:132-134.
43 Croft LB, Donnino R, Shapiro R, et al. Age-related prevalence of cardiac valvular abnormalities warranting infectious endocarditis prophylaxis. Am J Cardiol. 2004;94:386-389.