1 Hand and Wrist Injuries
Flexor Tendon Injuries
Important points for rehabilitation after flexor tendon laceration and repair
Rehabilitation rationale and basic principles of treatment after flexor tendon repair
Timing
Before tendons can be secondarily repaired, these requirements must be met:
| Grade | Preoperative Condition |
|---|---|
| 1 | Good: minimal scar with mobile joints and no trophic changes |
| 2 | Cicatrix: heavy skin scarring from injury or previous surgery; deep scarring from failed primary repair or infection |
| 3 | Joint damage: injury to the joint with restricted range of motion |
| 4 | Nerve damage: injury to the digital nerves resulting in trophic changes in the finger |
| 5 | Multiple damage: involvement of multiple fingers with a combination of the above problems |
Anatomy
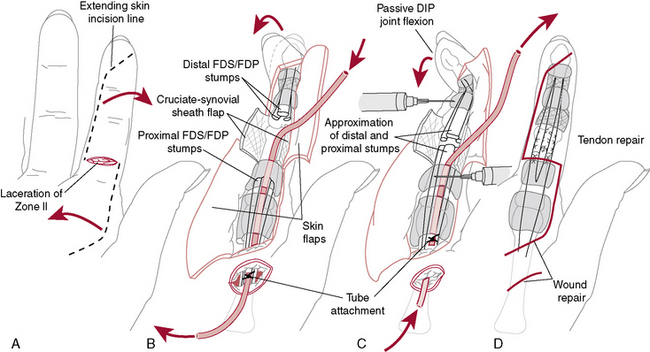
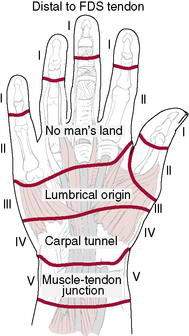
The anatomic zone of injury of the flexor tendons influences the outcome and rehabilitation of these injuries. The hand is divided into five distinct flexor zones (Fig. 1-3):
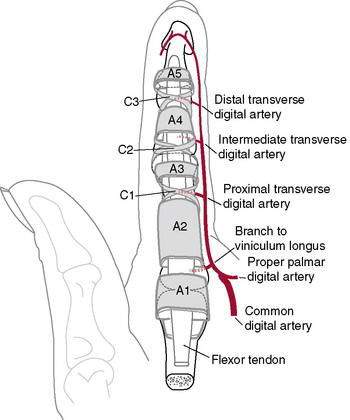
It is essential that the A2 and A4 pulleys (Fig. 1-4) be preserved to prevent bowstringing. In the thumb, the A1 and oblique pulleys are the most important. The thumb lacks vincula for blood supply.
Tendon Healing
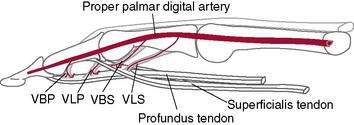
Flexor tendons in the distal sheath have a dual source of nutrition via the vincular system and synovial diffusion. Diffusion appears to be more important than perfusion in the digital sheath (Green 1993).
Several factors have been reported to affect tendon healing:
Through experimental and clinical observation, Duran and Houser (1975) determined that tendon glide of 3 to 5 mm is sufficient to prevent motion-limiting tendon adhesions. Exercises are thus designed to achieve this motion.
Treatment of Flexor Tendon Lacerations
Teno-Fix Repair
A stainless-steel tendon repair device (Teno Fix, Ortheon Medical, Columbus, OH) was reported to result in lower flexor tendon rupture rates after repair and similar functional outcomes when compared with conventional repair in a randomized, multicenter study, particularly in patients who were noncompliant with the rehabilitation protocol (Su et al. 2005, 2006). Active flexion was allowed at 4 weeks postoperatively. Solomon et al. (unpublished research) developed an “accelerated active” rehabilitation program to be used after Teno Fix repairs: Active digital flexion and extension maximum-attainable to the palm are started on the first day with the goal of full flexion at 2 weeks postoperatively. The anticipated risks with this protocol are forced passive extension, especially of the wrist and finger (e.g., fall on outstretched hand), and resisted flexion, potentially causing gapping or rupture of the repair.
FDP lacerations can be repaired directly or advanced and reinserted into the distal phalanx with a pull-out wire, but they should not be advanced more than 1 cm to avoid the quadregia effect (a complication of a single digit with limited motion causing limitation of excursion and, thus, the motion of the uninvolved digits). Citing complications in 15 of 23 patients with pull-out wire (button-over-nail) repairs, 10 of which were directly related to the technique, Kang et al. (2008) questioned its continued use. Complications of the pull-out wire technique included nail deformities, fixed flexion deformities of the distal interphalangeal (DIP) joint, infection, and prolonged hypersensitivity.
A more recent technique for FDP lacerations is the use of braided polyester/monofilament polyethylene composite (FiberWire, Arthrex, Naples, FL) and suture anchors rather than pull-out wires (Matsuzaki et al. 2008, McCallister et al. 2006). Reports of outcomes currently are too few to determine if this technique will allow earlier active motion than standard techniques.
Rehabilitation after flexor tendon repair
The rehabilitation protocol chosen (Rehabilitation Protocols 1-1 and 1-2) depends on the timing of the repair (delayed primary or secondary), the location of the injury (zones 1 through 5), and the compliance of the patient (early mobilization for patients who are compliant and delayed mobilization for patients who are noncompliant and children younger than 7 years of age). A survey of 80 patients with flexor and extensor tendon repairs determined that two thirds were nonadherent to their splinting regimen, removing their splints for bathing and dressing (Sandford et al. 2008).
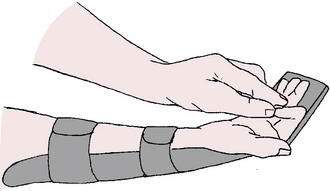
REHABILITATION PROTOCOL 1-1 Rehabilitation Protocol after Immediate or Delayed Primary Repair of Flexor Tendon Injury: Modified Duran Protocol
Postoperative Day 1 to Week 4.5
4.5 Weeks
REHABILITATION PROTOCOL 1-2 Indianapolis Protocol (“Active Hold Program”)
(From Neumeister M, Wilhelmi BJ, Bueno Jr, RA: Flexor tendon lacerations: Treatment. http://emedicine.medscape.com/orthopedic_surgery)
In a comparison of early active mobilization and standard Kleinert splintage,Yen et al. (2008)found at an average 4-month follow-up (3 to 7 months) that those in the early active mobilization group had 90% of normal grip strength, pinch, and range of motion compared to 50%, 40%, and 40%, respectively, in those with Kleinert splinting.
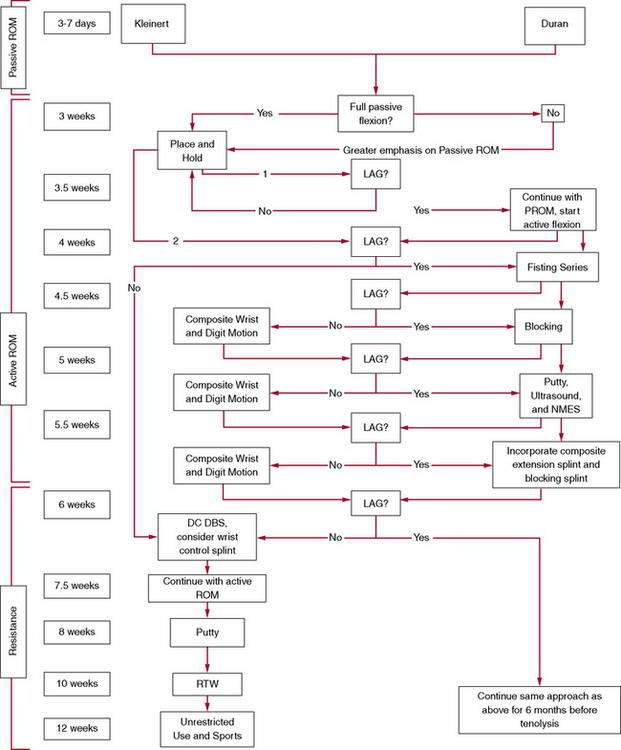
Sueoka and LaStayo (2008) devised an algorithm for zone 2 flexor tendon rehabilitation that uses a single clinical sign—the lag sign—to determine the progression of therapy and the need to modify existing protocols for individual patients. They defined “lag” as PROM—AROM (active ROM) ≥15 degrees and consider it a sign of tendon adherence and impairment of gliding. Rehabilitation begins with an established passive ROM Protocol (Duran), which is followed for 3.5 weeks before the presence or absence of a lag is evaluated. The presence or absence of lag is then evaluated at the patient’s weekly or twice-weekly visits, and progression of therapy is modified if a lag sign is present (Rehabilitation Protocol 1-3).
Trigger Finger (Stenosing Flexor Tenosynovitis)
S. Brent Brotzman, MD, and Theresa M. Kidd, BA
Treatment
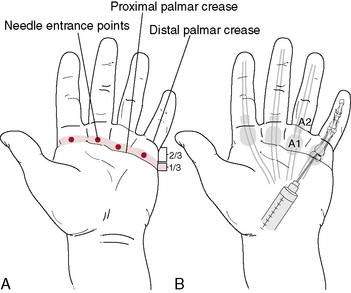
Currently, nonoperative treatment involves injection of corticosteroids with local anesthetic into the flexor sheath. A meta-analysis of the literature found convincing evidence that combining lidocaine with the corticosteroid obtains results superior to those with corticosteroid alone(Chambers 2009). In a cost-minimization analysis, the use of two steroid injections before resorting to surgery was found to be the least costly treatment strategy compared to one or three injections before surgery and open or percutaneous release(Kerrigan and Stanwix 2009).
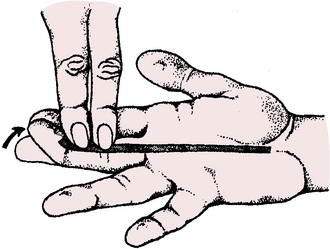
Our preference is 0.5 ml lidocaine, 0.5 ml bupivicaine, and 0.5 ml methylprednisolone acetate (Depo-Medrol) (Fig. 1-5). A single injection can be expected to relieve triggering in about 66% of patients. Multiple injections have been reported to relieve triggering in 75% to 85% of patients. Current reports indicate a success rate of 47% to 87% with this type of treatment. Systematic review of levels I and II studies in the Journal of the American Academy of Orthopedic Surgeons (Fleisch et al. 2007) indicates a success rate of 57%. Prognostic indicators of recurrence of trigger digits after corticosteroid injection include younger age, insulin-dependent diabetes mellitus, involvement of multiple digits, and a history of other tendinopathies of the upper extremity (Rozental et al. 2008).
The risk of cortisone injection here is of inadvertent injection into the flexor tendon with possible tendon weakening or rupture. Ultrasound guidance has been reported to help avoid this complication and improve results (Bodor and Flossman 2009).
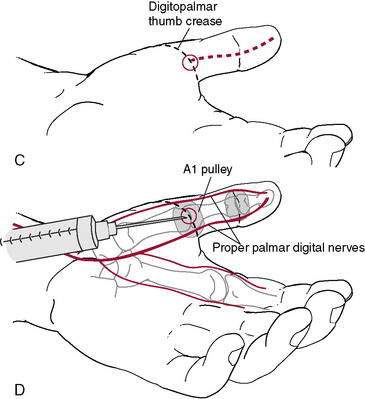
Surgery to “release” a trigger finger is a relatively simple outpatient procedure done with the patient under local anesthesia. The surgery involves a 1- to 2-cm incision in the palm overlying the A1 pulley to identify and completely divide the A1 pulley. Gentle active motion is initiated early, and return to unrestricted activities usually is possible at about 3 weeks (Rehabilitation Protocol 1-4).
REHABILITATION PROTOCOL 1-4 Rehabilitation Protocol After Trigger Finger Cortisone Injection or Release
After Trigger Release Surgery
| 0–4 days | Gentle active MCP/PIP/DIP joint ROM (avoid gapping of wound). |
| 4 days | Remove bulky dressing and cover wound with bandage. |
| 4–8 days | Continue ROM exercises. Remove sutures at 7–9 days. |
| 8 days–3 weeks | Active/active-assisted ROM/PROM MCP/PIP/DIP joints. |
| 3 weeks + | Aggressive ROM and strengthening. Return to unrestricted activities. |
Pediatric trigger thumb
Pediatric trigger thumb is a congenital condition in which stenosis of the A1 pulley of the thumb in infants causes locking in flexion (inability to extend) of the IP joint. It often is bilateral. Usually no pain or clicking occurs because the thumb remains locked. A recent report by Baek et al. (2008) indicates spontaneous resolution in 63% of cases. The rest require surgical intervention when the patient is around 2 to 3 years old to release the tight A1 pulley and prevent permanent joint flexion contracture.
Flexor Digitorum Profundus Avulsion (“Jersey Finger”)
Background
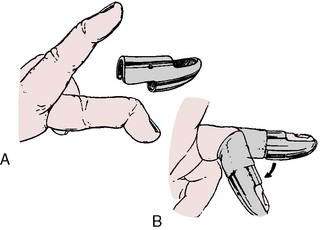
The resultant lack of active flexion of the DIP joint (FDP function loss) must be specifically checked to make the diagnosis (Fig. 1-6). Often the swollen finger assumes a position of extension relative to the other, more flexed fingers. The level of retraction of the FDP tendon back into the palm generally denotes the force of the avulsion.
Leddy and Packer (1977) described three types of FDP avulsions based on where the avulsed tendon retracts: type I, retraction of the FDP to the palm; type II, retraction to the proximal interphalangeal (PIP) joint; and type III, bony fragment distal to the A4 pulley. Subsequently, a type IV injury was described in which a type III lesion is associated with a simultaneous avulsion of the FDP from the fracture fragment. Treatment is based on the anatomy of the injury.
Treatment
The treatment of FDP avulsion is primarily surgical. The success of the treatment depends on the acuteness of diagnosis, rapidity of surgical intervention, and level of tendon retraction. Tendons with minimal retraction usually have significant attached avulsion bone fragments, which may be reattached bone-to-bone as late as 6 weeks. Tendons with a large amount of retraction often have no bone fragment and have disruption of the vascular supply (vinculum), making surgical repair more than 10 days after injury difficult because of retraction and the longer healing time of the weaker nonbone-to-bone fixation and limited blood supply to the repair. Based on a review of the literature and their clinical experience, Henry et al. (2009) listed four essentials for successful treatment of type IV extensor tendon injuries: (1) a high index of suspicion for this injury, with the use of magnetic resonance imaging (MRI) or ultrasound for confirmation if needed, (2) rigid bony fixation that prevents dorsal subluxation of the distal phalanx, (3) tendon repair that is independent of the bony fixation, and (4) early range of motion therapy (Rehabilitation Protocol 1-5).
REHABILITATION PROTOCOL 1-5 Rehabilitation Protocol After Surgical Repair of Jersey Finger with Secure Bony Repair
0–10 Days
Extensor Tendon Injuries
S. Brent Brotzman, MD, and Theresa M. Kidd, BA
Anatomy
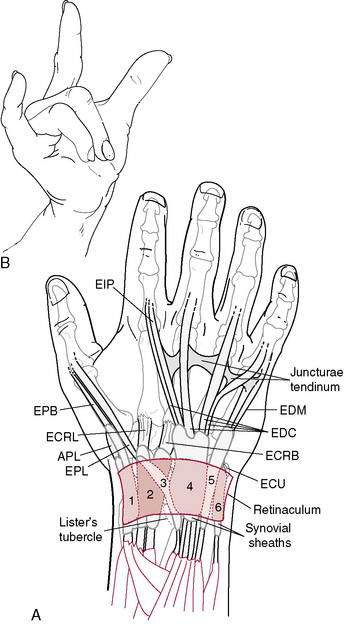
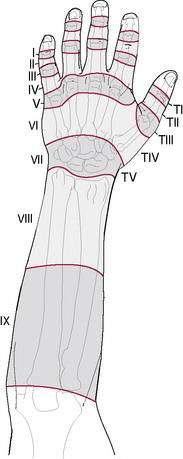
Extensor mechanism injuries are grouped into eight anatomic zones, according to Kleinert and Verdan (1983). Odd-number zones overlie the joint levels so that zones 1, 3, 5, and 7 correspond to the DIP, PIP, metacarpal phalangeal (MCP), and wrist joint regions, respectively (Figs. 1-7 and 1-8; Table 1-2).
| Zone | Finger | Thumb |
|---|---|---|
| I | Distal interphalangeal joint | Interphalangeal joint |
| II | Middle phalanx | Proximal phalanx |
| III | Proximal interphalangeal joint | Metacarpophalangeal joint |
| IV | Proximal phalanx | Metacarpal |
| V | MP joint | Carpometacarpal joint/radial styloid |
| VI | Metacarpal | |
| VII | Dorsal retinaculum | |
| VIII | Distal forearm | |
| IX | Mid and proximal forearm |
Table 1-2 Zones of Extensor Mechanism Injury
| Zone | Finger | Thumb |
|---|---|---|
| 1 | DIP joint | IP joint |
| 2 | Middle phalanx | Proximal phalanx |
| 3 | Apex PIP joint | MCP joint |
| 4 | Proximal phalanx | Metacarpal |
| 5 | Apex MCP joint | — |
| 6 | Dorsal hand | — |
| 7 | Dorsal retinaculum | Dorsal retinaculum |
| 8 | Distal forearm | Distal forearm |
DIP, distal interphalangeal; IP, interphalangeal; PIP, proximal interphalangeal; MCP, metacarpophalangeal.
From Kleinert HE, Verdan C. Report of the committee on tendon injuries. J Hand Surg 1983;8:794.
Extensor tendon injuries in zones 1 and 2
A recent literature review (Soni et al. 2009) found that traditional postoperative static splinting was equivalent to early motion protocols for all uncomplicated thumb injuries and zone 1 to 3 injuries of the second through fifth digits. The only benefit of early motion therapy compared with static splinting was a quicker return to final function for proximal zones of injury in the second through fifth digits. At 6 months after surgery, results of static splinting were comparable to those with early active and passive motion. Static splinting also was associated with a lower rupture rate than early active motion and a lower cost than early active and passive motion. An earlier meta-analysis (Talsma et al. 2008) found that short-term outcomes (4 weeks postoperative) after immobilization were significantly inferior to outcomes after early controlled mobilization, but at 3 months postoperatively no significant differences were found (Rehabilitation Protocol 1-6).
REHABILITATION PROTOCOL 1-6 Treatment and Rehabilitation of Chronic Extensor Tendon Injuries in Zones 1 and 2
| Tenodermodesis | Central Slip Tenotomy (Fowler) | Oblique Retinacular Ligament Reconstruction |
|---|---|---|
| Tenodermodesis is a simple procedure used in relatively young patients who are unable to accept the mallet finger disability. With the use of a local anesthetic, the DIP joint is fully extended and the redundant pseudotendon is excised so that the edges of the tendon coapt. A Kirschner wire may be used temporarily to fix the DIP joint in full extension. | With the use of a local anesthetic, the insertion of the central slip is sectioned where it blends with the PIP joint dorsal capsule. The combined lateral band and the extrinsic contribution should be left undisturbed. Proximal migration of the dorsal apparatus improves the extensor force at the DIP joint. A 10- to 15-degree extensor lag at the PIP joint may occur. | Reconstruction of the oblique retinacular ligament is done for correction of a chronic mallet finger deformity and secondary swan-neck deformity. A free tendon graft, such as the palmaris longus tendon, is passed from the dorsal base of the distal phalanx and volar to the axis of the PIP joint. The graft is anchored to the contralateral side of the proximal phalanx at the fibro-osseous rim. Kirschner wires temporarily fix the DIP joint in full extension and the PIP joint in 10 to 15 degrees of flexion. |
| 3–5 Days | 0–2 Weeks | 3 Weeks |
2–4 Weeks
4–5 Weeks
Extensor tendon injuries in zones 4, 5, and 6
Normal function is usually possible after unilateral injuries to the dorsal apparatus, and splinting and immobilization are not recommended. Complete disruptions of the dorsal expansion and central slip lacerations are repaired (Rehabilitation Protocol 1-7).
REHABILITATION PROTOCOL 1-7 After Surgical Repair of Extensor Tendon Injuries in Zones 4, 5, and 6
Zone 5 Extensor Tendon Subluxations
Acute injuries can be repaired directly, and chronic injuries can be reconstructed with local tissue. Most reconstructive procedures use portions of the juncturae tendinum or extensor tendon slips anchored to the deep transverse metacarpal ligament or looped around the lumbrical tendon(Rehabilitation Protocol 1-8).
REHABILITATION PROTOCOL 1-8 After Surgical Repair of Zone 5 Extensor Tendon Subluxation
2 Weeks
Extensor tendon injuries in zones 7 and 8
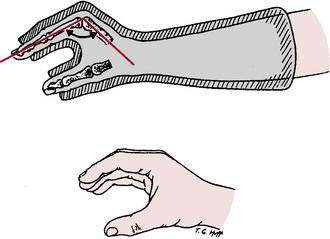
Repairs done 3 weeks or more after the injury may weaken the extensor pollicis longus (EPL) muscle sufficiently for electrical stimulation to become necessary for tendon glide. The EPL is selectively strengthened by thumb retropulsion exercises done against resistance with the palm held on a flat surface (Rehabilitation Protocol 1-9).
REHABILITATION PROTOCOL 1-9 After Surgical Repair of Extensor Tendon Injuries in Zones 7 and 8
2–4 Weeks
4–6 Weeks
Extensor tenolysis
Indications
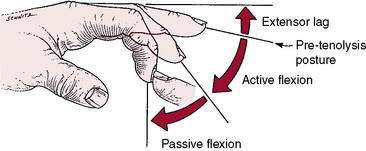
Figure 1-9 Passive supple digit with an extensor lag is an indication for possible extensor tenolysis.
(From Strickland JW: The Hand: Master Techniques in Orthopaedic Surgery. Philadelphia, Lippincott-Raven, 1998.)
Frequently, MCP and PIP joint capsular and ligament releases are necessary to obtain the desired joint motion. Complete collateral ligament resection may be required, and special attention may be necessary in the early postoperative period for resultant instability. Extensive tenolyses may require analgesic dosing before and during therapy sessions. Indwelling catheters also may be needed for instillation of local anesthetics for this purpose (Rehabilitation Protocol 1-10).
REHABILITATION PROTOCOL 1-10 After Extensor Tenolysis
1 Day–4 Weeks
4–6 Weeks
6 Weeks
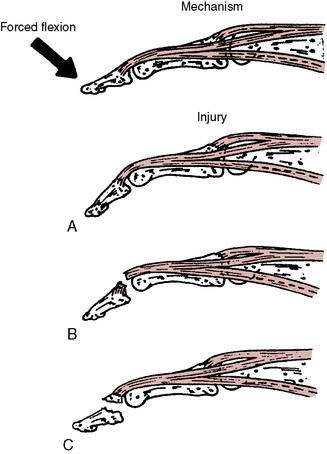
Mallet finger (extensor injury—zone 1)
Background
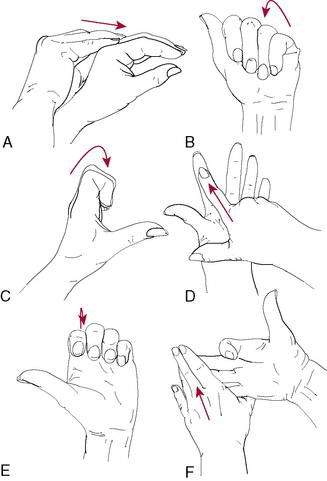
Avulsion of the extensor tendon from its distal insertion at the dorsum of the DIP joint produces an extensor lag at the DIP joint. The avulsion may occur with or without a bony fragment avulsion from the dorsum of the distal phalanx. This is termed a mallet finger of bony origin or mallet finger of tendinous origin (Fig. 1-10). The hallmark finding of a mallet finger is a flexed or dropped posture of the DIP joint and an inability to actively extend or straighten the DIP joint. The mechanism is typically forced flexion of the fingertip, often from the impact of a thrown ball.
Treatment
Abound and Brown (1968) found that several factors are likely to lead to a poor prognosis after mallet finger injury:
The results of mallet finger treatment are not universally good by any method of treatment.
Continuous extension splinting of the DIP joint, leaving the PIP free for 6 to 10 weeks is the typical treatment for mallet fingers of tendinous origin (Fig. 1-11). A variety of splints has been developed for treatment of mallet finger. Most commonly used are the Stack splint, the perforated thermoplastic splint, and the aluminium-foam splint. If no extensor lag exists at 6 weeks, night splinting for 3 weeks and splinting during sports activities for an additional 6 weeks are used.
Although splinting is the treatment of choice for most acute and chronic mallet finger injuries, surgery may be indicated for individuals who are unable to comply with a splinting regimen or for patients who would have difficulty performing their jobs with an external splint. Surgical options for acute mallet fractures include transarticular pinning of the DIP joint, compression pinning, and extension block pinning. For chronic injuries (more than 4 weeks after injury) surgical options include terminal extensor tendon shortening, tenodermodesis, reconstruction of the oblique retinacular ligament, and central slip tenotomy (see Rehabilitation Protocol 1-6 on page 43). Arthrodesis may be required as a salvage procedure for mallet fingers caused by arthritis, infection, or failed surgery.
Fractures and Dislocations of the Hand
Maureen A. Hardy, PT, MS, CHT, and S. Brent Brotzman, MD
Fractures that often require surgical intervention include the following:
Metacarpal and phalangeal fractures
General Principles
Metacarpal fractures
Table 1-3 Potential Problems with Metacarpal Fractures and Strategies for Therapeutic Intervention Maureen A. Hardy PT, MS CHT
| Potential Problems | Prevention and Treatment |
|---|---|
| Dorsal hand edema | Coban wrap compression, ice, elevation, high-voltage stimulation |
| Dorsal skin scar contracture that prevents full fist | Silicone, TopiGel, simultaneous heat and stretch with hand wrapped in a fisted position; friction massage |
| MP joint contracted in extension | Initially: position MP joint at 70 degrees of flexion in protective splint Late: dynamic or static progressive MP joint splint |
| Adherence of EDC tendon to fracture with limited MP joint flexion | Initially: teach EDC glide exercise to prevent adherence; splint IP joint in extension during exercises to concentrate flexion power at MP joint Late: dynamic MP flexion splint; NMES of EDC with on > off cycle |
| Intrinsic muscle contracture secondary to swelling and immobilization | Initially: teach intrinsic stretch (intrinsic minus position) Late: static progressive splint in intrinsic minus position |
| Dorsal sensory radial/ulnar nerve irritation | Desensitization program; iontophoresis with lidocaine |
| Attrition and potential rupture of extensor tendon over prominent dorsal boss or large plate | Rest involved tendon; contact physician if painful symptoms with AROM persist |
| Scissoring/overlapping of digits with flexion | Slight: buddy tape to adjacent digit Severe: malrotation deformity requiring ORIF |
| Absence of MP head | Shortening of metacarpal; may not be functional problem |
| Absence of MP head and MP joint extension lag | Shortening of metacarpal with redundancy in extensor length; splint in extension at night; strengthen intrinsics abduction/adduction; NMES of intrinsics with off > on cycle |
| Absence of MP head with volar prominence and pain with grip | Neck fracture angulated volarly Minor: padded work glove Major: reduction of angulation required |
MP, metacarpophalangeal; EDC, extensor digitorum communis; IP, interphalangeal; NMES, neuromuscular electrical stimulation; AROM, active range of motion.
Nondisplaced metacarpal fractures are stable injuries and are treated with application of an anteroposterior splint in the position of function: the wrist in 30 to 60 degrees of extension, the MCP joints in 70 degrees of flexion, and the IP joints in 0 to 10 degrees of flexion. In this position the important ligaments of the wrist and hand are maintained in maximal tension to prevent contractures (Fig. 1-13). Exceptions to splinting for metacarpal fractures may include treatment of boxer’s fractures (see page 13).
Fifth Metacarpal Neck Fracture (Boxer’s Fracture)
S. Brent Brotzman, MD; Theresa M. Kidd, BA; and Maureen A. Hardy PT, MS, CHT
Clinical history and examination
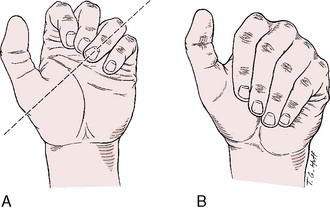
Patients usually have pain, swelling, and loss of motion about the MCP joint. Occasionally a rotational deformity is present. Careful examination should be performed to ensure that there is no malrotation of the fifth finger when the patient makes a fist (Fig. 1-14), no significant prominence of the distal fragment (palmarly displaced) in the palm, and no extensor lag of the involved finger.
Treatment
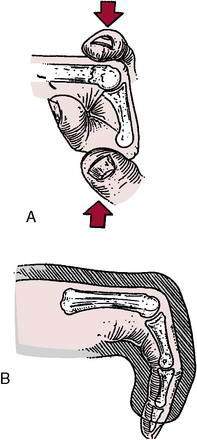
If displacement is unacceptable, closed reduction can be attempted with wrist block anesthesia using the maneuver credited to Jahss (1938), in which the proximal phalanx is flexed to 90 degrees and used to apply a dorsally directed force to the metacarpal head (Fig. 1-15). The hand is then splinted in an ulnar gutter splint for about 3 weeks with the MCP joint at 80 degrees of flexion, the PIP joint straight, and the DIP joint free.
Statius Muller et al. (2003) prospectively treated 35 patients with boxer’s fractures with a mean fracture angulation of 39 degrees (range 15 to 70 degrees). Patients were randomly allocated to treatment with either an ulnar gutter plaster cast for a period of 3 weeks followed by mobilization or a pressure bandage for only 1 week and immediate mobilization within limits imposed by pain. Between the two groups, no statistical differences were found with respect to ROM, satisfaction, pain perception, return to work and hobby, or need for physical therapy. In our clinic we employ the pressure bandage technique for our boxer’s fractures with good result.
Bansal and Craigen (2007) treated 40 boxer’s fractures with reduction and casting and 40 with buddy taping and range of motion only with instructions to return only if problems were experienced. The Disabilities of the Arm, Shoulder, and Hand (DASH) scores for the two groups were identical at 12 weeks, and the untreated group returned to work 2 weeks earlier and had a significantly higher satisfaction rate on their “care.”
Operative treatment of boxer’s fractures is indicated if the following occur:
Phalangeal Fractures of the Hand
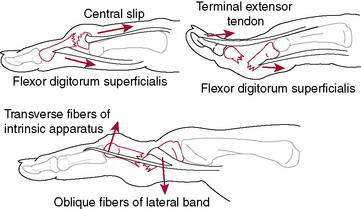
Figure 1-16 Deforming forces on phalangeal fractures.
(Adapted with permission from Breen TF: Sports-related injuries of the hand, in Pappas AM, Walzer J [eds]: Upper Extremity Injuries in the Athlete. New York, Churchill Livingston, 1995, p 475.)
Table 1-4 Potential Problems with Phalangeal Fractures and Strategies for Therapeutic Intervention Maureen A. Hardy PT, MS CHT
| Potential Problems | Prevention and Treatment |
|---|---|
| Loss of MP flexion | Circumferential PIP and DIP extension splint to concentrate flexor power at MP joint; NMES to interossei |
| Loss of PIP extension | Central slip blocking exercises; during the day MP extension block splint to concentrate extensor power at PIP joint; at night PIP extension gutter splint; NMES to EDC and interossei with dual-channel setup |
| Loss of PIP flexion | Isolated FDP tendon glide exercises; during the day MP flexion blocking splint to concentrate flexor power at PIP joint; at night flexion glove; NMES to FDS |
| Loss of DIP extension | Resume night extension splinting; NMES to interossei |
| Loss of DIP flexion | Isolated FDP tendon glide exercises; PIP flexion blocking splint to concentrate flexor power at DIP joint; stretch ORL tightness; NMES to FDP |
| Lateral instability, any joint | Buddy strap or finger-hinged splint that prevents lateral stress |
| Impending boutonnière deformity | Early DIP active flexion to maintain length of lateral bands |
| Impending swan neck deformity | FDS tendon glide at PIP joint and terminal extensor tendon glide at the DIP joint |
| Pseudo claw deformity | Splint to hold MP joint in flexion with PIP joint full extensor glide |
| Pain | Resume protective splinting until healing is ascertained; address edema, desensitization program |
MP, metacarpophalangeal; PIP, proximal interphalangeal; DIP, distal interphalangeal; NMES, neuromuscular electrical stimulation; EDC, extensor digitorum communis; FDP, flexor digitorum profundus; FDS, flexor digitorum superficialis; ORL, oblique retinacular ligament.
Proximal Interphalangeal Joint Injuries
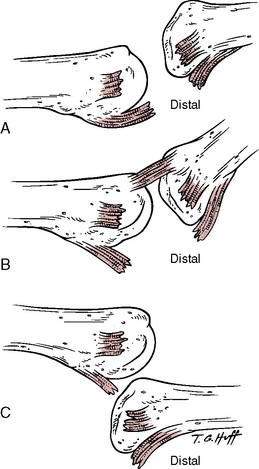
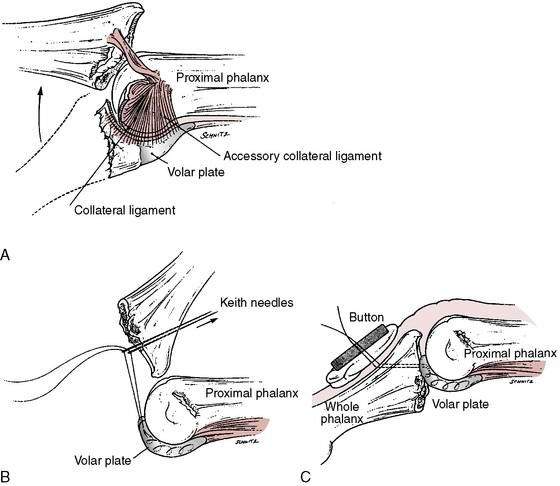
Three types of proximal interphalangeal joint dislocations (Fig. 1-17; Table 1-5) or fracture-dislocations have been described: lateral, volar (rotatory), and dorsal (Fig. 1-18). Each results from a different mechanism of injury and has specific associated complications. The treatment of PIP injuries is dictated by the stability of the injury.
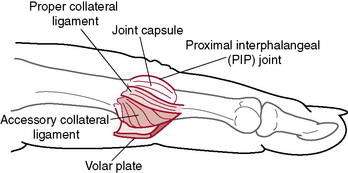
Figure 1-17 Anatomy of the volar plate and collateral ligaments of the proximal interphalangeal (PIP) joint.
(Adapted with permission from Breen TF: Sports-related injuries of the hand, in Pappas AM, Walzer J [eds]: Upper Extremity Injuries in the Athlete. New York, Churchill Livingston, 1995, p 459.)
Table 1-5 Managing Proximal Interphalangeal Joint Injuries of the Hand
| Injury | Clinical Manifestations or Special Considerations | Treatment |
|---|---|---|
| Sprain | Stable joint with active and passive motion; negative radiographs; pain and swelling only | Buddy tape for comfort; begin early ROM exercises, ice, NSAIDs |
| Open dislocation | Dislocated exposed joint | Irrigation, débridement, and antibiotics; treat as any open fracture or dislocation |
| Dorsal PIP Dislocation | ||
| Type 1 | Hyperextension, volar plate avulsion, minor collateral ligament tear | Reduction; very brief immobilization (3–5 days) followed by ROM exercises with buddy taping and close x-ray follow-up |
| Type 2 | Dorsal dislocation, volar plate avulsion, major collateral ligament tear | Same as type 1 |
| Type 3 | Stable fracture-dislocation: <40% of articular arc on fracture fragment | Extension block splint; refer to hand surgeon |
| Unstable fracture-dislocation: >40% of articular arc on fracture fragment | Extension block splint; open reduction with internal fixation if closed treatment impossible; refer to hand surgeon | |
| Lateral dislocation | Secondary to collateral ligament injury and avulsion and/or rupture of volar plate; angulation >20 degrees indicates complete rupture | Same as dorsal dislocation types 1 and 2 if joint is stable and congruous through active ROM |
| Volar PIP Dislocation | ||
| Straight volar dislocation | Proximal condyle causes significant injury to central extensor slip (may reduce easily, but extensor tendon may be seriously injured; requires careful examination) | Refer to a hand surgeon experienced in these rare injuries; closed reduction with traction with metatarsophalangeal and PIP flexed and extended wrist; full-extension immobilization of PIP joint if post-reduction x-rays show no subluxation; if closed reduction is not achieved or subluxation persists, surgery recommended |
| Ulnar or radial volar displacement | Condyle often buttonholes through central slip and lateral band; reduction often extremely difficult | Same as straight volar PIP dislocation |
ROM, range of motion; NSAIDs, nonsteroidal anti-inflammatory drugs; PIP, proximal interphalangeal.
From Laimore JR, Engber WD. Serious, but often subtle finger injuries. Phys Sports Med 1998;l26(6):226.
Stable lesions are treated with buddy taping of the injured digit to the noninjured digit adjacent to the torn or compromised collateral ligament. Unstable injuries are often associated with an intra-articular fracture of the middle phalanx (usually affecting more than 20% of the joint surface). However, even very tiny volar avulsion fractures may be associated with dorsal subluxation of the middle phalanx and be unstable. This is best assessed with fluoroscopy where the point of reduction can be accurately ascertained by sequential flexion of the PIP joint (Morgan and Slowman 2001).
Unstable injuries often are treated by dorsal extension block splinting (Fig. 1-19) with the initial digit flexion at the point where the stable reduction was obtained fluoroscopically. Incremental increase of extension of the splint and digit is done on a weekly basis for 4 weeks or until full extension at the joint has been obtained. Buddy taping is continued for 3 months during sports participation.
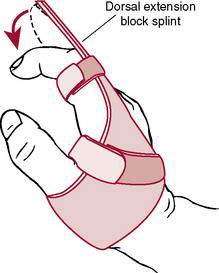
Figure 1-19 Dorsal extension block splint.
(Adapted with permission from Breen TF: Sports-related injuries of the hand, in Pappas AM, Walzer J [eds]: Upper Extremity Injuries in the Athlete. New York, Churchill Livingston, 1995, p 461.)
Volar PIP joint dislocations are less common than dorsal dislocations and are often difficult to reduce by closed techniques because of entrapment of the lateral bands around the flare of the proximal phalangeal head. If not treated properly, these injuries may result in a boutonnière deformity (combined PIP joint flexion and DIP joint extension contracture). Usually, the joint is stable after closed or open reduction; however, static PIP joint extension splinting is recommended for 6 weeks to allow healing of the central slip (Rehabilitation Protocol 1-11).
REHABILITATION PROTOCOL 1-11 Rehabilitation Protocol After Volar Proximal Interphalangeal Joint Dislocation or Avulsion Fracture
After Closed Reduction
Dorsal fracture-dislocations of the PIP joint are much more common than volar dislocations. If less than 50% of the articular surface is involved, these injuries usually are stable after closed reduction and protective splinting (Rehabilitation Protocol 1-12).
REHABILITATION PROTOCOL 1-12 Rehabilitation Protocol After Dorsal Fracture-Dislocation of the Proximal Interphalangeal Joint
Dorsal fracture-dislocations involving more than 40% of the articular surface may be unstable, even with the digit in flexion, and may require surgical intervention. The Eaton volar plate advancement is probably the most common procedure used (Fig. 1-20). The fracture fragments are excised, and the volar plate is advanced into the remaining portion of the middle phalanx. The PIP joint usually is pinned in 30 degrees of flexion (Rehabilitation Protocol 1-13).
REHABILITATION PROTOCOL 1-13 Rehabilitation Protocol After Dorsal Fracture-Dislocation of the Proximal Interphalangeal Joint Involving More Than 40% of the Articular Surface
Injuries to the Ulnar Collateral Ligament of the Thumb Metacarpophalangeal Joint (Gamekeeper’s Thumb)
Background
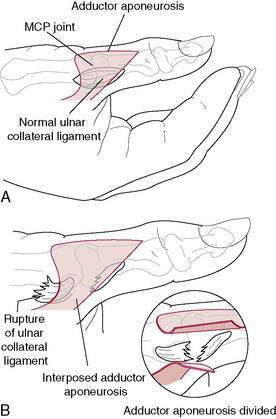
The amount of valgus laxity of normal thumbs varies widely. In full MCP joint extension, valgus laxity averages 6 degrees, and in 15 degrees of MCP joint flexion it increases to an average of 12 degrees. The adductor aponeurosis (when torn and pulled distally) occasionally entraps the UCL, preventing anatomic reduction or healing of the UCL (Stener lesion) (Fig. 1-21). The typical mechanism of injury is an extreme valgus stress to the thumb (e.g., falling on an abducted thumb).
Treatment
Stable Thumb on Valgus Stressing (No Stener Lesion)
REHABILITATION PROTOCOL 1-14 Rehabilitation Protocol After Repair or Reconstruction of the Ulnar Collateral Ligament of the Thumb Metacarpophalangeal Joint