Hand
Perspective
Epidemiology
Overall, hand injuries are reported to represent 5 to 10% of visits to an emergency department (ED), and approximately 6% of the patients have deep, significant injuries.1 Injuries have environmental, occupational, and recreational causes and are seen in all age groups. The spectrum of injury includes infections, lacerations, fractures, crush wounds, amputations, and burns. It is estimated that 10% of all patients with hand injuries require referral to a hand specialist, and most patients referred from EDs have fractures.2 The disability potential of hand injuries generally is high; such disability may involve loss of strength, flexibility, or sensation. According to available data, hand injuries account for 19% of lost-time injuries and for 9% of worker compensation cases.3 Approximately 3 to 4 million working days are lost each year as a result of hand injuries.4 Overall, hand and fingers are the most frequent body parts injured in the workplace and cared for in EDs.5
Principles of Disease, Functional Anatomy, Physiology, and Examination of the Hand
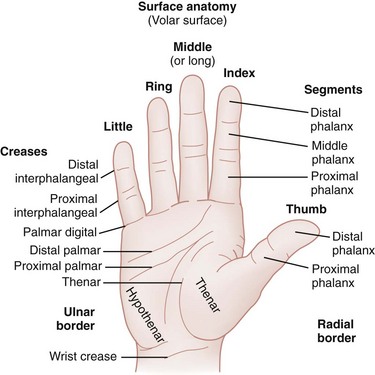
To avoid confusion, it is important that standard terminology for the surface anatomy of the hand be used (Fig. 50-1). The back of the hand and fingers is called the dorsal surface, and the palm side is called either the palmar or the volar surface. The borders of the hand are radial and ulnar. The five digits often are designated by numerals, but common names are preferable: I (thumb), II (index finger), III (long or middle finger), IV (ring finger), and V (little finger). Each finger has three joints: the metacarpophalangeal (MCP), the proximal interphalangeal (PIP), and the distal interphalangeal (DIP) joints. The thumb has an MCP joint and only one interphalangeal (IP) joint. There are proximal, middle, and distal phalanges in the fingers and only a proximal and a distal phalanx in the thumb. The thenar mass or eminence refers to the muscular area on the palmar surface overlying the thumb metacarpal. The hypothenar eminence is the muscle mass on the palmar surface overlying the little finger metacarpal.
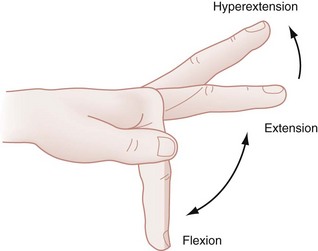
Hand and digit motion has been standardized and is illustrated in Figures 50-2 through 50-6. The carpometacarpal (CMC) joint is more mobile in the thumb than in the other fingers and is the key to the grasp and dexterity that characterize the human hand. Motions of this joint include palmar abduction (also called flexion), radial abduction, retroposition (extension), adduction, and opposition (see Fig. 50-6). The IP joints are essentially hinge joints and are capable of only two motions: flexion and extension.
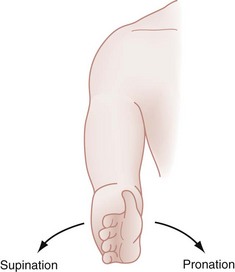
Figure 50-2 Supination and pronation of the hand.
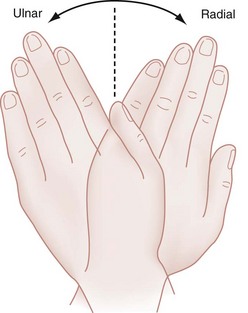
Figure 50-3 Ulnar and radial deviation of the hand.
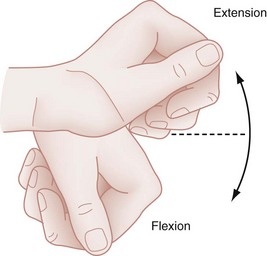
Figure 50-4 Wrist extension and flexion.
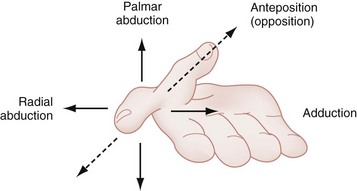
Figure 50-6 Perpendicular view of thumb mobility.
Structural Framework
The hand has two skin surfaces, each with different functions. The skin of the palm is thick compared with the dorsal skin and is stabilized by fibrous connections on its deep surface. The skin creases in the palmar aspect of the hand are largely transverse and represent adherence between skin and underlying fascia, without intervening adipose tissue. These features facilitate flexion and limit the development of inflammatory edema in the palm.6 The other noteworthy characteristic of the palmar skin is the unique arrangement of epithelial ridges of the dermis that form cutaneous striations. These ridges have forensic importance in the pulp as “fingerprints” and play an important role in increasing friction for grasping objects.7
The dorsal skin is relatively thin and mobile, permitting motion of the various joints. As a path of least resistance, the dorsum of the hand also swells easily after inflammation or trauma, which may limit flexion of the MCP joints.7 In addition, infection in the palmar aspect of the hand may cause dorsal swelling; this finding can be misleading without a careful physical examination.
Skeleton
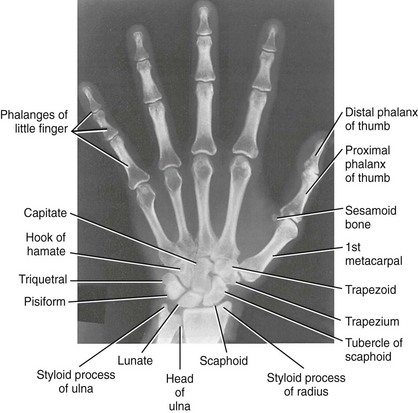
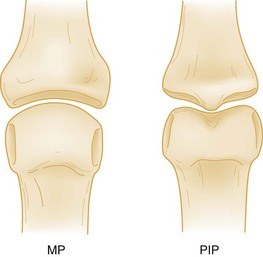
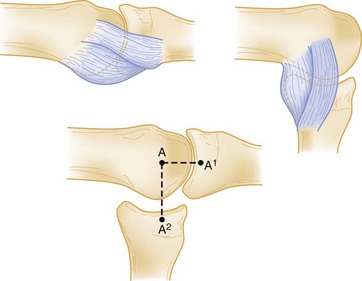
The hand and wrist contain 27 bones: 14 phalangeal bones, 5 metacarpal bones, and 8 carpal bones (Fig. 50-7). The eight small carpal bones in the region of the wrist are strongly united to one another by ligaments. These bones form synovial joints and are arranged in two rows, proximal and distal, with four bones in each row. Together the bones of the carpus present a concavity on their volar surface, which is bridged by a strong membranous band, the flexor retinaculum. In this way, the bridge and the bones form a tunnel, known as the carpal tunnel, through which pass the median nerve and the long flexor tendons of the fingers. The IP joints are inherently more stable than the MCP joint by virtue of their bicondylar configuration, which gives a modified tongue-in-groove appearance (Fig. 50-8).
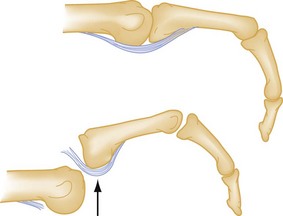
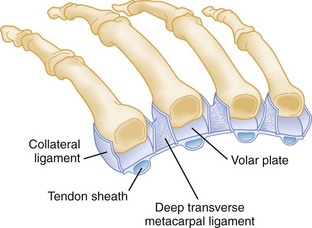
The soft tissue supporting these joints includes the capsular ligamentous structures, which afford stability, and the tendinous structures, which generate mobility. The metacarpal and IP joints are stabilized on both sides by collateral ligaments and anteriorly by a palmar fibrocartilaginous “volar plate.” Because of anatomic differences between the metacarpals and phalanges, the IP collaterals are tight throughout the entire range of motion, whereas the collaterals of the MCP joint are tightest in flexion (Fig. 50-9). The IP joints are hinges, but the MCP joint has additional side-to-side mobility and rotational movement to facilitate efficient grasp.7 The clinical importance of these differences is that for minimization of the development of contractures after joint injuries, the preferred position of immobilization of the PIP joints is extension, whereas the MCP joints are more properly placed in flexion.
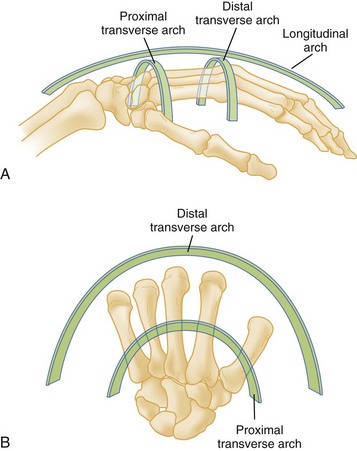
The structure and arrangement of the metacarpals are noteworthy. The metacarpals participate in three arches: the proximal (carpal) and distal (metacarpal) transverse arches and the longitudinal arch6 (Fig. 50-10). The index and long finger metacarpals form a fairly immobile segment because of their ridged articulation with the carpals. The adjacent metacarpals are more mobile. This unique anatomy gives the human palm a longitudinal and transverse concavity when the thumb is alongside the index finger; however, this changes to an oblique gutter when the thumb is extended.
The small bones of the child’s hand differ significantly from the bones of the adult and from other long bones because of the presence of an epiphysis or growth plate at one end of the bone. The phalangeal epiphyses and the thumb metacarpal epiphysis are located at the proximal end, and the finger metacarpal epiphyses are located at the distal end of the bone (Fig. 50-11). In boys the proximal phalangeal epiphysis appears at 15 to 24 months and fuses at 16 years. In girls it appears at 10 to 15 months and fuses at 14 years.8 The time of appearance and fusion is related to skeletal maturity and can be judged accurately until puberty from hand and wrist radiographs, because the sequence of development is age-specific.9
Muscle and Tendon Function
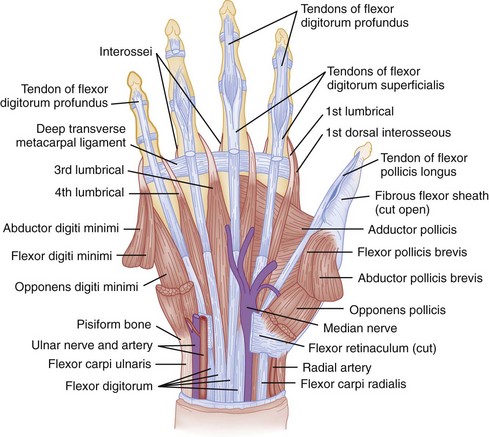
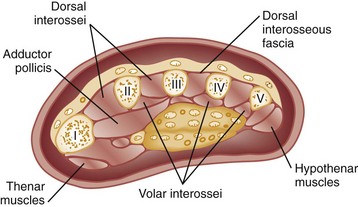
Intrinsic Musculature.: The intrinsic muscles of the hand include the muscles of the thenar and hypothenar eminences, the adductor pollicis, the interossei, and the lumbricals (Fig. 50-12). The thenar muscles cover the thumb metacarpal. This group includes the abductor pollicis brevis, opponens pollicis, and flexor pollicis brevis. These muscles originate in the flexor retinaculum and on the carpal bones and insert at the base of the first metacarpal and first proximal phalanx. They act in concert with the long flexors and extensors to carry the thumb through its intricate range of motion. The muscles are evaluated by palpation of the thenar eminence for contraction as the patient brings together the tips of the thumb and little finger. They also can be tested by asking the patient to place the dorsum of the hand on a flat surface and to raise the thumb up straight to form a 90-degree angle with the palm. The thenar muscles usually are innervated by the motor branch of the median nerve. In some cases they may be partially innervated by the ulnar nerve.
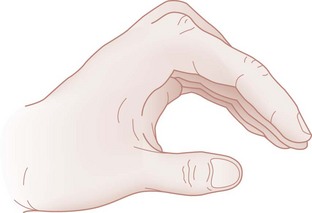
The adductor pollicis arises from the index and middle finger metacarpals and inserts on the first proximal phalanx. This muscle is innervated by the ulnar nerve. Thumb adduction is tested separately by having the patient forcibly hold a piece of paper between the thumb and radial side of the index proximal phalanx. If the adductor pollicis is weak or nonfunctioning, the thumb IP joint flexes with this maneuver (Froment’s paper sign).10 In this evaluation, the two hands should be compared.
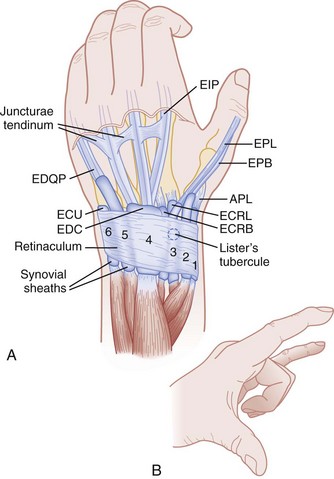
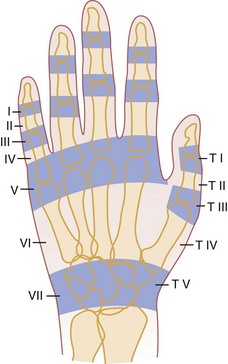
Extensor Tendons.: The extensor tendons are on the dorsal side of the forearm, wrist, and hand. The nine extensor tendons cross the wrist joint dorsal to its axis of rotation, pass under the extensor retinaculum, and are separated on the dorsum of the hand by a series of six fibro-osseous canals or compartments. Figure 50-13 outlines the compartments and their contents. The fibrous roof of these compartments prevents the tendons from bowstringing dorsally during active finger extension, particularly when the wrist also is extended.
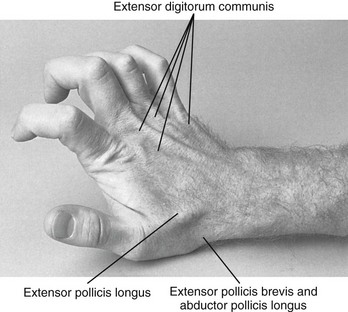
In the third compartment, a single tendon, the extensor pollicis longus, arises from the deep muscles of the midforearm, passes around a bony prominence on the dorsum of the wrist termed Lister‘s tubercle, and inserts on the base of the distal phalanx of the thumb. This tubercle can be palpated just proximal to the wrist joint. The extensor pollicis longus forms the dorsal border of the anatomic snuffbox, and the abductor pollicis longus forms the volar border (Fig. 50-14). The floor of this area contains the radial artery and two carpal bones, the scaphoid and trapezium. The extensor pollicis longus functions to extend and adduct the entire first ray and extend and hyperextend the IP joint of the thumb. This muscle is evaluated by placing the hand flat on a table and having the patient lift only the thumb off the surface. Because the abductor pollicis brevis and the adductor pollicis add terminal extension, complete laceration of the extensor pollicis longus tendon may not eliminate the patient’s ability to extend the thumb.11
The tendons that extend the fingers—the extensor indicis proprius and the extensor digitorum communis—are in the fourth compartment. The extensor digitorum muscle divides into four tendons proximal to the wrist. In the dorsum of the hand, these tendons are joined distally by fibrous interconnections called juncturae tendinum which help stabilize them to their insertions in the extensor expansions of the index, middle, ring, and little fingers. The extensor digiti minimi is contained in the fifth dorsal compartment. Both the extensor indicis proprius and the extensor digiti minimi typically lie ulnar to their respective common extensor tendons. The dual extensor system for the index and small fingers gives these two digits extension independent of the other digits. The middle finger and especially the ring finger have considerably limited independent extension. The motion restriction is because of the juncturae, which also prevents retraction of the proximal tendon end after distal transection of an extensor. Complete severance of an extensor proximal to the juncturae can be associated with normal MCP joint extension.7 This extension occurs through the juncturae connections. The extensor digitorum communis tendons can be evaluated by asking the patient to straighten out all of the fingers. The function of the extensor indicis proprius can be isolated from the common extensors by asking the patient to make a fist and then to point the index finger. The extensor digiti minimi is examined by having the patient straighten the little finger while the hand is closed into a fist.
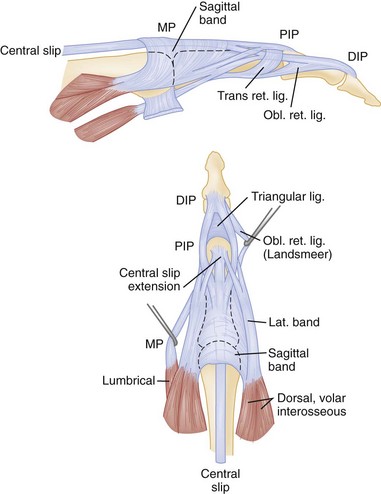
The extensor mechanism of each digit is a complex interrelationship of muscle-tendon units of the long extrinsic extensor tendons and the intrinsic system (Fig. 50-15). The extensor expansion divides into a central slip that attaches to the middle phalanx and two lateral bands that join with the tendons of the lumbrical and interosseous muscles and attach to the base of each distal phalanx. The interossei and lumbrical muscles insert in the lateral aspects of the dorsal hood. Most of the power of the common extensors serves to extend the MCP joint. Distal digit extension is provided by continuation of the lateral band mechanism and the oblique retinacular ligament. Because of this complex anatomy, injuries involving the extensor mechanism require meticulous repair.
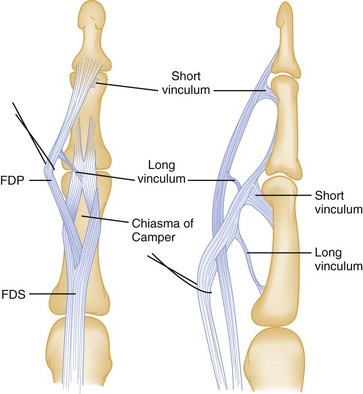
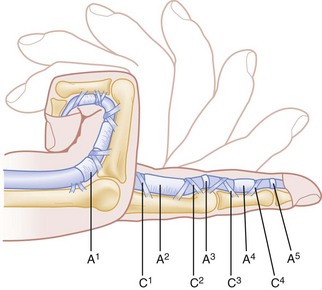
Flexor Tendons.: The flexor tendons reside on the volar side of the forearm and cross the wrist joint volar to its axis. In general, 12 tendons function to flex the wrist and digits; three of them—the flexor carpi radialis, flexor carpi ulnaris, and palmaris longus—primarily flex the wrist and deviate the wrist radially or ulnarly (Fig. 50-16). The remaining tendons pass into the digits through the carpal tunnel. A single tendon, the flexor pollicis longus, inserts on the distal phalanx of the thumb, and two flexor tendons go to each remaining finger. The flexor digitorum superficialis (FDS) tendons bifurcate near the base of the proximal phalanges and surround the tendons of the FDP before inserting on the middle phalanges of the index, middle, ring, and little fingers (Fig. 50-17). The FDS flexes all the joints it crosses, including the wrist, PIP joints, and MCP joints. The profundus tendons lie deep to the superficialis tendons over most of their course in the forearm. At the level of the MCP joint, they perforate the superficialis tendon to emerge to a superficial position. They insert at the base of the distal phalanx and act primarily to flex the DIP joint and all joints flexed by the FDS. From the level of the MCP joint distally, the two flexor tendons become enclosed in a fibrous flexor sheath lined by synovium. Regions of thickening in this sheath form pulleys that help prevent bowstringing of the flexor tendons across the joint and assist smooth, effective flexion (Fig. 50-18).
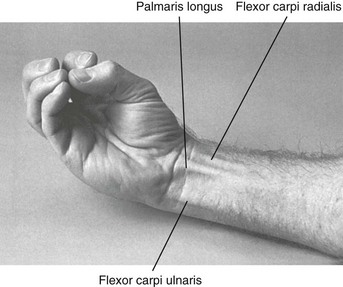
Figure 50-16 Palmaris longus accentuation.
After observation, each muscle-tendon unit is tested with a functional examination. The flexor carpi radialis, palmaris longus, and flexor carpi ulnaris are tested together by having the patient flex the wrist against resistance while the examiner palpates the individual tendons. The tendon of the flexor pollicis longus attaches to the base of the distal phalanx of the thumb and flexes the thumb MCP and IP joints. This tendon is tested by having the patient bend the tip of the thumb against resistance. FDP function can be tested by having the patient flex the distal phalanx of each finger while the PIP is stabilized in extension by the examiner (Fig. 50-19). The FDS is tested individually by asking the patient to flex the PIP joint while the other fingers are held in extension to block the flexion produced by the profundus tendons (Fig. 50-20). This is a subtle but important distinction, because lacerations of the digital creases can easily damage one or more of the tendons or adjacent neurovascular bundles. The FDP is more commonly lacerated in the finger because of its paradoxically superficial position.
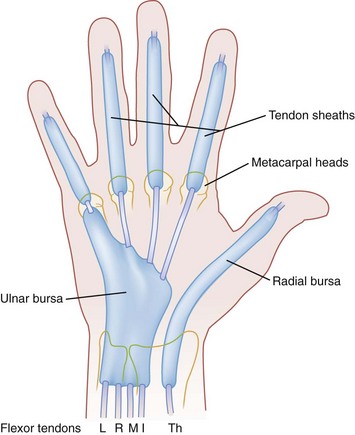
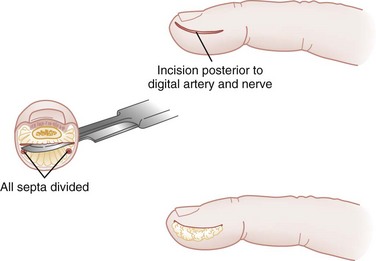
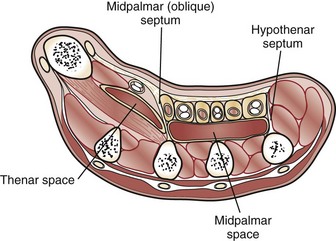
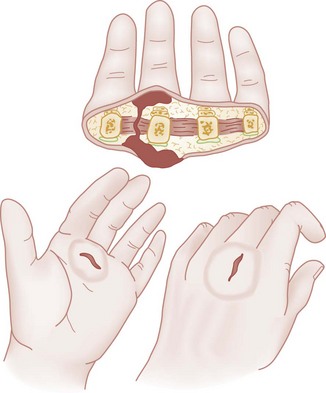
Synovial Spaces.: Bursae are synovial sheaths that cover tendons as they pass through osseofibrous tunnels. They contain synovial fluid and serve two essential functions: They decrease friction during tendon movement, and they help supply nutrients to the relatively avascular tendons (Fig. 50-21). These sheaths also can provide pathways for spread of infection. Extensor tendons do not lie within definite sheaths and are afforded a greater resistance to infections. The synovial sheaths of the flexors in the index, middle, and ring fingers are enclosed from their insertion to approximately the level of the distal palmar crease. The sheath of the flexor pollicis longus extends from the tip of the thumb to the proximal volar wrist crease, where it communicates with the radial bursa in the palm and carpal tunnel. Similarly, the synovial sheath of the little finger communicates with the ulnar bursa. Clinical features of flexor tenosynovitis are caused by inflammation and distention of these synovial sheaths. Kanavel12 described the classic signs: a semiflexed posture of the digit, pain on passive extension of the digit, fusiform swelling, and tenderness of the synovial sheath.
Blood Supply
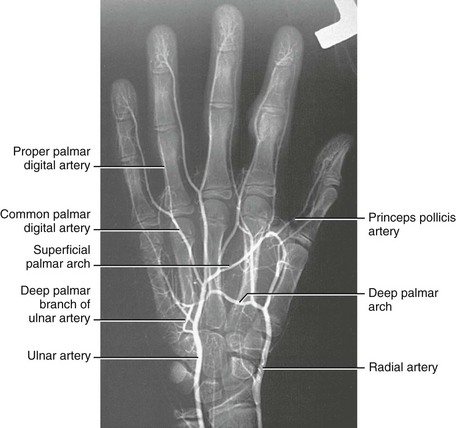
Arterial System.: The hands and the digits have a dual blood supply (Fig. 50-22). The major blood supply to the hand is from the radial and ulnar arteries. The radial artery lies on the anterior aspect of the radius in the distal part of the forearm. It continues around the lateral side of the wrist onto the dorsum of the hand by passing deep to the tendons of the abductor pollicis longus and the extensor pollicis brevis. On entering the palm, the radial artery terminates as the deep palmar arch. The ulnar artery enters the hand anterior to the flexor retinaculum on the radial side of the ulnar nerve and pisiform bone. The artery gives off a deep branch and then continues into the palm as the superficial palmar arch. This complex arterial arch system anastomoses and sends branches to the individual digits and the deep palmar spaces. Because of extensive collateralization, the hand usually survives even if both vessels are transected at the wrist.13 The circulation of the hand is evaluated by palpation of the radial and ulnar arteries on the volar aspect of the wrist, by assessment of the color and warmth of the skin, and by testing of capillary refill. Because “normal” findings vary among patients, the injured hand should be compared with the unaffected side.
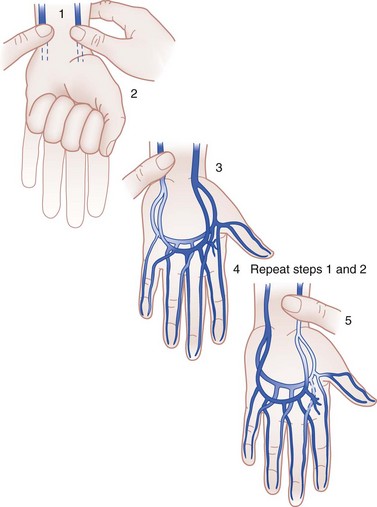
Although Allen’s test is an imperfect predictor of vascular compromise, it is commonly used to determine the patency of the arteries supplying the hand and the contributions to the circulation of the hand derived from each of the major vessels. The radial and ulnar arteries are compressed by the examiner at the wrist (Fig. 50-23). The patient opens and closes the hand repeatedly to exsanguinate it and then maintains a relaxed position. The radial artery is released. If the palm and fingers fill immediately with blood, the radial artery is patent, with good collateral flow into the ulnar artery system. To evaluate the ulnar artery, the same steps are repeated, but the ulnar artery is released. This method also can be used on a single digit to help evaluate the patency of each digital artery to that finger. Unilateral digital artery injuries may be well tolerated owing to adequate collateral circulation from the uninjured side. Bilateral digital artery injuries, although rare, tend to have poor outcomes.13,13a,13b
Venous and Lymphatic Systems.: The veins generally follow the arterial pattern in the deep system. The abundant dorsal, superficial veins are more extensive than the deep system and drain most of the blood from this region. The lymphatic vessels essentially follow the veins, with most lymph flowing into channels in the dorsal subcutaneous space. This vascular anatomy and the laxity of the dorsal skin account for palmar infections causing swelling on the dorsum rather than on the palmar surface of the hand.
Nerve Supply
Motor Innervation.: The radial nerve (formed from nerve roots C6 through C8) passes through the supinator muscle and enters the dorsal aspect of the wrist between the radial styloid and Lister’s tubercle. At this level, the nerve has a purely sensory function. Its important motor function is to innervate the dorsal extrinsic muscles in the forearm, which extend the wrist and MCP joints and abduct and extend the thumb. No intrinsic muscles in the hand are innervated by the radial nerve. Motor function in this nerve is tested by having the patient extend the wrist against resistance. Proximal injury to the radial nerve causes a condition known as wristdrop: The fingers are held in flexion at the MCP joints, and the thumb is adducted (Fig. 50-24A).
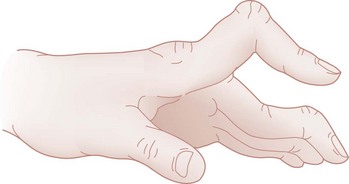
The ulnar nerve (C7, C8, and T1) passes through the flexor carpi ulnaris muscle in the forearm and lies ulnar to the artery and superficial to the flexor retinaculum. It enters the hand at the wrist through the ulnar tunnel, or Guyon’s canal. The ulnar nerve innervates the hypothenar muscles, the seven interosseous muscles, the lumbrical muscles to the ring and little fingers, and the adductor pollicis. Innervation of the flexor pollicis brevis is variable. In the forearm, the flexor carpi ulnaris and the ulnar half of the FDP also are innervated by the ulnar nerve. Loss of motor function of the ulnar nerve results in inability to pinch a piece of paper tightly between the thumb and the index finger. A late characteristic of distal ulnar damage is Duchenne’s sign, manifested by clawing of the ring and little fingers (see Fig. 50-24B). The ring and little fingers are hyperextended at the MCP joints by the extensor digitorum communis (radial nerve) and flexed at the IP joints by the FDP (intact proximal ulnar nerve). In addition, the interosseous and hypothenar muscles are atrophied.
The median nerve enters the forearm through the pronator teres muscle. At that level, it innervates that muscle, the flexor carpi radialis, the FDS, the radial part of the FDP, the flexor pollicis longus, and the pronator quadratus. The branch of the median nerve that innervates the last three muscles is called the anterior interosseous nerve. The median nerve enters the hand through the carpal tunnel accompanied by the nine extrinsic flexor tendons of the digits. The thenar motor branch (recurrent median nerve) innervates the abductor pollicis brevis, the opponens pollicis variably, and the flexor pollicis brevis. Common digital branches innervate the lumbrical muscles to the index and long fingers. Injury to this nerve occurs most commonly at the level of the wrist, by laceration or by compression in the carpal tunnel. Motor function is tested by having the patient appose the thumb to the index digit. Injury to the median nerve in the upper forearm or at the elbow usually results in weakness or absence of flexion of the index finger distal phalanx, the middle phalanx, and the thumb and weakness of thumb abduction and opposition. With passage of time, the muscles of the thenar eminence atrophy, leaving the hand with a flattened and “apelike” appearance (see Fig. 50-24C).
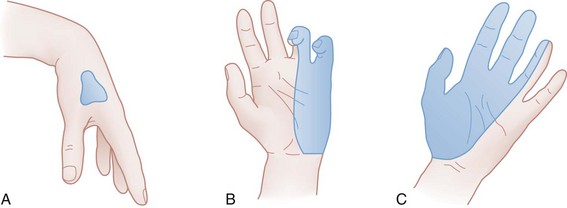
Sensory Innervation.: The typical distribution of the sensory nerves to the hand is shown in Figure 50-25. Because some overlap occurs between various sensory nerves, it is preferable to test sensation in the areas least likely to have dual innervation. The anatomic area of least ulnar variation and overlap is the volar tip of the little finger. The median nerve exclusively innervates the volar tip of the index finger. The dorsal first web space is entirely within the radial nerve distribution.
Several methods exist to assess sensation. Two-point discrimination is one such method, although both the accuracy and objectivity of this test have been called into question.14 An uninjured hand is able to distinguish two points that are 2 to 5 mm apart at the fingertips and 7 to 10 mm apart at the base of the palm. The dorsum of the hand is the least sensitive region, with a normal threshold at 7 to 12 mm. Two-point threshold distances wider than these ranges indicate impaired sensory function.14 The threshold and two-point discrimination tests may be of limited value in children, patients with heavily calloused fingertips, uncooperative patients, comatose patients, patients in severe pain, or suspected malingerers. In such patients, submerging the hand in water and observing the skin for the development of wrinkles has been offered as a way to diagnose nerve impairment because denervated skin will not wrinkle.15
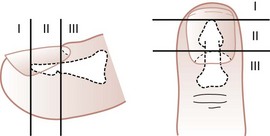
Fingertip
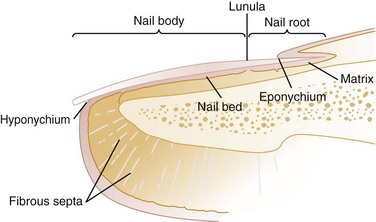
The fingertip generally is defined as the area distal to the insertion of the flexor profundus and extensor tendons (Fig. 50-26). The pulp is the tissue of the fingertip between the volar skin and the distal phalangeal bone. The fingertip is well padded by adipose tissue and is covered by highly innervated skin that is tethered to the distal phalanx by a series of fibrosepta. The dorsal skin is thinner and less vascularized than the volar skin. Sensation is supplied by nerves that travel with arteries bilaterally along the radial and ulnar aspects of the fingers. The arteries branch to form volar anastomoses or arches similar to those in the palm. Dorsal branches supply the nail bed and matrix.
Nail
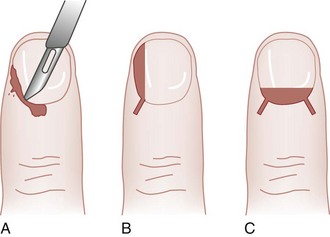
The nail bed complex is important in providing additional stabilization of the palmar soft tissues against compression and shear forces. The nail grows from the nail matrix along the nail bed and is firmly adherent to the bed. It is now believed that the entire nail bed is active in the generation and migration of the nail. As new nail forms, it glides forward over the nail bed at a rate of approximately 0.5 to 1.2 mm per week (toenails grow much more slowly). The nail itself is a hard, firm, and relatively translucent structure; the underlying vascular tissue showing through gives the nail its pink appearance. A smooth nail bed is essential to normal function. If the nail bed sustains injury that is not repaired accurately, granulation tissue forms scar that impedes normal nail production and growth. The result may be a split or absent nail that is cosmetically unappealing and sometimes functionally debilitating.16
Clinical Features: Signs and Symptoms
The initial evaluation of an acutely injured hand is crucial because it affords the best opportunity for accurate assessment of the extent of damage and for restoration of altered anatomy.17 Evaluation of any hand injury should begin by obtaining the historical facts of the patient’s age, occupation, hand dominance, and previous hand impairment or injury. In traumatic injuries, elapsed time since the injury, mechanism of injury, posture of the hand at the time of injury, and treatment before arrival in the ED all are useful data. In nontraumatic problems, pain, swelling, sensory change, contracture, timing of symptoms, presence of similar symptoms in other extremities, aggravating or alleviating factors, and functional impairment are useful historical points. A review of the medical history and a review of systems complete the evaluation.
After a detailed history is taken, the entire extremity should be exposed and evaluated when the hand is examined. A system of priorities, based primarily on threat to ultimate function, should direct the sequence of the examination. In order of priority, the examination includes evaluation of vascular and neurologic integrity, skin cover, skeletal stability, and joint and tendon function (Box 50-1). The general appearance of the hand should be noted, with focus on its color, presence of swelling or edema, and any abnormal posture or position. In traumatic injuries, the precise area of maximal tenderness should be localized. Rotational, angular, and shortening deformities should be noted with regard to direction and extent. Angular deformity may be seen best with the fingers in full extension. Rotational deformity is best observed during digital flexion. Digital or wrist block anesthesia may be helpful in some cases to accurately assess fracture deformity and stability during digital motion and, if necessary, stress testing. Open wounds should be assessed with regard to location, relationship to skin creases, direction and viability of skin flaps, extent of skin loss, degree of contamination of the wound, and extent of soft tissue injury. The examiner should have good light, adequate exposure, and a nearly bloodless field for a thorough evaluation. The complete examination also may require an evaluation of active shoulder motion, elbow motion, and pronation and supination of the forearm and assessment of the contralateral hand.
Diagnostic Strategies: Radiology
Despite the development of numerous new and sophisticated imaging techniques, plain radiography remains the most important imaging modality for the hand and wrist. The standard radiographic series of the hand should include a posteroanterior, a true lateral, and an oblique projection (Fig. 50-27). With correct positioning, the bones do not overlap on the film, allowing complete evaluation of each area for visualization of fractures, subluxation, dislocation, deformities, and retained radiopaque foreign bodies.18 On a hand series, the wrist is not properly positioned for radiographic examination, and vice versa; if the patient has injuries to the hand and wrist, separate radiographic series should be obtained.
For an adequate posteroanterior view, the forearm and hand should be fully pronated so that the palm rests flat on the film. This view forms the basis for all assessments but is poor at showing fractures of the articular surface of the metacarpal head. The lateral view normally is a radioulnar projection and is made by positioning the palm and forearm at 90 degrees to the film with the fingers splayed. This view is essential to show displacement of fracture fragments and joint dislocations. If the projection is not a true lateral view, joint dislocation, avulsion fractures, or fractures through the articular surface of the base of the phalanx may be overlooked. The oblique view is obtained with the hand and forearm pronated at 45 degrees to the film. It is particularly useful for assessing dislocation of the MCP and CMC joints and fractures at the base of the metacarpal bones. When injury is confined to the distal end of a single digit, radiologic evaluation should be limited to that digit, but the same projections are used (Fig. 50-28).
Special views are used to diagnose specific injuries. The standard views of the hand do not give true posteroanterior and lateral projections of the thumb because the plane of the thumb is at 90 degrees to that of the fingers. Separate posteroanterior and lateral views of the thumb should be requested. The posteroanterior projection of the thumb is obtained with the hand and forearm hyperpronated so that the dorsal surface of the thumb and the thumb metacarpal rests flat on the film. The lateral view is obtained by pronating the hand and forearm to allow the lateral surface of the thumb to lie on the film. Stress views are used most often to rule out ligamentous injury to the first MCP joint. Localized widening of the joint space or subluxation may indicate a significant collateral ligament injury. Plain radiographs taken in multiple projections can help detect and localize soft tissue foreign bodies. Whether an object can be visualized will depend on its composition, configuration, size, and orientation. Many foreign bodies encountered in the ED, including almost all glass, are more dense than soft tissue and can be readily seen on plain radiographs.19 Plastic and wood foreign bodies are notable exceptions, with many of these objects being radiolucent.
Mechanisms of Injury and Management
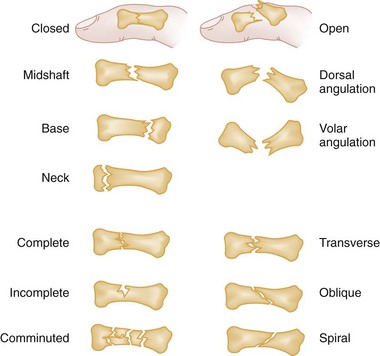
The bones of the hand are the most commonly fractured bones in the body. Radiologic evaluation of significant hand injuries is mandatory. Any hand injury that causes swelling should be evaluated radiographically with a minimum of three views. Although the classification of hand fractures is difficult and at times confusing, it generally is done according to the nature and site of the fracture line and whether the fracture is open or closed (Fig. 50-29).
In general, transverse fractures have a stable configuration. Spiral, oblique, and comminuted fractures are unstable. The degree of displacement also is an indicator of potential fracture instability. Fractures of inherently unstable configuration may be stable if they are nondisplaced or only minimally displaced because the periosteum is undamaged or minimally disrupted. Displacement is defined by the deformity it creates and can result in rotation, angulation, shortening, or a combination of these fractures. Although shortening has an adverse effect on muscle tension, the hand accommodates more easily to this component of deformity than to others.18
Distal Phalanx Fractures
Pathophysiology and Clinical Features
Fractures of the distal phalanx are the most common fractures of the hand. They occur most often as a result of crush or shearing forces, usually as a sports-related injury in children and adolescents, industrial accidents in adults, or accidental falls in elderly persons.20 Distal phalangeal fractures are classified as extra-articular fractures (longitudinal, transverse, and comminuted) or intra-articular fractures. The most common location for these fractures is the distal tuft (Fig. 50-30). Because the mechanism of injury is usually direct trauma, tuft fractures often are comminuted and usually are associated with soft tissue injury to the nail, nail bed, and nail matrix.21 Supporting fibrous septa that radiate from the bone to the skin prevent displacement of fracture fragments and act to contain soft tissue swelling, contributing to the severe pain that can accompany these fractures. Examination typically reveals tenderness and swelling over the distal phalanx, including the pulp.
Management
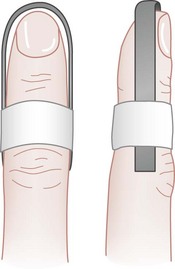
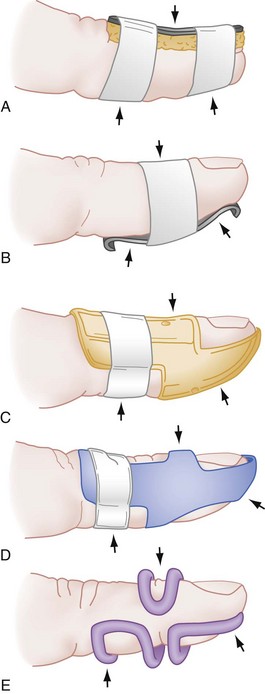
Treatment of most fractures of the distal phalanges is directed toward the accompanying soft tissue injury. Closed tuft fractures need only symptomatic treatment with elevation (to reduce swelling) and analgesics. Fracture immobilization is rarely necessary; however, a short volar splint or hairpin splint (Fig. 50-31) is recommended for 2 to 3 days to protect the tip of the finger from further trauma and allow swelling without constriction. Immobilization should not include the PIP joint. Transverse shaft fractures with angulation or displacement may be irreducible because of interposition of soft tissue. Closed reduction may be attempted with dorsal traction on the distal fragment followed by immobilization with a volar splint and repeat radiographs for documentation of position. If this approach is unsuccessful, referral to a hand surgeon is indicated for Kirschner wire fixation.21
Complications
Distal phalanx fractures generally are uncomplicated; however, distal phalanx fractures that appear innocuous can result in prolonged morbidity, especially if associated with soft tissue crush injury. In a long-term follow-up series, DaCruz and associates22 showed that at 6 months 31% of tuft fractures had not healed radiographically and 70% of all patients had bothersome symptoms, including numbness, hyperesthesia, and cold sensitivity. Trauma to the nail bed may result in abnormal nail growth despite exact tissue approximation. Failure to recognize and extricate an entrapped nail bed in the fracture site may result in nonunion of the fracture. Osteomyelitis from open fractures is a rare but potentially serious complication.
Proximal and Middle Phalangeal Fractures
Pathophysiology and Clinical Features
Because the anatomy, mechanism of injury, and treatment for proximal and middle phalangeal fractures are similar, these fractures are discussed together. The proximal phalanx has no tendinous attachments. Fractures in this region have a typical volar angulation resulting from forces exerted from the extensors and the interosseous muscles. The middle phalanx has two important insertions. The tendon of the FDS divides and inserts along nearly the entire volar surface of the phalanx, and the extensor tendon inserts on the proximal dorsal base of the middle phalanx. Because of this alignment, fractures at the base of the middle phalanx usually result in dorsal angulation, and fractures at the neck of the middle phalanx usually result in volar angulation.23 The mechanism of injury often determines the nature of the fracture; a direct blow is more likely to cause a transverse or comminuted fracture, whereas a twisting injury more often results in an oblique or spiral fracture. Associated injuries may include contusion or transection of digital nerves, vascular disruption, and tendon rupture.
Intra-articular fractures include condylar fractures; comminuted fractures; dorsal, volar, or lateral base fractures; fracture-dislocations; and shaft fractures involving the joint. Extra-articular fractures involve the neck, shaft, or base of the phalanx. Although most phalangeal fractures may be easily seen, condylar fractures and displaced neck fractures are not always apparent on anteroposterior radiographs; oblique views may be needed to identify them.24 Rotational deformities are difficult to determine by radiologic study but may appear on the lateral view as discrepancies in the diameter of the shaft at the fracture site.
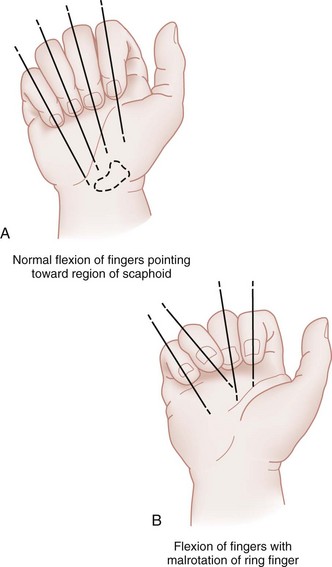
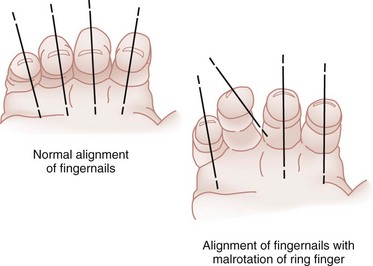
Skeletal alignment can be assessed radiographically, but rotational alignment should be judged clinically by the relationship of the finger to adjacent normal fingers (Fig. 50-32). Symmetrical flexion of adjacent injured and normal fingers at their MCP and PIP joints is the best possible guide to accurate rotational alignment of the injured segment.23 Normally, all of the fingers of the closed fist except the thumb should point to the scaphoid. Alternatively, when the fingers are loosely flexed, the nails of opposing digits should lie in the same parallel plane (Fig. 50-33). The uninjured hand should be used for comparison.
Management
Similar to metacarpal fractures, phalangeal fractures require precise anatomic alignment to ensure a good result because of the intimate relationship of the flexor and extensor tendons to the phalanx.23 Appropriate treatment selection depends on accurate assessment of fracture stability. The angle of the fracture is an important factor in determining this stability. Transverse fractures usually are stable, whereas oblique fractures are inherently unstable. It also is important to ascertain whether the fracture has been impacted or displaced and what deforming forces are acting on it. If there is any question of the fracture’s stability, the digit should be anesthetized, and stress should be applied. Reduction of phalangeal fractures usually is not necessary because most are stable and nondisplaced.17 Patients with such fractures should be started on early protected motion as soon as pain subsides (within the first 3 to 5 days). Protection is provided by taping the injured digit to an adjacent, larger normal finger proximally, a form of dynamic splinting. This technique, known as “buddy-taping,” encourages the patient to move the finger and use the hand as normally as possible while the fracture heals (Fig. 50-34).
If the fracture is displaced or unstable, it is not suitable for dynamic splinting. In general, treatment depends on the type of trauma and the ability to achieve a stable reduction. Phalangeal fractures that are satisfactorily managed by closed reduction can be immobilized by several methods. In such cases it is advisable to immobilize the wrist and the injured finger. Specific types of immobilization include circular cast, the Böhler method of incorporating a cast with an outrigger, gutter splints, and anterior and posterior splints (Fig. 50-35). The period of immobilization of phalangeal fractures should not exceed 3 weeks, to prevent stiffness and to minimize disability. In addition to temporary immobilization, ED management includes ice for comfort, elevation, analgesics, and referral for follow-up care. Repeat radiographs in 7 to 10 days are recommended to ensure that no delayed displacement has occurred.
Unstable fractures that cannot be reduced by closed manipulation and maintained with external splinting require internal fixation. Midshaft transverse fractures tend not to be amenable to closed reduction; similarly, spiral oblique fractures and intra-articular fractures are inherently unstable and require surgical fixation if a significant portion of the articular surface is involved.25 Intra-articular fractures of the proximal metaphysis of the middle phalanx that have extreme comminution may require treatment in static or dynamic traction or external fixation with or without ancillary Kirschner wire fixation.25
Complications
Malunion is the most common bony complication of phalangeal fractures and may result from malrotation, volar or lateral angulation, or shortening. Malrotation usually is seen after oblique or spiral fractures of the proximal and middle phalanges and may require osteotomy through the phalanx or metacarpal for correction. Volar angulation of proximal phalangeal fractures greater than 25 to 30 degrees results in pseudoclawing. This deformity makes use of the hand awkward and is esthetically unacceptable. Other potential complications include diminished motion resulting from tendon adhesions and stiffness of the PIP joint after intra-articular fractures with incongruity.23
Metacarpal Fractures
Metacarpal Fractures of the Index, Middle, Ring, and Little Fingers
The hand can adjust functionally to dorsal angulation in the metacarpal equal to its motion at the CMC joint, plus 10 to 15 degrees in some patients. Because the index and middle fingers are immobile at their CMC joints, they may accommodate only 10 to 15 degrees of dorsal angulation. The ring finger usually has 20 to 30 degrees of mobility at its CMC joint and may accommodate 40 to 45 degrees of dorsal angulation. The small finger generally has 30 to 50 degrees of motion at its base and may accommodate 50 to 70 degrees of dorsal angulation. Finger metacarpals may tolerate 10 to 15 degrees of lateral angulation and 3 to 4 mm of shortening. Rotational deformity, most commonly seen in spiral and oblique fractures, is poorly tolerated. A small amount of rotational deformity can translate into a substantial digital overlap when the fingers are closed to form a fist. Just 10 degrees of malrotation may cause as much as 2 cm of overlapping (scissoring) of the fingers during flexion.17 Surgical intervention is indicated with 2 to 3 mm of shortening, 1 mm of articular surface step-off, greater than 25% articular involvement, or any degree of malrotation.23
Metacarpal Head Fractures
Pathophysiology.: Fractures of the metacarpal head are rare. They usually occur as a result of direct trauma or crush injury and typically are comminuted.21 These fractures occur distal to the attachment of the collateral ligaments. Physical examination reveals tenderness and swelling over the involved MCP joint. Pain is increased if axial compression is applied along the extended digit. The presence of lacerations over the metacarpal heads is significant and suggests the possibility of an open fracture potentially caused by human bite injury.
Diagnostic Strategies: Radiology.: Although routine radiographic imaging of the injured hand reveals most fractures, the metacarpal heads can be difficult to assess because of overlap on the lateral view. In such cases in which clinical suspicion of a fracture exists and the initial radiographic appearance is normal, the Brewerton “ball-catcher’s” view may be helpful.26 This view is obtained with the digits in 65 degrees of flexion at the MCP joints and the x-ray beam angled 15 degrees radially, projecting the metacarpal heads in profile. Occasionally, computed tomography also may be required to evaluate accurately the degree of displacement of intra-articular fractures at the MCP level.
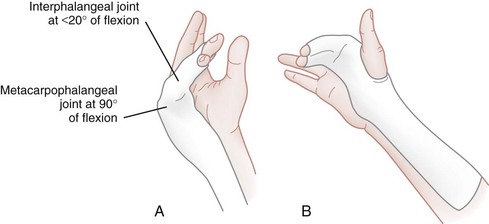
Management.: Emergency management of closed metacarpal head fractures consists of elevation, ice for comfort, analgesics, and immobilization of the hand in the “safe” or functional position, which balances the forces of the intrinsic muscles. In this position, shown in Figure 50-36, the wrist is extended 20 degrees, the MCP joints are flexed to 90 degrees, and the PIP and the DIP joints are extended. Referral to a hand surgeon for management and follow-up evaluation is required in all cases. Because these are intra-articular fractures, displacement by more than 1 to 2 mm predisposes the patient to a poor result; however, little consensus has been reached regarding optimal definitive treatment.27
Lacerations or puncture wounds over the dorsum of the MCP joint associated with a metacarpal head fracture should be considered open until proven otherwise. Such injuries often are caused by a clenched-fist injury and are highly contaminated wounds. Emergent consultation with a hand surgeon for operative débridement and irrigation is recommended. Prophylactic coverage with a cephalosporin is routinely recommended, although patients with highly contaminated wounds should receive penicillin with a β-lactamase inhibitor and an aminoglycoside.28 Several studies have found preoperative wound cultures to be of no value in predicting the risk of infection or identifying the likely pathogen, and some clinicians have abandoned their use.29,30
Complications.: Metacarpal head fractures may be associated with debilitating hand complications, including avascular necrosis, rotational malalignment, interosseous muscle fibrosis, extensor tendon injury or fibrosis, and chronic stiffness of the MCP joint. Many of these fractures also may require late arthroplasty.21
Metacarpal Neck Fractures
Pathophysiology.: Fractures of the metacarpal neck are among the most common fractures in the hand. The mechanism of injury is a direct impaction force (e.g., a punch with a closed fist). A boxer‘s fracture is a fracture of the neck of the little finger metacarpal (Fig. 50-37). Most metacarpal neck fractures have a typical apex dorsal angulation. They are inherently unstable because of the deforming muscle forces and frequent comminution of the volar cortex. Management generally is difficult because of this instability and the difficulty in maintaining reduction.
Management.: For treatment purposes, metacarpal neck fractures are divided into two groups: fractures involving the ring and little finger metacarpals and fractures involving the index and long finger metacarpals. There is considerably more mobility of the metacarpals of the ring and little fingers compared with the index and long fingers. This greater mobility makes them more prone to fracture, and the relative immobility of the index and long finger metacarpals increases the need for accurate alignment after reduction. In general, less than 15 degrees is allowed in the index and long finger metacarpals; in the ring and little finger metacarpals, 35 degrees and 45 degrees of angulation, respectively, are allowed. Any rotational malalignment should be completely corrected.
Nondisplaced ring and little finger metacarpal fractures without angulation deformity can be treated initially with ice, limb elevation, analgesia, and immobilization in a gutter splint. Nondisplaced, nonangulated metacarpal fractures of the index and long finger metacarpals are treated similarly. The splint should be in standard position of function and extend from below the elbow up to, but not including, the PIP joint. In general, it is recommended to begin PIP and DIP motion without delay. Protected MCP motion can begin in 3 to 4 weeks.21 For isolated fractures of the little finger metacarpal neck, some clinicians advocate immediate mobilization of fractures regardless of the degree of angulation. Results with this approach include excellent function, with only minor cosmetic deformity, and early return to work. Early follow-up evaluation is advised to exclude residual angulation, rotational deformity, and delayed displacement.31
Reduction of ring and little finger metacarpal neck fractures with significant angulation or deformity may be attempted in the ED. After appropriate anesthesia is obtained, usually with a hematoma block or an ulnar nerve block, traction is applied on the metacarpal to disimpact the fracture. The MCP joints and IP joints are flexed at 90 degrees, and simultaneous pressure is applied in a volar direction over the metacarpal shaft and in a dorsal direction over the flexed PIP joint (Fig. 50-38). This maneuver is termed the 90-90 method and should complete reduction. A gutter splint in position of function should be applied. Postreduction radiographs should be obtained immediately and after 1 week to ensure that reduction has not been lost. If closed reduction cannot be achieved or maintained, pin fixation by a hand surgeon is necessary, and early referral is indicated.
Complications.: Metacarpal neck fractures may have an associated rotational component that can impair function and result in overlapping of the affected finger over an adjacent finger. If excessive angulation is not corrected, the patient may experience forced hyperextension of the MCP joint and flexion of the PIP joint when extending the finger and pain when tightly grasping objects. Other complications include extensor tendon injury and collateral ligament damage. Nonunion is rare after closed metacarpal fractures.
Metacarpal Shaft Fractures
Pathophysiology.: There are three types of metacarpal shaft fractures: transverse, oblique or spiral, and comminuted. Transverse and comminuted fractures usually result from a direct blow and commonly exhibit dorsal angulation (Fig. 50-39). Indirect trauma or rotational torque applied to the finger may result in a spiral shaft fracture. These fracture fragments tend to shorten and rotate rather than angulate.
Management.: Metacarpal shaft fractures are treated differently than fractures involving the neck because rotational deformity and shortening are more likely and less angular deformity is acceptable. In general, any rotational deformity should be corrected. Angulation deformities are unacceptable in the index and long finger metacarpals, whereas a small amount of angulation may be compensated for in the ring and little finger metacarpals. Acceptable reduction is less than 10 degrees of angulation in the former and less than 20 degrees in the latter, with less than 3 mm of shortening and normal rotational alignment.21
Most metacarpal shaft fractures can be managed initially with ice, limb elevation, analgesia, and immobilization in a gutter splint. The splint should include the wrist and the entire metacarpal shaft, but not the MCP joint if the fracture is proximal to the neck. Repeat radiographic examination and referral to a hand surgeon are recommended. If manipulative reduction is necessary, operative fixation usually is indicated. Multiple displaced metacarpal shaft fractures, oblique or spiral fractures with rotational deformity, irreducible transverse fractures, and displaced open fractures require internal fixation.31
Metacarpal Base Fractures
Clinical Features.: Fractures of the metacarpal base generally are stable and occur infrequently. They may result from either a direct blow over the base of the metacarpal or an axial force or torque applied along the digit. Examination reveals tenderness and swelling at the base of the involved metacarpal, and a significant degree of rotational deformity may be evident. Fractures at the base of the ring or little finger metacarpals may cause injury to the motor branch of the ulnar nerve, resulting in paralysis of the intrinsic hand muscles. In addition, they may be associated with a carpal bone fracture.
Thumb Metacarpal Fractures
Extra-articular Fractures.: Extra-articular fractures are seen more commonly than intra-articular fractures and usually result from direct trauma or impaction. The three types of extra-articular fractures are transverse, oblique, and, in children, epiphyseal. Examination reveals localized pain and swelling over the fracture site.
Mobility of the thumb metacarpal allows 20 to 30 degrees of angular deformity without functional impairment. Patients with extra-articular fractures with a greater degree of angulation should undergo closed reduction, postreduction radiographic evaluation, and immobilization of the thumb in abduction with its IP joint extended with a thumb spica cast for 4 weeks. Transverse fractures usually are stable and can be managed with closed reduction and immobilization. If the fracture is oblique, it may require Kirschner wire fixation because of instability and a propensity for rotational deformity.21
Bennett’s Fracture.: Bennett‘s fracture is an intra-articular fracture at the base of the thumb metacarpal combined with a dislocation or subluxation of the CMC joint. The ulnar portion of the metacarpal remains in place, and the larger fragment subluxates dorsally because of the pulling force of the abductor pollicis longus and adductor pollicis muscles (Fig. 50-40). There is complete disruption of the ligaments around the CMC joint. Because stability is conferred mostly by the dorsal ligament (posterior oblique CMC ligament), dislocation ensues. The mechanism of injury usually involves an axial force acting on a partially flexed metacarpal (e.g., striking a rigid object with a closed fist). This is the most common fracture of the thumb base.32
Bennett’s fracture requires an anatomic reduction. Treatment goals are to achieve stability of the CMC joint by rejoining the volar lip fragment to the first metacarpal and to restore articular congruity. Initial management consists of immobilization in a thumb spica splint, ice, limb elevation, and analgesia. Early referral to a hand surgeon is warranted because although closed reduction can be achieved, the fragments are difficult to hold in position as a result of the pulling forces of the abductor pollicis longus and adductor pollicis muscles. Definitive treatment consists of conservative management, closed reduction with percutaneous pinning, or, if anatomic reduction fails or the fracture fragment represents more than 20% of the articular surface, open reduction and internal fixation.23
Rolando’s Fracture.: Rolando‘s fracture is a comminuted fracture of the base of the thumb metacarpal. Various degrees of comminution occur, but the typical configuration is in a Y– or T-shaped pattern. The severity of comminution often is underrepresented on radiographic studies. The mechanism of injury is the same as in Bennett’s fracture, but Rolando’s fracture occurs much less commonly and generally carries a much worse prognosis.
ED management of Rolando’s fracture consists of immobilization in a thumb spica splint, ice, limb elevation, analgesia, and early referral to a hand surgeon for surgical reduction. Definitive treatment is controversial and depends on the severity of comminution at the base of the thumb and the degree of displacement. If open reduction is indicated, a plate often is placed dorsally to maintain the reconstruction; with severe comminution, Kirschner wire fixation, bone graft placement, and external fixation may be used for continued distraction until healing occurs.33
Complications.: Complications include joint stiffness, degenerative arthritis, and malunion. Malunion is the most common late complication but usually is well tolerated at the thumb CMC joint.34 Post-traumatic arthritis is more common after Rolando’s fracture and may require arthrodesis or resection hemiarthroplasty. Nonunion is rare.
Pediatric Fractures of the Hand
Pathophysiology and Assessment
The hand is frequently injured in children, with phalanx and metacarpal fractures representing the most commonly fractured bones.35 In young children, the most common hand fracture involves a crush injury of the fingertip with an open fracture of the distal tuft.36 The most distinctive feature of the immature skeleton is the presence of epiphyseal growth centers. Although the cartilaginous epiphysis is believed to be a weak link in the immature skeleton, injuries involving this region reportedly account for only 18% of pediatric fractures.37
The Salter-Harris classification of epiphyseal fractures is used to direct treatment and predict outcome. The injuries are classified numerically I through V, with higher numbers corresponding to an increased risk for growth disturbance.38 The proximal phalanx is the most frequently fractured bone among the phalanges.39 The most common epiphyseal fracture in the hand is a Salter-Harris type II fracture of the proximal phalanx.40 It usually results from a twisting or hyperextension mechanism and most often involves the ring and little fingers and the thumb. Although lack of cooperation in this age group may make examination difficult, the clinician should look for swelling, ecchymosis, and deformity. In addition, the examiner should palpate for bony tenderness and for tenderness over the collateral ligaments. Persistent limitation of motion in a young child usually implies a significant injury of the bones or joints of the digit.
Management
Most pediatric hand fractures can be readily treated with either simple splinting or closed reduction, followed by brief immobilization, usually for no longer than 3 weeks. A plaster or fiberglass gutter splint incorporating the adjacent uninjured finger and including the wrist is the best means of immobilizing a child’s finger fracture. The previously mentioned safe position still should be used whenever possible. Some clinicians advocate that in children, even stable injuries that ordinarily would be treated by buddy-splinting in an adult should be protected with full splinting for several weeks to prevent further injury. Open reduction and surgical fixation may be necessary for displaced intra-articular fractures, displaced Salter-Harris type III or IV fractures, and unstable fractures that cannot be maintained by closed methods.41
Soft Tissue Injuries
Soft tissue injuries of the hand are extremely common ED presentations.42 Trauma accounts for most of these injuries to the tendons, ligaments, and cartilage. Although such injuries are not life-threatening, they may result in potentially disabling complications, including deep space infection, osteomyelitis, compartment syndrome, joint laxity, loss of motion, chronic pain, swelling, and deformity.
Dislocations and Ligamentous Injuries
Because the goal of treatment is to restore functional stability, it is essential to perform a systematic evaluation of joint stability. Functionally, stability may be determined through use of a two-phase test of the IP and MCP joints of the hand. Because range of motion is heavily influenced by pain, accurate assessment generally requires digital or wrist block anesthesia in even the most cooperative patients. Active stability is tested by allowing the patient to move the digit through the normal range of motion. Completion of a full range without displacement indicates that adequate joint stability remains. Passive stability is assessed by applying gentle radial and ulnar stress to each collateral ligament and posteroanterior stress to assess volar plate integrity. Stress testing should be done in extended and moderately flexed positions to avoid the stabilizing effect of the volar plate. Comparisons with the same joint of the uninvolved hand may assist in the diagnosis. Supplemental stress radiographs also may be helpful in evaluating difficult cases.43
The diagnosis of incomplete or partial ligamentous injuries is made when the joint is stable to active and passive stress but is significantly swollen, with pain elicited on stress and palpation of the involved ligament systems. The examiner should attempt to ascertain whether the most tender area is over the central slip (dorsal), collateral ligaments (radial and ulnar), or volar plate (volar). Grade I and II injuries exhibit stability with pain on stress testing. Grade III injuries show instability on stress testing. Stability of the joint provides strong evidence that optimal functional recovery would result from short-term immobilization rather than surgical intervention. Because of the three-dimensional boxlike configuration that the collateral ligaments and volar plate form around the joint, wide displacement indicates that at least two components of the ligament box complex are disrupted21,42 (Fig. 50-41). Joints with demonstrable instability should be immobilized in a gutter splint and the patient referred to a hand surgeon to determine whether surgical repair is necessary. Immobilization should be done with the IP joints splinted at 30 degrees of flexion and the MCP joints splinted at 45 to 50 degrees of flexion; when the thumb MCP is involved, it should be splinted in 30 degrees of flexion. Because the long-term effects of joint injuries are almost always joint stiffness and loss of flexion rather than persistent instability, the immobilization period usually is brief (2 to 3 weeks) and should be followed by a gradual procession of active range-of-motion exercises.21
Interphalangeal Joint Injuries
Distal Interphalangeal Joint.: The DIP joint structure is analogous to that of the PIP joint. Additional stability is provided by the adjacent insertions of the flexor and extensor tendons, and dislocations are uncommon. Most dislocations are dorsal and usually are associated with an open wound (Fig. 50-42). The distal phalanx is said to be “bayonet-apposed”—the shafts of distal and middle phalanges lie adjacent to each other, but no bony contact occurs end-to-end at the articular surfaces. Routine radiographs are used more often to rule out associated fractures than to confirm a suspected diagnosis. Treatment consists of closed reduction performed under digital or wrist block anesthesia, followed by active and passive stability testing. Reduction usually is accomplished easily by longitudinal traction and hyperextension to distract the bayonet-apposed distal phalanx followed by direct application of dorsal pressure to the base of the distal phalanx. Irreducible fractures require surgery for open reduction. The irreducibility may be a result of interposition of an avulsed fracture fragment in the joint, entrapment of the profundus tendon, or buttonhole tear through the volar plate.44
If the dislocation is open, the joint is contaminated, and treatment should include débridement and copious wound irrigation. The skin should be sutured and the joint splinted in slight flexion with a dorsal splint for 3 weeks. Most authorities recommend prophylactic antibiotics.44
Proximal Interphalangeal Joint.: Dislocations of the PIP joint are the most common ligament injuries in the hand. Stability is derived from the strong conjoined attachments of the paired collateral ligaments and the volar plate. Three types of displacement of the PIP joint may occur: dorsal, lateral, and volar. The mechanism of injury usually is sports related, with a high-velocity blow to the end of the finger, which causes an axial load and hyperextension. Simple dorsal dislocations result when the volar plate ruptures and the middle phalanx assumes the position of bayonet apposition. Alternatively, a lateral dislocation may result from a radially or ulnarly directed force on the joint that leads to rupture of one collateral ligament and at least partial avulsion of the volar plate from the middle phalanx. In lateral dislocations, the ratio of radial-to-ulnar collateral ligament (UCL) rupture is 6 : 1, and the digit usually is ulnarly deviated. Volar dislocation of the PIP joint is rare. The most common mechanism of injury is a rotary longitudinal compression force on a semiflexed middle phalanx that results in unilateral disruption of a collateral ligament and partial avulsion of the volar plate. Physical examination reveals swelling and tenderness over the PIP joint and inability to extend the joint. Routine radiographs of the injured digit reveal the type of dislocation and any associated avulsion fractures.
Management.: Small bone fragments at attachment sites seen on radiographs are associated with avulsions of minor ligamentous attachment points and do not indicate the need for open repair. Avulsion fractures involving 33% or more of the articular surface usually are unstable and require surgery.45
Most closed dorsal and lateral PIP dislocations are treated nonoperatively.44 Reduction is facilitated by digital nerve block and usually can be accomplished by longitudinal traction and mild hyperextension followed by firm dorsal pressure on the proximal aspect of the middle phalanx. When reduction has been achieved, active motion is tested. Reduction is stable if no displacement occurs during active range of motion and passive stressing of the joint. More than 20 degrees of deformity and instability with lateral testing indicate a complete ligamentous injury.46 If stability is maintained during active range of motion, treatment consists of 3 weeks of immobilization in 20 to 30 degrees of flexion, followed by active exercises. Although stiffness, pain, and swelling are likely to persist for months, the long-term prognosis is good, and subluxation usually does not recur unless the finger is hyperextended again.44 If the dislocation is irreducible or there is evidence of complete ligamentous disruption with dislocation on active range of motion, operative repair is required.
The management of volar dislocations of the PIP joint is controversial. The dislocation has been described as irreducible and requiring open reduction; however, some authorities state that most volar dislocations can be reduced by a closed technique of applying gentle traction with MCP and PIP joints flexed.44 A stable reduction with repair of the soft tissue structures and transarticular pinning in the fully extended position also has been recommended.44
Injury to the Metacarpophalangeal Joints of the Fingers
Pathophysiology.: MCP dislocations are considerably less common than dislocations of the PIP joint. The MCP joints of the fingers are resistant to ligamentous injury and dislocation because of their inherent ligamentous structure, their surrounding supporting structures, and their protected position at the base of the fingers. Like the DIP and PIP joints, each MCP joint has two collateral ligaments and a volar fibrocartilaginous plate; however, the MCP joints are condyloid joints and permit, in addition to flexion and extension, 30 degrees of lateral motion while the joint is extended. Because of the shape of this articulation, the joint is more stable in flexion when the collateral ligaments are stretched than when they are in extension. They are most vulnerable to injury from forces directed ulnarly and dorsally.
Isolated injury to the collateral ligaments and volar plate of the MCP joint is rare. These injuries usually occur with hyperextension stress applied to the MCP joint with the finger extended. The patient has ecchymosis and swelling of the joint. Examination reveals tenderness along the joint and varying degrees of instability. The radiographic appearance usually is normal on routine views, but some clinicians recommend a Brewerton view to show any evidence of avulsed bone fragments.47 Treatment for most of these injuries consists of application of a gentle compression dressing with light plaster reinforcement and early orthopedic referral.
Dislocations of the MCP joints of the fingers are relatively rare injuries and usually are dorsal. The most common digit involved is the index finger, followed by the little finger. These dislocations result from hyperextension forces that rupture the proximal volar plate and are divided into simple and complex types. In the simple dislocation (subluxation), the joint appears to be hyperextended to 60 to 90 degrees, and the articular surfaces are in contact without interposed soft tissue. With complex (complete) dislocations, the MCP joint is in moderate hyperextension and angulated, the metacarpal head is prominent in the palm, and the distended palmar skin is dimpled. Complex dislocations have a less striking presentation but represent a more severe injury; the volar plate is interposed in the MCP joint space, and closed reduction is not possible (Fig. 50-43). Radiographic examination shows an obvious dislocation on the lateral view. Posteroanterior views reveal widening of the joint space in complex dislocations. In addition, sesamoid bones may be seen in the joint; this finding is pathognomonic for this injury (Fig. 50-44).
Management.: After appropriate anesthesia is obtained, simple dorsal dislocations should be reduced in a way that prevents entrapment of the volar plate in the joint. Reduction is accomplished by flexing the wrist to relax the flexor tendons and applying firm pressure over the dorsum of the proximal phalanx in a distal and volar direction. Excessive hyperextension or longitudinal traction should be avoided. The MCP joints should be splinted in flexion, and referral to a hand surgeon is necessary. Complex dorsal dislocations do not reduce with closed methods and require operative reduction. Volar dislocations are rare and generally require operative reduction.
Injury to the Carpometacarpal Joints of the Fingers
Pathophysiology.: The CMC joints of the digit form the base of the transverse metacarpal arch of the hand. The metacarpal bases articulate with one another and with the distal carpal row in a complex interlocking structural arrangement. The joints are supported by strong dorsal, volar, and interosseous ligaments and are reinforced by the broad insertions of the wrist flexors and extensors (Fig. 50-45). Dislocations of the CMC joints are uncommon and often are missed.48 Overall, the most commonly injured CMC joint is the little finger, and most of these injuries are dorsal fracture-dislocations.49 The injury occurs as a result of motor vehicle collisions, falls, crushes, and closed-fist trauma.
Clinical Features and Diagnostic Strategies.: Clinically, the patient has swelling on the dorsum of the hand and tenderness over the involved CMC joints. Routine radiographs should be viewed carefully because fracture lines may be subtle, and the metacarpals may be obscured by superimposition. Other radiographic views that may be helpful include multiple oblique, forearm in 30-degree pronation, and Brewerton views.49
Management.: Initial treatment consists of ice for comfort, limb elevation, and analgesia. Closed reduction of the dorsal fracture-dislocation may be attempted after adequate regional anesthesia has been obtained. Traction and flexion with simultaneous longitudinal pressure on the metacarpal base, followed by extension of the metacarpal head when length has been restored, generally result in reduction. Even in cases in which reduction is achieved by closed means, early referral to a hand surgeon is needed because Kirschner wire fixation is advisable to ensure adequate stability. The late sequelae of fracture-dislocations include pain and weakness from traumatic arthritis secondary to imprecise alignment or chronic dislocation of the CMC joints.
Injury to the Metacarpophalangeal Joint of the Thumb
Management.: Closed reduction may be attempted after radial and median nerve wrist block anesthesia has been achieved. Pressure is directed distally on the base of the proximal phalanx, with the metacarpal flexed and adducted. If reduction is difficult, the IP joint and wrist can be flexed to relax the entrapped flexor pollicis longus tendon. When restoration of anatomic position has been accomplished, the collateral ligaments should be tested, and reduction should be confirmed by radiographic assessment. Stability to active range of motion and stress testing suggests that immobilization in a thumb spica splint with the MCP joint in 20 degrees of flexion for 4 weeks constitutes adequate treatment. Nonreducible (complex) dislocations or dislocations with significant lateral instability require open reduction and operative repair. Hyperextension, instability, and chronic pain on pinching may occur after these injuries.
Ulnar Collateral Ligament Injuries (Gamekeeper’s Thumb, Skier’s Thumb)
Pathophysiology.: Injury to the UCL was first described as an occupational hazard of Scottish gamekeepers, who damaged their thumbs by a repeated maneuver involving twisting the necks of hares.50 Skiing is now the most common cause of acute and chronic injury to the UCL.51 Skier‘s thumb is the most common upper extremity injury in skiing and results from interference with release of the pole at the moment of impact during a fall. UCL rupture occurs 10 times more often than radial collateral ligament injury.52 The mechanism of injury is forced radial deviation (abduction), and the subsequent tear usually occurs at the insertion into the proximal phalanx. Stener53 showed that in nearly two thirds of cases of complete UCL rupture, the adductor pollicis becomes interposed between the superficial proximal portion and the deep distal portion of the ligament (see Fig. 50-45). Besides the collateral ligament injury, associated injuries of the dorsal capsule and volar plate are common.
Clinical Features.: Physical examination reveals swelling and localized tenderness over the ulnar border of the joint and weakness of pinch. Complete and partial ruptures usually can be differentiated by clinical examination. Valgus stress testing of the UCLs is required and should be performed with the joint in full extension and in 30 degrees of flexion to avoid the stabilizing effect of the volar plate. If the examination elicits pain and guarding, the test should be done after median and radial nerve block at the wrist or with use of local infiltration anesthesia. More than 35 degrees of joint laxity or 15 degrees of laxity beyond that present in the uninjured thumb is consistent with complete UCL rupture.54 Routine radiographs should be obtained before the joint is stressed and may reveal a bony avulsion from the insertion of the UCL into the proximal phalanx or an associated condylar fracture. Radiographic findings of proximal phalanx volar subluxation and radial deviation may indicate complete UCL rupture.55 Because of the difficulty in diagnosing complete rupture, it is commonly misdiagnosed as a simple sprain in the ED, potentially resulting in chronic disability.56
Management.: Acute partial ruptures of the UCL can be treated effectively with a 4-week period of immobilization in a thumb spica cast; full recovery is the rule. Complete ligament tears require surgical repair because a high percentage are associated with soft tissue interposition from the adductor aponeurosis (Stener’s lesion), with limited predicted healing potential. Anatomic repair within 3 weeks of injury achieves good or excellent results in 90% of affected patients.57 Long-term complications include chronic pain and instability with the loss of pinch strength, which may necessitate arthrodesis.
Radial Collateral Ligament Injuries
Radial collateral ligament injuries of the MCP joint of the thumb are less common but equally debilitating.52 The usual mechanism is forced adduction with or without hyperextension. Diagnosis and treatment generally are similar to those for UCL injuries. There have been isolated case reports of a Stener-like lesion on the radial side, with some authors advocating for the role of surgical repair.58
Injuries to the Carpometacarpal Joint of the Thumb
Injuries of the volar ligament of the thumb CMC joint, similar to those of other joints of the hand, may be complete or partial. Complete rupture permits the entire thumb metacarpal to dislocate dorsally. Controversy exists regarding the ligament most responsible for stability of the thumb CMC joint, although most recent evidence implicates the dorsoradial ligament in dislocations at this joint.59 These dislocations are reduced easily but are unstable after reduction. Initial management consists of ice, analgesia, limb elevation, and application of a thumb spica splint. The patient should be promptly referred to a hand surgeon for possible operative repair of the ligament. If the capsule is allowed to heal with imperfect metacarpal reduction, joint instability may result, with progressive degenerative changes leading to chronic pain.
Tendon Injuries
Extensor Tendon Injuries
Injuries to the extensor tendons have been grouped into anatomic zones for easy understanding and classification. Different systems for assigning zones have been described, but the most widely accepted is that of Verdan60 (Fig. 50-46). This system defines eight zones, from zone I at the DIP joint level to zone VIII at the distal forearm level. The use of zones is convenient for assessing injury patterns, repair techniques, and rehabilitation.
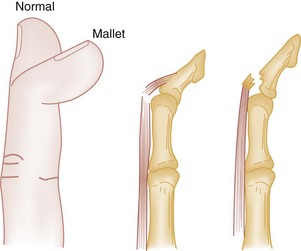
Pathophysiology.: Zone I is the area over the distal phalanx and DIP joint. In this region, the conjoint extensor tendon is well defined and dorsally positioned. Injuries that occur here disrupt the terminal extensor tendon; they may be open or closed and may occur with or without a fracture. Complete laceration of the conjoint tendon results in a flexed posture of approximately 40 degrees at the DIP joint. Partial transection results in a lesser extension lag and a decrease in the strength of extension against resistance from a flexed position. The extension lag may increase if the partial injury is not treated appropriately. For this reason, exploration of dorsal lacerations near the DIP joint is important.
Mallet finger is the most common injury in zone I and refers to a closed disruption of the distal extensor apparatus.21 As a result of loss of extensor tendon continuity to the distal phalanx, there is a flexion deformity of the DIP joint. The injury can be seen in any finger but is most common in the long, ring, and little fingers. Overall, mallet finger represents the most common tendon injury in the hand seen in athletes.61 The mechanism of injury often is sudden forceful flexion of an extended finger when an object, such as a ball, strikes the tip of the finger. This mechanism is commonly encountered in athletes and often is described as “jamming” the finger. Other mechanisms include hyperextension with axial compression and direct crush injury at the DIP joint. Four types of injury patterns are recognized, with type 1 injuries being the most common (Fig. 50-47 and Box 50-2). Fracture fragments of variable size are seen in one fourth to one third of cases (Fig. 50-48). Small avulsion fractures usually are the result of hyperflexion injuries, whereas large fracture fragments usually result from a hyperextension mechanism.62
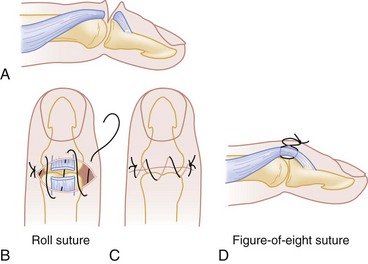
Clinical Features.: In the acute injury, clinical findings include swelling, pain, and tenderness over the DIP joint. The distal phalanx is flexed because of the unopposed action of the FDP. There is usually complete passive but incomplete active extension at the DIP joint. Although the diagnosis is easily made, the patient often seeks treatment late because the functional disability is not great.
Management.: Although various treatment protocols have been proposed, splinting of the IP joint for 6 to 8 weeks has yielded good results while minimizing morbidity in a majority of patients. The primary goal of treatment is the maintenance of continuous DIP joint extension until tendon healing occurs. Treatment of closed (type I) injuries is nonoperative. Immobilization can be accomplished with either a volar or a dorsal splint made from a variety of materials, including aluminum and plastic (Fig. 50-49). The DIP joint is immobilized in slight hyperextension for 6 to 8 weeks, but the PIP and MCP joints are allowed to move freely.21 An excessive degree of hyperextension should be avoided because this can lead to skin necrosis on the dorsal surface of the DIP joint.63
Open zone I injuries that divide the extensor tendon (mallet finger types II and III) are treated by suturing the cut ends (Fig. 50-50). Partial and compete lacerations are repaired with either a roll suture or figure-of-eight stitch with 5-0 nonabsorbable sutures. This repair should be followed by continuous splinting of the DIP joint in full extension for a minimum of 6 weeks.60
Definitive treatment of a type IV injury is controversial. Some authorities recommend operative repair; others recommend conservative management with uninterrupted splinting of the digit.60
Prognosis.: More than 80% of patients who receive conservative treatment for mallet finger report successful outcomes; however, most patients do not regain full mobility at the DIP joint.64 Possible delayed complications include dorsal deformity, cold intolerance, pain, and the so-called swan neck deformity (Fig. 50-51). This abnormality develops when the lateral bands displace proximally and dorsally, resulting in increased extension forces on the PIP joint. Secondarily, the extensor lag at the DIP joint increases because the force of the FDP tendon is unopposed. The swan neck deformity is not seen acutely unless the injured finger has a normally hyperextended PIP joint. Classically, this deformity occurs as a complication of a chronic untreated mallet finger.60

Figure 50-51 Swan neck deformity of the fingers.
Zone II Injuries.: Zone II is the area over the middle phalanx. As the lateral bands blend dorsally to form the conjoint tendon, they are thin and oriented around the dorsal half of the middle phalanx. Injuries here usually are the result of a simple laceration, which seldom transects all of the dorsal apparatus. Examination reveals a typical mallet deformity. The treatment is identical to that for open zone I injuries.
Pathophysiology.: Zone III is the area over the PIP joint. The central tendon is the most commonly injured structure in this zone; such injuries are the second most common closed tendon injury in athletes.61 The mechanisms for closed rupture include forced flexion of an actively extended finger, a direct blow to the dorsum of the PIP joint, and hyperextension with volar dislocation of the PIP joint. It often results from a “jamming” injury. Lacerations that occur just distal to the PIP joint also may divide the central tendon and readily extend into the joint. Wounds are carefully explored to define the status of the PIP joint capsule.
Disruption of the central tendon causes an imbalance in the extensor mechanism. The FDS is now unopposed and flexes the PIP joint. The lateral bands displace volarly to the axis of the PIP joint and become flexors of the joint. In addition, the extensor hood retracts proximally, causing extension of the MCP and DIP joints. The resulting tendon imbalance leads to the so-called boutonnière (buttonhole) deformity, with flexion of the PIP joint and hyperextension of the DIP and MP joints (Fig. 50-52). Although open injuries of the central tendon may cause an acute boutonnière deformity, this usually is delayed several weeks after a closed athletic injury.
Clinical Features.: Early diagnosis of a closed central tendon rupture or avulsion is difficult before the boutonnière deformity has developed. The patient typically has a history of trauma to the involved digit and a painful, swollen PIP joint. The finger is held in slight flexion at the PIP joint and slight extension at the DIP joint. Rupture of the central tendon may be differentiated from the more common injury to the collateral ligament by the location of the maximal area of tenderness on the dorsum rather than on the sides of the joint, and by the patient’s inability to extend the PIP joint actively. PIP joint extension can be tested by having the patient attempt to extend the fingers against slight resistance with the hand flat on the table and the PIP joint flexed 90 degrees over an edge of a table (Elson’s test). A positive Elson’s test result, indicative of rupture of the central tendon slip, occurs when the DIP joint is held in fixed extension or hyperextension, with the absence of PIP joint extension.65 During the acute phase of an injury, a digital block may be necessary to facilitate performance of the Elson test.60 The radiographic appearance of a central tendon rupture typically is normal but may be diagnostic if an avulsion fracture of the volar base of the middle phalanx is visualized on the lateral view.
Management.: Patients with suspected closed central tendon injuries should be managed with splinting of the PIP joint in full extension for 5 to 6 weeks. Only the PIP joint should be immobilized, and passive and active DIP joint flexion is encouraged from the outset. Operative repair may be required for an acute closed boutonnière injury associated with a displaced avulsion fracture and injury with volar PIP joint dislocation. Early referral to a hand surgeon is advised.
Zone IV Injuries.: Zone IV includes the area over the proximal phalanx. The clinical findings are similar to those with zone III injury but are less severe because the PIP joint and lateral bands are intact. The resulting injury usually is partial, and the tendon ends usually do not retract appreciably. These injuries are treated with primary or delayed primary repair and appropriate splinting for 3 to 6 weeks. Simple injuries in this zone can be well approximated with 5-0 nonabsorbable sutures with buried knots. Immobilization should be done with maintenance of the wrist in extension and the MCP joints in approximately 15 degrees of flexion. Tendon adhesions are common in this zone because of associated damage to the periosteum.
Zone V Injuries.: Zone V injuries involve the areas over the MCP joint and should be presumed to be the result of a human bite until proven otherwise. These injuries occur most commonly over the MCP joints of the long and ring fingers. Radiographs are mandatory and may include Brewerton views to assess the metacarpal head closely for injury. The clinical findings with injuries to the extensor tendon at this level are flexion of the MCP joint and inability to extend the joint fully.
In an open joint injury caused by a human bite, the potential for mixed aerobic and anaerobic infections is high. Operative exploration, débridement, and irrigation are necessary. A combination of a β-lactam and a β-lactamase inhibitor drug is recommended empirically for infections related to human bites.28 In penicillin-allergic patients, clindamycin in combination with a fluoroquinolone may be given.28 The wound is left open and may be closed at 4 to 5 days if free from infection. The resultant tendon injury usually is only a partial laceration, which may be managed with primary or delayed primary repair.
Zone VI Injuries.: Zone VI includes the area of the dorsum of the hand. Although these injuries may be similar in clinical appearance to zone V injuries, the joint is not involved, and these injuries generally are not as severe. Because the extensor tendons are superficial at this level, a relatively trivial-appearing skin laceration may be associated with one or more tendon lacerations. If the injury is proximal to the juncturae tendinum, the patient may be able to extend the involved MCP joint because weak extensor forces are transmitted to the junctura from adjacent extensor tendons.
Flexor Tendon Injuries
Pathophysiology.: Flexor tendon injuries are not as common as injuries to the extensor complex and often have a subtle clinical presentation. The most common mechanism of injury is laceration, but closed traumatic disruption also may occur. FDP avulsion is the third most common tendon rupture in the hand in athletes.61 This injury usually is sports-related and involves a hyperextension force applied to an actively flexing digit; the classic example is that of an injured digit in a football player who grabs the clothing of an opponent who is breaking free from a tackle. Most of these injuries involve the ring finger, possibly because the ring finger becomes the most prominent finger with the fingers held in a partially flexed position.66 Because of the closed nature of these injuries, the patient may not seek immediate care, or the condition initially may be misdiagnosed.
Clinical Features.: Careful assessment is necessary to diagnose flexor tendon disruption and associated neurovascular injury. With the normal hand at rest, there is a cascade of flexion of the digits, beginning with less flexion at the index finger and progressing to more flexion toward the little finger. An injury to a flexor tendon may be evident if the involved finger does not assume a naturally flexed position. Complete disruption of the profundus tendon results in an extended position of the DIP joint as a result of unopposed extensor forces. If the FDS is completely severed, or a partial tendon injury has occurred, the digit rests in less flexion than normal. An abnormal posture of the injured digit may suggest a flexor tendon injury; this usually is confirmed by a functional examination. The FDP and the FDS should be tested separately as previously described. This examination requires careful observation: The patient may flex the distal tip with an intact profundus, but an injury to the FDS precludes flexion at the PIP joint. Disruption of the FDP tendon leads to loss of flexion at the DIP joint, instability in pinch, and loss of grip strength. FDP avulsions can be classified into three types. Type I injuries involve retraction of the avulsed FDP tendon into the palm, damaging the blood supply to the tendon and causing hematoma formation in the process. Because of the damaged vasculature, these injuries should be repaired urgently to prevent ischemic tendon damage.67 Types II and III injuries cause lesser degrees of retraction of the FDP tendon. Accordingly, these injuries result in less compromise of the tendon’s blood supply and have more favorable outcomes.67 FDP injuries may be present if the patient complains of subjective weakness or if an abnormal position of the hand is observed at rest. Clinically, injuries are associated with pain and weakness with flexion against resistance. Despite these findings, it may not be possible to arrive at a complete and accurate diagnosis until the wound is surgically explored. The palmaris longus, which is not present in approximately 15% of people, is not a functionally significant wrist flexor. Palmaris longus lacerations have tremendous diagnostic significance, however, because most of these injuries (80 to 90%) are associated with concomitant partial or complete median nerve lacerations. For this reason, all patients with palmaris longus lacerations should be assumed to have median nerve laceration until such injury has been ruled out clinically or by direct examination.68
Management.: Flexor tendon repairs require the expertise of a hand surgeon and generally are not repaired by emergency physicians. Immediate or delayed primary repair is now advocated for most acute flexor tendon injuries, including avulsions of the FDP and injuries involving the so-called “no man’s land,” which extends from the distal palmar crease to the midportion of the middle phalanx. The term “no man’s land” refers to the high frequency of tendon adhesion after injury in this area. The advantages of primary repair with surgical reapproximation over secondary grafting for treatment of acute injuries have been well described in the literature.69 Emergent repair of lacerated flexor tendons is indicated in the setting of diminished circulation to the digit requiring vascular repair. Otherwise, early definitive repair can be undertaken within days of the injury.69 Secondary repair of flexor tendons may be performed 4 weeks after injury, but repair is considered late after that. In general, the results of primary, delayed primary, and early secondary repair are approximately equal. Treatment of partial flexor tendon lacerations is controversial, but referral to a hand surgeon for further exploration and possible repair is prudent.
Complications.: With optimal management, most patients with flexor tendon injuries have good to excellent outcomes.70 With injuries involving the no man’s land, results may be poor, and tendon grafting occasionally is required. Overall, adhesions remain the most significant problem after operative repair. Other complications include triggering, bowstringing, and intratendinous epidermoid cyst formation.71
Mutilating Injuries
Mutilating injuries to the hand are encountered frequently in the ED. These are severe multistructural injuries that destroy the anatomy and functional integrity of the hand. Initial evaluation should focus on preservation of vital structures, analgesics, early consultation, wound care with débridement of devitalized tissue, and antibiotics. Evolving over recent years is a more aggressive push with respect to procedure timing, whether a single-stage or multistage strategy is used.72 Successful long-term clinical and socioeconomic outcomes have brought focused attention on procedure timing. The concept of early primary reconstruction with fast rehabilitation should be pursued based on case profile.72 One such type is snowblower-, wood chipper–, or lawnmower-associated hand injuries, which can result in substantial deformity and disability. Snowblower injuries typically occur in clusters and are responsible for approximately 1000 amputations and 5000 ED visits annually.73 The dominant hand is involved approximately 68% of the time, with middle and index fingers most commonly injured. Phalangeal fractures are the most common type of injury.74 Snowblower injuries often are managed as open fractures with intravenous antibiotics, irrigation, and débridement and repair of bone, soft tissue, and nail bed structures.74 Irreparable devascularization currently is considered the only absolute indication for immediate or early digital amputation after injury.75 The concept and techniques for reimplantation and revascularization in mutilating injuries in children are similar to those in adults.76
Fingertip Injuries
Fingertip Amputations
Classification.: Fingertip amputations are the most common type of amputation of the upper extremity. In zone I injuries (Fig. 50-53), the proximal two thirds of the nail bed is preserved. In zone II injuries, bone is exposed, and in zone III injuries, the entire nail bed is lost. Radiographic studies are indicated if bony avulsion injury or fracture cannot be excluded. Most of these fingertip injuries can be managed on an outpatient basis.
Management.: Treatment of distal fingertip injuries is controversial; consequently, management should be individualized, and few guidelines are available. In general, most hand surgeons try to maintain length of the thumb by whatever means possible.77 The index finger is considered next before the other fingers. An intact pulp-to-pulp pinch mechanism is the principal goal. Other factors to consider include the patient’s age, health, occupation, and handedness.
Complications.: These injuries commonly leave the patient with a painful, cold-intolerant fingertip; this complication has been described after primary closure, coverage with grafts or flaps, and healing by secondary intention. Skin grafting may result in induration, fissuring, and diminished sensibility. Nail deformity is common, particularly with considerable volar loss of tissue.78
Acute Nail Bed Injuries
Injuries of the nail bed most commonly result from localized trauma to the nail with subsequent compression of the nail bed. The most common type of injury is simple laceration followed by stellate laceration, crush, and avulsion.79 The middle and distal thirds of the nail bed are the most common sites of injury, and 50% of these injuries involve fractures of the distal phalanx or tuft.79 Radiographs are required in most cases to show occult fractures and foreign bodies.
Subungual Hematoma.: Subungual hematomas result from crush injury or blunt trauma to the nail bed with bleeding from the rich vascular bed. The nail bed is predisposed to injury because it is interposed between the firm nail and the distal phalanx. The injury is manifested by pain and dark red to black discoloration of the nail bed and is classified by the percentage of area beneath the nail that is involved. When the fingertip is unstable or the mechanism of injury suggests a significant distal phalanx fracture, a radiograph should be obtained to identify associated fracture.
Management.: Small subungual hematomas do not require drainage; the blood is incorporated into the nail and eventually removed with the free edge. Large (>50% of the nail) hematomas cause significant discomfort and should be removed by nail trephination with a heated paper clip or a hot microcautery unit. Some clinicians recommend a surgical scrub of the finger before perforation of the nail to prevent contamination of the subungual area and the subsequent risk of infection and potential osteomyelitis, but this generally is unnecessary. Anesthesia is not necessary, and pain relief is immediate with decompression. If a significant fracture is present, the digit should be splinted. Although a distal phalangeal fracture with a subungual hematoma is technically an open fracture, such injuries usually heal without problems. Ungual tuft fractures are not associated with osteomyelitis. The risk of infection with an open fracture of the phalanx proper should be considered, and a broad-spectrum antibiotic and close follow-up monitoring are recommended. Otherwise, antibiotics are not necessary. Patients with significant hematomas should be informed that they may lose the nail.
Some authorities recommend nail removal and nail bed repair if the size of the subungual hematoma is greater than 50% of the nail area. Simon and Wolgin80 attempted to correlate the association between subungual hematoma size, digital phalanx fractures, and occult nail bed lacerations. In their series, patients with a subungual hematoma greater than half the size of the nail had a 60% incidence of nail bed laceration requiring repair, and if an associated fracture of the distal phalanx was present, the incidence was 95%. If more than 50% of the visible portion of the nail is undermined by hematoma, some clinicians recommend removal of the nail, inspection of the nail bed, and repair of injuries. However, several studies have found no notable differences in outcome between nail trephination alone and formal nail bed repair regardless of hematoma size in cases with an intact nail and nail margins.81–83 As a result, many authorities now recommend nail removal and repair of the nail bed only if the nail is broken or the nail edges are disrupted.79
Nail Bed Lacerations.: Lacerations of the nail bed should be repaired to minimize esthetic deformity and the duration of functional impairment. These injuries generally do well after primary repair, but late reconstruction of the nail bed is unpredictable, and usually little improvement is obtained.
Simple and crushing lacerations should be repaired accurately with 5-0 or 6-0 absorbable suture, ideally under loupe magnification. The results with both injuries should be satisfactory in the majority of cases.79 After the nail bed is accurately approximated, a hole is burned through the nail to allow drainage of blood from the subungual area after the nail is reinserted into the nail fold. The avulsed nail may be sutured in place or secured with tape. A single thickness of nail-shaped Adaptic or other nonadherent gauze may be placed in the nail fold if the nail is unavailable. The replaced nail or gauze is used as a temporary splint to help protect the integrity of the underlying nail bed and maintain the fold for new nail growth and to help prevent synechiae and subsequent nail deformity. Complete nail growth takes 70 to 160 days, but after the injury the growth pattern often is changed.
Nail bed avulsion commonly leaves fragments of nail bed attached to the undersurface of the avulsed nail.84 In these cases it is advisable to replace the nail as accurately as possible onto the avulsion site. Repair should be done with mattress sutures without attempting to separate the nail from the nail bed. If the tissue is not available and the defect is small, effective healing occurs by secondary intention.
Clenched-Fist Injuries
All human bites should be considered serious in nature and at risk for significant complications. Clenched-fist injuries, also called “fight bites,” are notorious for being the worst human bites. Inadequate initial management leads to significant morbidity. Misleading history, innocuous wound appearance, intoxication and lack of cooperation of the patient leading to inadequate examination, patient reluctance to admit the nature of the injury, delayed presentation, and inadequate exploration all may lead to mismanagement. Clenched-fist injuries are associated with the highest incidence of complications of any closed-fist injury and of any type of bite wound.85
Clinical Features
The classic injury is a bite wound over the third MCP joint, but injury can occur over any joint. Soft tissue injury is apparent with possible extensor tendon injury and violation of the joint capsule. When the fist is subsequently opened, the bacterial inoculum is dragged with the extensor tendon and soft tissue proximally into the dorsum of the hand.85 Presentation may be acute or delayed. Swelling, limited range of motion, erythema, and pain out of proportion to the apparent severity of injury are typical findings. Pain is more severe with range of motion.
High-Pressure Injection Injuries
High-pressure injection injuries to the hand are uncommon, and most are occupation related. The usual cause is an accident involving industrial equipment, with machinery such as grease guns, spray guns, and diesel engine injectors accounting for most of these injuries.86 A wide variety of materials, including paint, paint thinner, grease, oil, hydraulic fluid, plastic, wax, water, and semifluid cement, have been reported to be injected. In general, substances that are highly viscous (e.g., grease) require higher forces to produce injury than do paint, oil, and solvents. The high pressures involved are sufficient to penetrate skin from a distance, and contact of the device with the hand is not a prerequisite for injury to occur. High-pressure injection injuries have been associated with amputation rates as high as 48%.87 Recent data suggest amputation rates of 30%, which may be a result of higher vigilance and early recognition of tissue injury.88 Early recognition and intervention are essential. Even with early intervention, the injury leads to significant impairment, with delays in débridement associated with higher rates of amputation.87
Pathophysiology
Tissue injury from high-pressure injection generally depends on physical, chemical, and biologic factors. Of particular importance are the type, amount, and velocity of injected material and the anatomic location of the injury. The most important factor is the type of material injected, which determines the likely tissue inflammatory response and the resulting fibrosis that develops during healing. Paint and paint thinner produce a large, early inflammatory response, resulting in a high percentage of amputations.89 By contrast, grease injuries cause a small inflammatory response and carry a lower amputation rate but are associated with oleogranuloma and fistula formation, scarring, and loss of digit function.89 The amount of material injected into the confined space of the digits or palm determines the degree of mechanical distention and the potential for vascular compromise. The velocity of the injected material and the site of tissue penetration determine dispersion, which may include the digit, hand, and forearm. Injection injuries at distal sites (e.g., tips of fingers) carry a worse prognosis than proximal injections.87
Complications
Early recognition and treatment, including operative decompression and débridement, greatly influence outcome. Early surgical amputation should be considered in cases in which the affected digit is initially cool or poorly perfused.90 In most other cases, joint stiffness is a late sequela.
Amputations and Ring Avulsion Injuries
Few epidemiologic studies have been done on amputation injuries. Traumatic amputations have been reported to constitute 0.1 to 1% of all hand injuries.2 Amputation may be complete or partial. Injuries with interconnecting tissue between the distal and the proximal portions are considered incomplete, or partial, amputations. Complete amputations will necessitate replantation, whereas with partial amputations, revascularization is attempted. Traumatic amputations most commonly result from local crush injuries and occur infrequently from a sharp guillotine mechanism. Partial and complete amputations reportedly occur with equal frequency. The former are often related to the use of power saws and lawnmowers.
Ring avulsions include a spectrum of injuries from partial degloving of the skin of a finger to loss of the entire digit and entire length of a flexor tendon. These injuries usually occur when a ring on a finger catches on an object during a fall. In addition to neurologic and arterial injuries, there may be complete disruption of the venous return of the finger. In general, these injuries represent complex management problems, and treatment may range from primary amputation to microvascular repair with replantation and free tissue transfer in addition to local flap, pedicle flap, or graft coverage.91
The time for which an amputated part can survive before replantation has not been determined. As a general rule, the more proximal the amputation, the less ischemia time the amputated part can tolerate. Attempts to extend viability during ischemia have shown that the most important controllable factor is the temperature of the amputated part. Warm ischemia may be tolerated for 6 to 8 hours; cooling the part to 4° C extends this time to approximately 12 to 24 hours with distal amputations. Successful replantation of digits after 40 hours of warm ischemia has been reported.92
The decision of whether to attempt replantation should be made by the surgeon who is responsible for performing the procedure. On occasion, final judgment regarding replantation may be delayed until after microscopic inspection of vessels and nerves has been completed.93 Patient selection generally is based on the nature and level of the injury and patient age and health-related factors. The classic indications for and contraindications to replantation are listed in Box 50-3. The thumb is needed to preserve the function of opposition, and all such traumatic amputations should be considered for microvascular salvage regardless of the level of amputation or mechanism of injury. Loss of the thumb is equivalent to a 40% loss of function of the hand.94 Similarly, all amputations in children should be considered for replantation. In replantation of digits amputated distal to the insertion of the FDS between the PIP joint and the DIP joint, good motor and sensory function often is achieved. If the amputated part is crushed, mangled, or amputated at multiple levels, however, replantation usually is contraindicated. With digits that cannot be replanted, skin coverage by flaps or ray resection will be required.
Vascular Injuries
Significant vascular disorders of the hand are uncommon compared with other problems of the hand. The vascular supply to the hand and digits is duplicated so that isolated arterial injuries to either side seldom result in ischemia. Lacerations of the arteries of the hand may stop bleeding by the time the patient is evaluated; in these situations, a history of pulsatile bleeding is highly suggestive of an arterial injury. Although most arterial injuries are the result of penetrating trauma, blunt trauma to the hand occasionally can result in arterial thrombosis or a false aneurysm.13 In addition, associated injuries should not be overlooked. Because digital nerves invariably cross with and are superficial to the digital artery, an arterial lesion should raise the possibility of an accompanying nerve injury.
Compartment Syndrome in the Hand
A compartment syndrome develops when elevated pressure within a closed fascial space reduces perfusion to the point of muscle and nerve dysfunction. In the hand, 10 compartments are evident on cross section through the palm (Fig. 50-54). In addition, the fingers are compartmentalized by fascia and skin at flexor creases. Because these compartments are not interconnected, each additional compartment should be surgically decompressed if muscle ischemia is suspected.13,95
Nerve Injuries
Nerve injuries may result from a direct blow, puncture or laceration, crush injury, injection injury, or amputation. These injuries are divided into three main groups: neurapraxia, axonotmesis, and neurotmesis. In neurapraxia, there is loss of function of the nerve, but the axon, Schwann’s sheath, and endoneurium remain intact. Recovery in these cases is usually complete within days. In axonotmesis, the axon is severed within an intact endoneurial tube. The distal axon degenerates and is absorbed after disruption. The proximal portion of the severed axonal stump can regenerate along the intact endoneurial tube at a rate of approximately 1 to 3 mm/day with ultimate return of function. Neurotmesis refers to complete disruption of all nerve elements. Regrowth of the proximal axonal endings does not occur along the endoneurial tubes, unless the severed nerve endings are reapproximated.96
Management
Identification of the injury and appropriate referral are important aspects in the initial management of patients with nerve injuries in the hand. Patients with closed nerve injuries not associated with compartment syndromes should be referred to a hand specialist for serial examinations. All digits that have lost function as a result of a nerve injury should be splinted to prevent further inadvertent injury. If function does not return within 3 weeks, electromyograms and nerve conduction studies can help differentiate neurotmesis from axonotmesis and determine the need for surgical exploration.96
Lacerated nerves require reapproximation by hand surgeons. In general, all motor branches of the ulnar and median nerves should be repaired. In addition, digital nerve injuries proximal to the DIP crease on the radial aspect of the index finger, the ulnar aspect of the little finger, and both sides of the thumb should be considered for repair.97 Clean, single-nerve lacerations should be repaired primarily when feasible. Complex nerve injuries may involve wound contamination or extensive tissue damage and usually are managed by delayed repair to allow for improved soft tissue conditions. Although the functional recovery is never complete, a good outcome can result from primary and delayed repair. In general, sensory recovery returns more often than does motor function.
Infections of the Hand
Paronychia
Pathophysiology.: A paronychia is a localized superficial infection or abscess involving the lateral nail fold. It is the most common infection in the hand and is thought to be caused by frequent trauma to the delicate skin around the fingernail and cuticle. Clinically, swelling and tenderness of the soft tissue along one or both sides of the lateral nail fold are evident. A paronychia begins as a cellulitis, but a frank abscess may form, and occasional extension to the overlying proximal nail (termed an eponychia) may be seen. S. aureus is the most common isolate, followed by streptococci.98 Paronychias in children often are caused by anaerobes, presumably because of finger sucking and nail biting common in this age group.99 Atypical mycobacteria, Candida albicans, and other fungi should be considered as causative agents in chronic cases unresponsive to standard treatment.100
Management.: In the early cellulitis phase, management consists of frequent warm soaks, elevation of the affected limb, and administration of an oral antistaphylococcal antibiotic, such as dicloxacillin or cephalexin. When the area becomes fluctuant, drainage is necessary and usually is curative. Adequate drainage often can be obtained by lifting the skin edge off the nail to allow the pus to drain (Fig. 50-55). This can be accomplished without anesthesia in selected patients, but drainage for more extensive lesions is best carried out under digital block anesthesia. After the eponychium has been softened by soaking, a No. 11 blade scalpel or an 18-gauge needle may be advanced parallel to the nail and under the eponychium at the site of maximal swelling.98 If the infection is more extensive, the lateral one fourth of the nail may be bluntly dissected from the underlying nail bed and germinal matrix, and the lateral nail plate excised. After the cavity is irrigated, a small piece of packing gauze may be slipped under the eponychium for 24 hours to provide continual drainage. Cultures are not indicated. Antibiotics are commonly prescribed, although this is not necessary if drainage is complete or if the surrounding area of cellulitis is minimal. Most paronychias resolve in 5 to 10 days, and patients are advised to obtain primary care follow-up evaluation. A well-known complication of even a properly drained paronychia is osteomyelitis of the distal phalanx. Patients with a chronic, indolent infection of the perionychium seldom respond to ED intervention. These patients should be referred to a dermatologist or hand surgeon because of the prolonged treatment required.
Felon
Pathophysiology.: A felon is an infection of the pulp of the distal finger or thumb. It differs from other types of subcutaneous abscesses because of the presence of multiple vertical septa that divide the pulp into small fascial compartments. The usual cause is penetrating trauma with secondary bacterial invasion. The most common pathogen is S. aureus, although gram-negative organisms and polymicrobial infections also have been described.100 Although the septa may facilitate an infection in the pulp and inhibit drainage after incomplete surgical decompression, they provide a barrier that protects the joint space and the tendon sheath by limiting the proximal spread of infection. Clinically, a felon begins as an area of cellulitis and inflammation that progresses rapidly to severe throbbing, pain, swelling, and increased pressure in the distal pulp space.
Management.: Traditional management of felons emphasizes the need for early and complete incision through the septa to provide adequate drainage and to relieve pressure in septal compartments. Most felons can be drained by a single lateral incision.100 The incision should be made along the ulnar aspect of the index, middle, and ring fingers and the radial aspects of the thumb and little finger, avoiding pincher surfaces. The incision is begun approximately 0.5 cm distal to the DIP joint crease and dorsal to the neurovascular bundle of the fingertip. The incision is extended to the free edge of the nail (Fig. 50-56). The wound should be irrigated and loosely packed with gauze, and the affected finger splinted. The packing is removed in 48 to 72 hours, and the wound is left to close secondarily. Most felons are treated empirically with an antistaphylococcal oral antibiotic for at least 5 days pending culture results. Some authorities recommend draining this abscess where it “points,” with use of a volar midline incision that does not cross the distal flexion crease.101
Complications.: If untreated, the expanding abscess can extend toward the phalanx, producing an osteitis or osteomyelitis, or toward the skin, resulting in necrosis and formation of a sinus tract on the palmar surface of the digital pulp. Other complications include soft tissue and bony tuft necrosis, osteomyelitis, septic arthritis of the DIP joint, and flexor tenosynovitis from proximal extension. The lateral incision used to drain felons commonly leaves unstable finger pads or may result in painful neuromas or anesthetic fingertips. “Fishmouth” incisions may destroy the blood supply to the fingertip.100 Longitudinal midline incisions on the volar surface may leave scars over an important area for sensation but do not have the other disadvantages of lateral incisions. Any incision that is made too deeply and proximally can injure the flexor tendon sheath, initiating a tenosynovitis.
Herpetic Whitlow
Epidemiology and Pathophysiology.: Herpetic whitlow is a self-limited herpes simplex viral infection of the distal finger. It is the most common viral infection of the hand. Infection by human herpes simplex virus type 1 or 2 is clinically indistinguishable.102 Direct inoculation of the virus into an open wound or broken skin is the usual mechanism of primary infection. Herpetic whitlow commonly is reported in adult women with genital herpes and children with coexistent herpetic gingivostomatitis. Health care workers are at increased risk for development of this infection as an occupational hazard secondary to exposure to orotracheal secretions; however, a review of herpes infection in the hand found that only 14% of adult cases occur in health care workers.103 The overall incidence has decreased, probably as a result of heightened awareness of the condition and strict infection control precautions.
Clinical Features.: The infection usually involves a single finger and begins with localized pain, pruritus, and swelling, followed by the appearance of clear vesicles. Systemic symptoms usually are absent; however, secondary infection of the vesicles can occur.102 More typically, the vesicles coalesce over 2 weeks to form an ulcer, which may develop a hemorrhagic base. At this stage, it may be difficult to distinguish herpes simplex infection of the hand from more common bacterial infections, such as felon or paronychia. The distinction is important because drainage of the herpetic lesions is contraindicated and may lead to viral dissemination and secondary bacterial infection. A careful history is important to determine risk of a possible herpetic cause. On examination, tenderness is present but is noticeably less than that typical for bacterial infections. In addition, the pulp space remains soft and does not become tense, as it does in a bacterial felon.104
Diagnostic Strategies.: The diagnosis usually is made clinically on the basis of the appearance of the lesion and the history of recurrence or potential sources of inoculation. The diagnosis may be confirmed by polymerase chain reaction (PCR), viral culture, or a Tzanck smear showing multinucleated giant cells in a scraping taken from the base of an unroofed vesicle.102,105
Management.: Herpetic whitlow usually resolves spontaneously in 3 to 4 weeks, although recurrence is common, occurring in up to 20% of cases. The main goals of treatment are to prevent oral inoculation or transmission of the infection and to provide symptomatic relief. The involved digit should be kept covered with a dry dressing. Oral acyclovir has a role in treatment for immunocompromised patients and patients with frequently recurring infections, but its role in immunocompetent patients is less clear.105 Topical acyclovir has not been shown to be effective in either the treatment of or the prophylaxis for this disorder.
Tenosynovitis
Pathophysiology.: Acute synovial space infections in the hand usually involve the flexor tendon sheaths and the radial and ulnar bursae. The tendon sheaths are double-walled, with a visceral layer adherent to the tendon and a parietal layer extending from the midpalmar crease to just proximal to the DIP joint. The flexor tendon sheath of the thumb is continuous with the radial bursa of the palm, and the small finger sheath is continuous with the ulnar palmar bursae. The ulnar bursa surrounds the superficial and deep flexor tendons, and the radial bursa surrounds the flexor pollicis longus. These two bursae communicate in 80% of persons; in most instances, however, the tenosynovial coverings of the index, middle, and ring fingers do not communicate. Infections in the synovial spaces in the hand tend to spread along the course of the flexor tendon sheaths and may spread to the midpalmar, thenar, and lumbrical compartments. Infections usually are caused by penetrating trauma to the sheath, but they occasionally result from hematogenous spread. The most commonly isolated organisms are S. aureus and streptococci, followed by gram-negative organisms and enterococci.106
Clinical Features.: Four cardinal signs of acute flexor tenosynovitis usually are present and help differentiate tenosynovitis from other soft tissue infections in the hand: (1) tenderness along the course of the flexor tendon, (2) symmetrical swelling of the finger, (3) pain on passive extension, and (4) a flexed posture of the finger.60 All four signs may not be present early in the course of infection. The third sign may be the most important. Early recognition and treatment are essential because elevated pressure within the enclosure of the flexor tendon sheath can occlude the already tenuous circulation to the tendon, resulting in necrosis and proximal spread.
Management.: All patients with flexor tenosynovitis require hospital admission and prompt consultation with a hand surgeon to determine whether open drainage or closed tendon sheath irrigation is indicated. In early cases or uncertain diagnoses, the hand should be splinted in a bulky dressing and elevated, and intravenous antibiotics should be initiated. Infections secondary to penetrating trauma should be treated with a penicillinase-resistant antistaphylococcal penicillin or first-generation cephalosporin. Disseminated gonorrhea should be considered in all sexually active persons, especially if a traumatic cause for the infection is not apparent. In such cases, some authorities recommend empirical treatment with ceftriaxone until results of final cultures (including mucosal sites) are available.106,107 Surgical treatment is indicated for established cases or when improvement is not evident within 24 hours.
Deep Space Infections
Anatomy and Pathophysiology.: The deep fascial or palmar spaces of the hand include the midpalmar space, the hypothenar space, and the thenar space. Three additional, more superficial spaces of the hand are the dorsal subcutaneous space, the dorsal subaponeurotic space, and the interdigital web space108 (Fig. 50-57). Although anatomically distinct from the deep spaces owing to their lack of well-defined anatomic borders, superficial spaces can harbor infections that manifest similarly to deep space infections.108 The fascial spaces are potential rather than actual spaces in a normal hand.109 These closed compartments are susceptible to infection from direct penetrating trauma, infection in contiguous compartments, or hematogenous seeding. The most commonly isolated pathogens are S. aureus, streptococci, and coliforms.
Clinical Features.: The unique anatomic features of the deep fascial spaces lead to characteristic clinical findings when these regions are involved with pyogenic infection. The dorsal subaponeurotic abscess causes swelling and erythema on the dorsum of the hand. Pain with passive movement of the extensor tendons often is present, but it may be difficult to distinguish clinically from simple cellulitis on the dorsum of the hand. Subfascial web space infections commonly result when palmar blisters become secondarily infected. The infection tends to spread dorsally into the interdigital space and produce a characteristic hourglass configuration, or the so-called “collar-button abscess” (Fig. 50-58). Thenar space infections are characterized by pain and swelling of the thenar eminence and the first web space; the thumb is held in abducted and flexed position.109 In midpalmar infections, clinical features include loss of the normal hand concavity and tenderness of the central palm; movement of the middle and ring fingers is painful. Suppurative tenosynovitis of the second digit can rupture proximally into the thenar space, with subsequent abscess formation. Tenosynovitis of digits III, IV, and V may be responsible for a midpalmar space infection.
Management.: Treatment of all deep fascial space infections involves intravenous antibiotics and operative exploration and drainage by experienced surgeons. The most common practice is to use broad-spectrum empirical coverage with a β-lactamase–resistant penicillin or a first-generation cephalosporin. Based on local bacteriologic data, it may be necessary to begin empirical coverage against methicillin-resistant S. aureus (MRSA).110
Septic Arthritis
Pathophysiology.: Septic arthritis in the hand may involve the IP, MCP, CMC, or radiocarpal joints. These joints usually are infected by direct inoculation of bacteria from penetrating trauma or by spread from a contiguous infective process, such as a felon or tenosynovitis. Hematogenous spread may occur but is less common than in other joints of the body. S. aureus is the most common cause; streptococci, Haemophilus influenzae, Pseudomonas aeruginosa, and coliforms are involved much less commonly.111 A survey at a large county hospital found that the most commonly isolated organisms were staphylococci and streptococci in nearly equal numbers, with enterococci, corynebacteria, and anaerobes encountered rarely.112 Monarticular nontraumatic septic arthritis also may be caused by Neisseria gonorrhoeae.
Clinical Features.: Clinically the involved joint appears red and swollen and is extremely tender; an overlying puncture wound may be visible. The joint is held in a position that maximizes its volume (slight flexion for MCP and IP joints), and passive motion of the joint, however slight, is painful. In contrast with flexor tenosynovitis, tenderness is localized to the involved joint.108 Pain also may be elicited by axial compression of the joint. The diagnosis is made by arthrocentesis.
Management.: Treatment includes parenteral antibiotics with a semisynthetic antistaphylococcal penicillin and emergent drainage of the joint. Most infected joints require open drainage, but some hand surgeons may choose to manage certain cases with closed joint catheter irrigation and repeated aspiration.
Osteomyelitis
Osteomyelitis in the hand occurs most commonly with open fractures or with secondary involvement of bone from soft tissue infections. The incidence of infection in open fractures of the hand is much lower than in open long bone fractures and is reported to be 1 to 11%. McLain and colleagues30 found that injuries with severe skeletal trauma, gross contamination, and significant soft tissue injury have the highest risks for infection. The presentation of osteomyelitis is seldom rapid and fulminant, unless associated with septic arthritis or other deep space infection of the hand. Physical signs may include fever, localized redness, swelling, warmth, and tenderness. Children with osteomyelitis may have pseudoparalysis, manifesting as refusal to use the affected limb.114 Radiographs may show bone destruction or periosteal elevation. Treatment includes débridement of infected bone and sequestra and parenteral antibiotics.
Nontraumatic Disorders of the Hand
The most common type of stenosing tenosynovitis in the hand involves the flexor tendons at the level of the MCP joint where the tendon passes through the pulley systems. Repetitive strain can result in tendon and pulley hypertrophy with localized tenderness. When painful blocking of flexion and extension is noted at the involved joint, the condition is called trigger finger, as noted earlier. The ring and long fingers are the most commonly involved digits. Injection therapy is recommended and works well in most patients.115 A mixture of 1% lidocaine and steroid suspension (for a total volume of 0.5-1 mL) is given over the nodule and into the tendon sheath.116,117 After the injection, extension of the finger usually is possible. The finger should be splinted in extension, and referral to a hand surgeon is advised because multiple injections or surgical release may be required.118
Ganglion
A ganglion is the most common soft tissue tumor of the hand and consists of a synovial cyst from either a joint or the synovial lining of a tendon that has herniated. Ganglia contain a gelatinous fluid that is secreted by the synovial tissue. They are common in the wrist and the flexor tendon sheaths of the fingers and usually have an insidious onset. Patients rarely recall a specific inciting traumatic event.119 Patients commonly complain of a dull ache or mild pain over the ganglion. Reassurance is important, and the patient should be informed of the benign nature of the lesion. A large or troublesome ganglion can be aspirated. Because of the high rate of recurrence, definitive treatment is operative excision, which is done on an elective basis.119
Foreign Bodies in the Hand
Penetrating trauma to the hand may result in a foreign body becoming lodged in the soft tissues. The presence of a foreign body should be considered in any wound regardless of its size. A detailed and accurate history of the injury should be obtained because the mechanism often gives clues to the possibility of a foreign body.120 The most common foreign bodies are pieces of wood, glass, or metal. Useful signs of occult foreign bodies include sharp pain with deep palpation over a puncture wound, pain associated with a mass, and failure of a wound to heal or persistence of pain with movement.19
Initial examination of hand wounds should include local exploration with sterile technique in a bloodless field. After exploration and removal of easily accessible foreign bodies, radiographs should be taken using soft tissue technique with multiple views. Radiographs are the best method for detecting radiopaque foreign bodies and detect metals, most glass, many plastics, gravel, and sand.19 Wooden foreign bodies are difficult to visualize radiographically.121 Whether an object shows on plain radiographs depends on its composition, configuration, size, and orientation. When a foreign body is clinically suspected and the initial radiographic appearance is normal, other imaging methods should be considered. The identification of nonmetallic objects such as splinters may be improved by the use of modalities including computed tomography, magnetic resonance imaging, and ultrasound studies.19,121,122
Management
Decisions regarding the necessity and timeliness of removal of a foreign body are based on the size and the reactivity of the foreign body, proximity to vital structures, degree of wound contamination, and presence or absence of symptoms.19 Foreign bodies that cause continued pain, interfere with hand function because of their size or their position, or cause local or systemic toxicity (e.g., paints or mercury) should be removed. In removing foreign bodies, traction should be applied along the long axis of the foreign body in order to allow easier extraction, as well as to avoid breakage into two or more pieces. With foreign bodies associated with fractures, prompt surgical débridement is necessary to prevent osteomyelitis.123 Wounds that are grossly contaminated with soil or organic material require immediate removal of the foreign body, débridement, and irrigation. Foreign bodies near tendons, nerves, and vessels and foreign bodies causing ischemia or hemorrhage require cautious removal under optimal conditions.
References
1. Overton, DT, Uehara, DT. Evaluation of the injured hand. Emerg Med Clin North Am. 1993;11:585.
2. Atroshi, I, Rosenberg, H. Epidemiology of amputations and severe injuries of the hand. Hand Clin. 2001;17:343.
3. Altman, RS, Harris, GD, Knuth, CJ. Initial management of hand injuries in the emergency patient. Am J Emerg Med. 1987;5:400.
4. Chung, K, Spilson, S. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26:908.
5. Sorock, G, et al. Acute traumatic occupational hand injuries: Type, location, and severity. J Occup Environ Med. 2002;44:345.
6. Pratt, NE. Anatomy and kinesiology of the hand. In: Skirven TM, ed. Rehabilitation of the Hand and Upper Extremity. 6th ed. Philadelphia: Mosby; 2011:3–17.
7. Belliappa, PP, Scheker, LR. Functional anatomy of the hand. Emerg Med Clin North Am. 1993;11:557.
8. Kozin, SH, Waters, PM. Fractures and dislocations of the hand and carpus in children. In: Beaty JH, Kasser JR, eds. Rockwood and Wilkins Fractures in Children. 7th ed. Philadelphia: Lippincott: Williams & Wilkins; 2010:225–291.
9. Hodgkinson, DW, Kurdy, N, Nicholson, DA, Driscoll, PA. The hand: ABC of emergency radiology. BMJ. 1994;308:401.
10. Froment, J. La préhension dans les paralysies du nerf cubital et le signe du pouce. Presse Med. 1915;23:409.
11. Wright, PE, Flexor and extensor tendon injuries, Campbell’s Operative Orthopaedics. 11th ed. Canale, ST, Beaty, JH, eds., Campbell’s Operative Orthopaedics. St Louis:Mosby; 2008;vol 4.
12. Kanavel, AB. Infections of the Hand, 6th ed. Philadelphia: Lea & Febiger; 1993.
13. Koman, LA, et al. Vascular disorders. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, eds. Green’s Operative Hand Surgery. 6th ed. Philadelphia: Churchill Livingstone; 2011:2197.
13a. Luczak, BP, et al. Closed digital artery injury. Ochsner J. 2011;11:139–142.
13b. Al-Qattan, MM. Phalangeal neck fractures with concomitant vascular injury. J Hand Surg Eur Vol. 2009;34:104–109.
14. Lundborg, G, Rosen, B. The two-point discrimination test—time for a reappraisal? J Hand Surg Br. 2004;29:418.
15. Tindall, A, Dawood, R, Povlsen, B. The skin wrinkle test: A simple nerve injury test for paediatric and uncooperative patients. Emerg Med J. 2006;23:883.
16. Zook, EG. Reconstruction of a functional and aesthetic nail. Hand Clin. 2002;18:577.
17. Henry, MH. Hand fractures and dislocations. In: Bucholz RW, et al, eds. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia: Lippincott: Williams & Wilkins; 2010:710.
18. Wilks, M, Meldon, S. The hand. In: Schwartz DT, Reisdorff EJ, eds. Emergency Radiology. New York: McGraw-Hill, 2000.
19. Stone, DB, Levine, MR. Foreign body removal. In: Roberts JR, Hedges JR, eds. Clinical Procedures in Emergency Medicine. Philadelphia: Saunders, 2009.
20. De Jonge, JJ, Kingma, J, van der Lei, B, Klasen, HJ. Phalangeal fractures of the hand: An analysis of gender and age-related incidence and aetiology. J Hand Surg Br. 1994;19:168.
21. Simon, RR, Sherman, SC, Koenigsknecht, SJ. Emergency Orthopedics: The Extremities, 5th ed. New York: McGraw-Hill; 2007.
22. DaCruz, DJ, Slade, RJ, Malone, W. Fractures of the distal phalanges. J Hand Surg Br. 1988;13:350.
23. Freeland, AE, Lindley, SG. Malunions of the finger metacarpals and phalanges. Hand Clin. 2006;22:341.
24. Wayne, PH. Radiology of the occupationally injured hand. Hand Clin. 1986;2:467.
25. Stern, PJ, Roman, RJ, Kiefhaber, TR, McDonough, JJ. Pilon fractures of the proximal interphalangeal joint. J Hand Surg Am. 1991;16:844.
26. Stapczynski, JS. Fracture of the base of the little finger metacarpal: Importance of the “ball-catcher” radiographic view. J Emerg Med. 1991;9:145.
27. Light, TR, Bednar, MS. Management of intra-articular fractures of the metacarpophalangeal joint. Hand Clin. 1994;10:303.
28. Talan, DA, et al. Clinical presentation and bacteriologic analysis of infected human bites in patients presenting to emergency departments. Clin Infect Dis. 2003;37:1481.
29. Wolfe, SW, Dick, HM. Articular fractures of the hand: Part I. Guidelines for assessment. Orthop Rev. 1991;20:27.
30. McLain, RF, Steyers, C, Stoddard, M. Infections in open fractures of the hand. J Hand Surg Am. 1991;16:108.
31. Lee, SG, Jupiter, JB. Phalangeal and metacarpal fractures of the hand. Hand Clin. 2000;16:323.
32. Peterson, JJ, Bancroft, LW. Injuries of the fingers and thumb in the athlete. Clin Sports Med. 2006;25:527.
33. Soyer, AD. Fractures of the base of the first metacarpal: Current treatment options. J Am Acad Orthop Surg. 1999;7:403.
34. Foster, RJ, Hastings, H, II. Treatment of Bennett, Rolando, and vertical intraarticular trapezial fractures. Clin Orthop Relat Res. 1987;214:121.
35. Landin, LA. Epidemiology of children’s fractures. J Pediatr Orthop B. 1997;6:79.
36. Papadonikolakis, A, Li, Z, Smith, BP, Koman, LA. Fractures of the phalanges and interphalangeal joints in children. Hand Clin. 2006;22:11.
37. Della-Guistina, K, Della-Guistina, DA. Emergency department evaluation and treatment of pediatric orthopedic injuries. Emerg Med Clin North Am. 1999;17:895.
38. Salter, RB, Harris, WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 1963;45:587.
39. Vadivelu, R, Dias, JJ, Burke, FD, Stanton, J. Hand injuries in children. J Pediatr Orthop. 2006;26:29.
40. Mahabir, RC, Kazemi, AR, Cannon, WG, Courtemanche, DJ. Pediatric hand fractures: A review. Pediatr Emerg Care. 2001;17:153.
41. Stahl, S, Jupitur, JB. Salter-Harris types III and IV epiphyseal fractures in the hand treated with tension-band wiring. J Pediatr Orthop. 1999;19:233.
42. Clark, DP, Scott, RN, Anderson, IWR. Hand problems in an accident and emergency department. J Hand Surg. 1985;10:297.
43. Musharafieh, RS, Bassim, YR, Atiyeh, BS. Ulnar collateral ligament rupture of the first metacarpophalangeal joint: A frequently missed injury in the emergency department. J Emerg Med. 1997;15:193.
44. Merrell, G, Slade, JF. Dislocations and ligament injuries in the digits. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, eds. Green’s Operative Hand Surgery. 6th ed. Philadelphia: Churchill Livingstone; 2011:291.
45. Kahler, D, McCue, F. Metacarpophalangeal and proximal interphalangeal joint injuries of the hand, including the thumb. Clin Sports Med. 1992;11:57.
46. Kiefhaber, TR, Stern, PH, Grood, ES. Lateral stability of the proximal interphalangeal joint. J Hand Surg Am. 1986;11:661.
47. Wilson, RL, Liechty, BW. Complications following small joint injuries. Hand Clin. 1986;2:329.
48. Henderson, JJ, Arafa, MA. Carpometacarpal dislocation: An easily missed diagnosis. J Bone Joint Surg Br. 1987;69:212.
49. Gurland, M. Carpometacarpal joint injuries of the fingers. Hand Clin. 1992;8:733.
50. Campbell, CS. Gamekeeper’s thumb. J Bone Joint Surg Br. 1955;37:148.
51. Gerber, C, Senn, E, Matter, P. Skier’s thumb. Surgical treatment of recent injuries to the ulnar collateral ligament of the metacarpophalangeal joint. Am J Sports Med. 1981;9:171.
52. Edelstein, DM, Kardashian, G, Lee, SK. Radial collateral ligaments injuries of the thumb. J Hand Surg Am. 2008;33:760.
53. Stener, B. Displacement of the ruptured ulnar collateral ligament of the metacarpophalangeal joint of the thumb. J Bone Joint Surg. 1962;44:869.
54. Tang, P. Collateral ligament injuries of the thumb metacarpophalangeal joint. J Am Acad Orthop Surg. 2011;19:287.
55. Patel, S, Potty, A, Taylor, EJ, Sorene, ED. Collateral ligament injuries of the metacarpophalangeal joint of the thumb: A treatment algorithm. Strategies Trauma Limb Reconstr. 2010;5:1.
56. Heyman, P. Injuries to the ulnar collateral ligament of the thumb: Metacarpophalangeal joint. J Am Acad Orthop Surg. 1997;5:224.
57. Chuter, GS, Muwanga, CL, Irwin, LR. Ulnar collateral ligament injuries of the thumb: 10 years of surgical experience. Injury. 2009;40:652.
58. Doty, JF, Rudd, JN, Jemison, M. Radial collateral ligament injury of the thumb with a Stener-like lesion. Orthopedics. 2010;33:925.
59. Bosmans, B, Verhofstad, MH, Gosens, T. Traumatic thumb carpometacarpal joint dislocations. J Hand Surg Am. 2008;33:438.
60. Strauch, RJ. Extensor tendon injury. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, eds. Green’s Operative Hand Surgery. 6th ed. Philadelphia: Churchill Livingstone; 2011:159.
61. Pyne, JI, Adams, BD. Hand tendon injuries in athletics. Clin Sports Med. 1992;11:833.
62. Hanz, KR, Saint-Cyr, M, Semmler, MJ, Rohrich, RJ. Extensor tendon injuries: Acute management and secondary reconstruction. Plast Reconstr Surg. 2008;121:109e.
63. Rayan, GM, Mullins, PT. Skin necrosis complicating mallet finger splinting and vascularity of the distal interphalangeal joint overlying skin. J Hand Surg Am. 1987;12:548.
64. Geyman, JP, Fink, K, Sullivan, SD. Conservative versus surgical treatment of mallet finger: A pooled quantitative literature evaluation. J Am Board Fam Pract. 1998;11:382.
65. Elson, RA. Rupture of the central slip of the extensor hood of the finger. A test for early diagnosis. J Bone Joint Surg Br. 1986;68:229.
66. Bynum, DK, Gilbert, JA. Avulsion of the flexor digitorum profundus: Anatomic and biomechanical considerations. J Hand Surg. 1988;13A:222.
67. Murphy, BA, Mass, DP. Zone I flexor tendon injuries. Hand Clin. 2005;21:167.
68. Ablove, RH, Moy, OJ, Peimer, CA. Pediatric hand disease diagnosis and treatment. Pediatr Clin North Am. 1998;45:1507.
69. Seiler, JG, III. Flexor tendon injury: Acute injuries. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, eds. Green’s Operative Hand Surgery. 6th ed. Philadelphia: Churchill Livingstone; 2011:189.
70. Taras, JS, Kaufmann, RA. Flexor tendon injury: Flexor tendon reconstruction. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, eds. Green’s Operative Hand Surgery. 6th ed. Philadelphia: Churchill Livingstone; 2011:207.
71. O’Hara, JJ, Stone, JH. An intratendinous epidermoid cyst after trauma. J Hand Surg Am. 1990;15:477.
72. Geissler, GA, Erdmann, D, Germann, G. Soft tissue coverage in devastating hand injuries. Hand Clin. 2003;19:63.
73. Hammig, B, Jones, C. Injuries related to snow blowers in the United States: 2002 through 2008. Acad Emerg Med. 2010;17:566.
74. Chin, G, Weinzweig, N, Weinzweig, J, Geldner, P, Gonzalez, M. Snowblower injuries to the hand. Ann Plast Surg. 1998;41:390.
75. Arellano, A, Wegener, E, Freeland, A. Mutilating injuries to the hand: Early amputation or repair and reconstruction? Orthopedics. 1999;22:683.
76. Buncke, G, Buntic, R, Romeo, O. Pediatric mutilating hand injuries. Hand Clin. 2003;19:121.
77. Jebson, PJ, Louis, DS, Bagg, M. Amputations. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, eds. Green’s Operative Hand Surgery. 6th ed. Philadelphia: Churchill Livingstone; 2011:1885.
78. Dautel, G, Barbary, S. Mini replants: Fingertip replant distal to the IP or DIP joint. J Plast Reconstr Aesthet Surg. 2007;60:811.
79. Sommer, NZ, Brown, RE. The perionychium. In: Wolfe SW, ed. Green’s Operative Hand Surgery. 6th ed. Philadelphia: Elsevier Churchill Livingstone; 2011:333.
80. Simon, RR, Wolgin, M. Subungual hematoma: Association with occult laceration requiring repair. Am J Emerg Med. 1987;5:302–304.
81. Meek, S, White, M. Subungual hematomas: Is simple trephining enough? J Accid Emerg Med. 1998;15:269.
82. Seaberg, DC, Angelos, WJ, Paris, PM. Treatment of subungual hematomas with nail trephination: A prospective study. Am J Emerg Med. 1991;9:209.
83. Roser, SE, Gellman, H. Comparison of nail bed repair versus nail trephination for subungual hematomas in children. J Hand Surg Am. 1999;24:1166.
84. Shepard, G. Perionychial grafts in trauma and reconstruction. Hand Clin. 2002;18:595.
85. Perron, A, Miller, M, Brady, W. Orthopedic pitfalls in the ED: Fight bite. Am J Emerg Med. 2002;20:114.
86. Bekler, H, Gokce, A, Beyzadeoglu, T, Parmaksizoglu, F. The surgical treatment and outcomes of high-pressure injection injuries of the hand. J Hand Surg Br. 2007;32:394.
87. Neal, NC, Burke, FD. High-pressure injection injuries. Injury. 1991;22:467.
88. Hogan, CJ, Ruland, RT. High-pressure injection injuries to the upper extremity: A review of the literature. J Orthop Trauma. 2006;20:503.
89. Wong, TC, Ip, FK, Wu, WC. High-pressure injection injuries of the hand in a Chinese population. J Hand Surg Br. 2005;30:588.
90. Lewis, HG, Clarke, P, Kneafsey, B, Brennen, MD. A 10-year review of high-pressure injection injuries to the hand. J Hand Surg Br. 1998;23:479.
91. Kay, S, Werntz, J, Wolff, TW. Ring avulsion injuries: Classification and prognosis. J Hand Surg Am. 1989;14:204.
92. Baek, SM, Kim, SS. Successful digital replantation after 42 hours of warm ischemia. J Reconstr Microsurg. 1992;8:455.
93. Morrison, WA, McCombe, D. Digital replantation. Hand Clin. 2007;23:1.
94. Neumeister, M, Brown, R. Mutilating hand injuries: Principles and management. Hand Clin. 2003;19:1.
95. Gulgonen, A, Ozer, K. Compartment syndrome. In: Wolfe SW, ed. Green’s Operative Hand Surgery. 6th ed. Philadelphia: Elsevier Churchill Livingstone; 2011:1929.
96. Isaacs, J. Treatment of acute peripheral nerve injuries: Current concepts. J Hand Surg. 2010;35A:291.
97. Harrison, BP, Hilliard, MW. Emergency department evaluation and treatment of hand injuries. Emerg Med Clin North Am. 1999;17:793.
98. Jebson, PJ. Infections of the fingertip: Paronychias and felons. Hand Clin. 1998;14:547.
99. Brook, I. Bacteriologic study of paronychia in children. Am J Surg. 1981;141:703.
100. Wright, PE, Hand infections, Campbell’s Operative Orthopaedics. 11th ed. Canale, ST, Beaty, JH, eds., Campbell’s Operative Orthopaedics. St Louis:Mosby; 2008;vol 4.
101. Kilgore, ES, Jr., Brown, LG, Newmeyer, WL, Graham, WP, 3rd., Davis, TS. Treatment of felons. Am J Surg. 1975;130:194.
102. Wu, IB, Schwartz, RA. Herpetic whitlow. Cutis. 2007;79:193.
103. Gill, MJ, Arlette, J, Buchan, K. Herpes simplex virus infection of hand: A profile of 79 cases. Am J Med. 1988;84:89.
104. Mann, RJ, Hoffeld, TA, Farmer, CB. Human bites of the hand: Twenty years of experience. J Hand Surg Am. 1985;2:97.
105. Habif, TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy, 4th ed. Edinburgh: Mosby/Elsevier; 2010.
106. Small, LN, Ross, JJ. Suppurative tenosynovitis and septic bursitis. Infect Dis Clin North Am. 2005;19:991.
107. Garcia-De La Torre, I, Nava-Zavala, A. Gonococcal and nongonococcal arthritis. Rheum Dis Clin North Am. 2009;35:63–73.
108. Stevanovic, MV, Sharpe, F. Acute infections of the hand. In: Wolfe SW, ed. Green’s Operative Hand Surgery. 6th ed. Philadelphia: Elsevier Churchill Livingstone; 2011:41.
109. Jebson, PJ. Deep subfascial space infections. Hand Clin. 1998;14:557.
110. Wilson, PC, Rinker, B. The incidence of methicillin-resistant Staphylococcus aureus in community-acquired hand infections. Ann Plast Surg. 2009;62:513.
111. Murray, PM. Septic arthritis of the hand and wrist. Hand Clin. 1998;14:579.
112. Weinzweig, N, Gonzalez, M. Surgical infections of the hand and upper extremity: A county hospital experience. Ann Plast Surg. 2002;49:621.
113. Reference deleted in proofs.
114. McLario, DJ, Burton, LJ, Bruce, RW, Whipple, TJ, Simon, HK. Pseudoparalysis of the lower extremity in an infant. Pediatr Emerg Care. 1998;14:277.
115. Nimigan, AS, Ross, DC, Gan, BS. Steroid injections in the management of trigger fingers. Am J Phys Med Rehabil. 2006;85:36.
116. Saunders, S, Longworth, S. Injection Techniques in Orthopaedics and Sports Medicine. Edinburgh: Churchill Livingstone; 2006.
117. Peters-Veluthamaningal, C, van der Windt, DA, Winters, JC, Meyboom-de Jong, B. Corticosteroid injection for trigger finger in adults. Cochrane Database Syst Rev. 1, 2009.
118. Zyluk, A, Jagielski, G. Percutaneous A1 pulley release vs steroid injection for trigger digit: The results of a prospective, randomized trial. J Hand Surg Eur Vol. 2011;36:53.
119. Abe, Y, Watson, HK, Renaud, S. Flexor tendon sheath ganglion: Analysis of 128 cases. Hand Surg. 2004;9:1.
120. Steele, MT, Tran, LV, Watson, WA, Muelleman, RL. Retained glass foreign bodies in wounds. Am J Emerg Med. 1998;16:627.
121. Blankenship, RB, Baker, T. Imaging modalities in wounds and superficial skin infections. Emerg Med Clin North Am. 2007;25:223.
122. Allen, GM, Drakonaki, EE, Tan, ML, Dhillon, M, Rajaratnam, V. High resolution ultrasound in the diagnosis of upper limb disorders: A tertiary referral centre experience. Ann Plast Surg. 2008;61:259.
123. Stein, F. Foreign body injuries of the hand. Emerg Med Clin North Am. 1985;3:383.